 by Karen Parker Davidson, DHA, MSA, MEd, MSN, ARPN
by Karen Parker Davidson, DHA, MSA, MEd, MSN, ARPN
Can you trust what the patient tells you? The topic of discussion at meetings has moved from sleep disorders to breathing disorders and now to nasal resistance. Subjective assessments like patient directed questionnaires have been a validated form of understanding what motivates the patient to seek out healthcare providers from primary care to dentists. Although patient directed forms and questionnaires paint a picture of health or disease, quantifiable numeric data provides a clearer view of patient conditions. We see this in such technologies as CBCT, MRI, and the increasingly common non-invasive technologies used in offices across the country. While there is a helpful emotional component in patient directed tools, objective measurements have added value to direct better care and outcomes. Let’s set the record straight about what they are, how they are used, and the value they bring.
Why Haven’t You Heard about Using Objective Measurements?
Objective measurements have been developed to become validated, standardized tools for screening and quantifying patient complaints. The concepts have been around since 1894; in 1958, Semarak described the first “Nasal Patency Assessment Device” that enabled simultaneous assessment of nasal respiratory flow and pressure difference between the nasal entrance and choanae. In 1968, Dr. Cottle, whom we all know by the “Cottle Maneuver”, introduced rhinomanometry to clinical rhinology. To further extend the history, Dr. Christian Guilleminault looked at maxillary expansion and rhinometry in 2004. Nasal resistance was part of several of his studies for AHI correlations and proper identification of patients for various therapies, including DOME and CPAP intolerance, as far back as 2012.1-3
These measurement devices, ranging in retail price from $63-$38,000, are used to measure the pressure-flow relationship in nasal breathing, the location of obstructions, and the extent obstructions and nasal breathing are disrupted in adults, children, and even small animals pre, mid, and post treatment or therapy. It is a common opinion across all specialties that nasal flow limitations cause nasal obstructions resulting in a sequela of events to include TMD, postural problems, an increase in the Hypopnea/Apnea ratios, and sleep disordered breathing. Many of these clinical presentations lead to a hypoventilative state and obstructive sleep apnea (OSA) if left untreated. Objective measurement technologies have been on the market for more than 20 years and published in over two thousand medical and dental journal articles; however, they may be misunderstood in their function, theory, and application. The purpose of this review is to discuss each type of measurement tool, where it is most useful in the clinical workflow, and the effect it can have on blurring the line between medicine and dentistry.

Acoustic Rhinometry
Acoustic Rhinometry was validated as a tool for geometric measurements in 1989 by Hilberg et al., and first came to market in 1993 by Hood Laboratories (K921452), later purchased by Sleep Group Solutions (SGS), followed by GM Instruments, Ltd. (K972140) in 1998.4 To date, these are the only two manufacturers with FDA approved devices that measure the cross-sectional area of the nasal passages to assess static volume and anatomical landmarks. While the patient holds their breath, the acoustic pulse sound waves are generated from a speaker or spark source, travels through the nose reflecting from the mucosal surface, picked up by the microphone in the sound tube, back to amplifier, and to the measurement software for interpretation. Two landmarks in the measurement are minimal crossectional area, MCA, or crossectional area, CSA1, at the internal nasal valve (INV) and MCA or CSA2 at the inferior head of the anterior turbinate. The main advantage is that this is a noninvasive and quick test, depending on the brand and company technology, and can be done in an office, OR, or hospital. The disadvantage is the accuracy is dependent on the interface of the nose and equipment by way of the shape of the nosepiece, (round versus anatomical), and positioning of the tube.
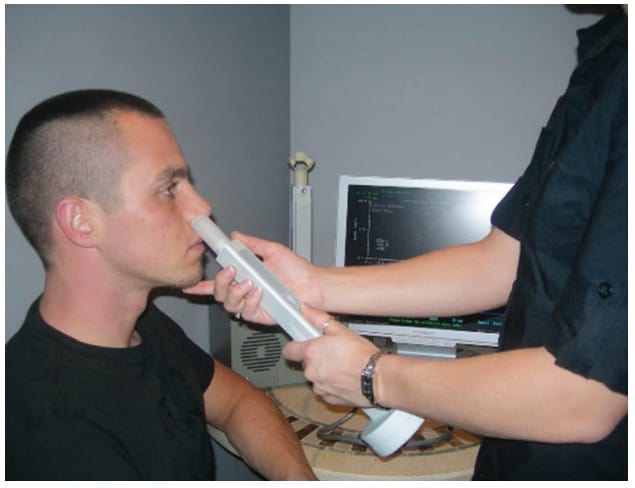
(Sleep Group Solutions)
Rhinomanometry
Rhinomanometry, unlike rhinometry, is a form of manometry that uses pressure and flow sources from a transducer box to objectivly measurement nasal function by the intranasal pressure and the rate of airflow during active breathing. Four-phase anterior and posterior rhinomanometry (GM Instruments, Ltd.), FDA approved in 1990, (K902120) is the only non-invasve, parameter-based technology for measuring nasal function in the sitting and supine postions. In 2010, the Standardization Committee on the Objective Measurement of the Upper Airway published 4-Phase-Rhinomanometry Basics and Practices in the Supplement of Rhinology. In 2015, the Committee updated the standards of practice to declare classic, non 4 phase, rhinomanometry obsolete and confirmed subjective symptoms comparable and compatible to 4-phase rhinomanometry.5 The first measurements of nasal flow limitations were taken in 1894 with the use of a refrigerator plate to measure the amount of vapor in exhaled air, the first rhinomanometer did not become computerized until 1970. Over time, transnasal pressures and the correlation to OSA and disease progression have been studied as many in the medical field find AHI losing relevance as the primary diagnostic metric of OSA.6,7
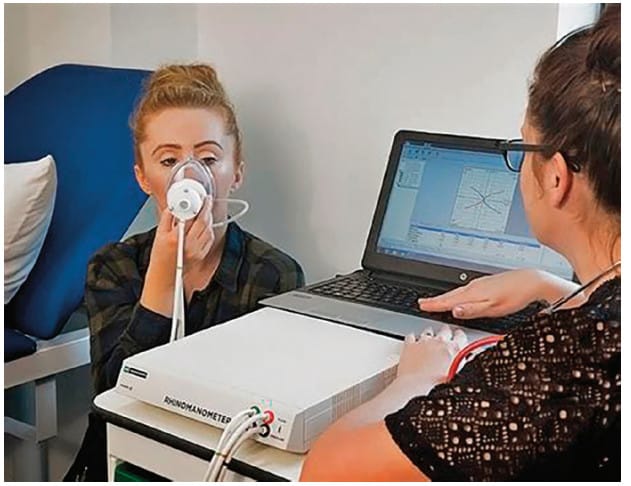
(GM Instruments)
Pharyngometry
Pharyngometry, much like rhinometry, uses sound pulse waves to measure the geometric area of the nasopharyngeal airway down to the glottis, resulting in static measurements. Most commonly known as Ecco-vision, it came to market in 2002 by E. Benson Hood Laboratories (K011329) then aquired by SGS soon thereafter. Popular in ENT for voice and laryngeal cases, it has made its way to the dental market as a tool for measuring the airway and positioning the mandible for oral appliance therapy. Although it may be a screening tool for OSA based on the Starling resistor model and volumetric measurements, it does not correlate to collapsability, which is based on a pressure-flow relationship. Furthermore, clinical observations and studies suggest that anatomical factors alone do not cause OSA.

(Sleep Group Solutions)
Peak Nasal Inspiratory Flow
PNIF, Peak Nasal Inspiratory Flow Meter, is the most cost-effective device for measuring nasal inspiratory function only. The device is provided to the patient to take home to self-assess nasal airflow. The PNIF meter can be utilized to rapidly assess the patency of the nose. It utilizes a variable diameter tube adjusted in liters/minute alongside a low inertia marker ring, whose position after an inspiratory maneuver shows the greatest flow accomplished. Precise measurements are Plus/Minus 10% of the reading or 10 L/min flow (whichever is the more prominent), with repeatability of plus/minus 5%. Product life expectancy with typical utilization is to stay operational for two years and is a great option for patient follow-up, using telehealth.

(PNIF) Meter (GM Instruments)
How Do I Integrate These Technologies into My Clinical Practice and Workflow?
By understanding the indication and theory behind each technology, dentists and medical professionals who specialize in airway can add them as a screening and treatment assessment tool for therapy identification and improvement at various endpoints. It is equally important to understand that none of them are used to diagnose airway problems or OSA, but correlate to breathing problems that progress to hypoventilation or OSA. For example, breathing during acoustic pulse sound wave measurements can cause a testing error as noncartilaginous tissue will vibrate during active breathing. Positional and postural changes also cause errors in testing, too. Any volumetric change caused by forward head posture, C-spine lesions, shoulder injuries, or spinal injuries, to name a few, will affect a pharygnometry reading by mimicing a smaller airway. The same holds true with rhinomanometry and nasal function measurements during breathing. If the test is not measured in the natural state or with the head over the shoulders, what was once a normative mean resitance value can increase with postural changes, mimicing high resistance that may indicate a problem that was not clinically present. Additionally, in testing, recumbent positions affect nasal resistance and airflow limitations – important considerations in snorers and sleep apnea patients.
It is evident based on a number of studies that nasal resistance is an undervalued and overlooked biosignal that affects maxillary growth in children and the mandible position in children and adults. Essentially, nasal resistance data has given the sleep and airway community something to talk about.
Each of the these objective measurement devices, proven with validation, specificity, and senstivity studies, has potential value as an assessement tool in trained provider’s hands. Dental practices can develop improved clinical workflow by quantifying therapy selection and outcomes. Measuring airflow can be an additional reimbursable revenue stream for a mutually beneficial experience between the doctor and patient.
- Pirelli P, Saponara M, Guilleminault C. Rapid maxillary expansion in children with obstructive sleep apnea syndrome. 2004;27(4):761-766. doi:10.1093/sleep/27.4.76
- Iwasaki T, Yoon A, Guilleminault C, Yamasaki Y, Liu SY. How does distraction osteogenesis maxillary expansion (DOME) reduce severity of obstructive sleep apnea? Sleep Breath. 2020;24(1):287-296. doi:10.1007/s11325-019-01948-7
- Toh ST, Lin CH, Guilleminault C. Usage of four-phase high-resolution rhinomanometry and measurement of nasal resistance in sleep-disordered breathing. 2012;122(10):2343-2349. doi:10.1002/lary.2344
- Hilberg O, Jackson AC, Swift DL, Pedersen OF. Acoustic rhinometry: evaluation of nasal cavity geometry by acoustic reflection. J Appl Physiol (1985). 1989;66(1):295-303. doi:10.1152/jappl.1989.66.1.295
- Vogt K, Wernecke KD, Behrbohm H, Gubisch W, Argale M. Four-phase rhinomanometry: a multicentric retrospective analysis of 36,563 clinical measurements. Eur Arch Otorhinolaryngol. 2016;273(5):1185-1198. doi:10.1007/s00405-015-3723-5
- Pevernagie DA, Gnidovec-Strazisar B, Grote L, et al. On the rise and fall of the apnea-hypopnea index: A historical review and critical appraisal. J Sleep Res. 2020;29(4):e13066. doi:10.1111/jsr.13066
- Hoel HC, Kvinnesland K, Berg S. Impact of nasal resistance on the distribution of apneas and hypopneas in obstructive sleep apnea. Sleep Med. 2020;71:83-88. doi:10.1016/j.sleep.2020.03.024


 Karen Parker Davidson, DHA, MSA, MEd., MSN, ARPN, for over two decades has held many positions in the medical device industry in the ENT and Sleep markets, in addition to thirty years of clinical experience to include service as a Critical Care Nurse and Flight Nurse in the US Air Force Reserves. Dr. Davidson is adjunct faculty at Liberty University and Central Michigan University, founder of FACT Healthcare Consulting Group, and creator of the patent pending DAFNE Score System to guide and educate healthcare providers the values of objective nasal function and treatment options and improvements based on the readings. She is published in medical journals discussing airway disorders, a coauthor of “The Power of the Tongue In the Beginning, We Were All Tongue Tie” and “Sleep Apnea and Pregnancy: The Female Response to Sleep Breathing Disorders”, a contributing author to “Growing Into Breathing Problems: The Quest for Collaborative Life Time Solutions” and “Health Informatics and Patient Safety in Times of Crisis”, and the author of an upcoming book, “Breathe Through Your Nose, Don’t Pay Through It: The Impact the Healthcare Industry has on Nasal Function and How We Breathe”.
Karen Parker Davidson, DHA, MSA, MEd., MSN, ARPN, for over two decades has held many positions in the medical device industry in the ENT and Sleep markets, in addition to thirty years of clinical experience to include service as a Critical Care Nurse and Flight Nurse in the US Air Force Reserves. Dr. Davidson is adjunct faculty at Liberty University and Central Michigan University, founder of FACT Healthcare Consulting Group, and creator of the patent pending DAFNE Score System to guide and educate healthcare providers the values of objective nasal function and treatment options and improvements based on the readings. She is published in medical journals discussing airway disorders, a coauthor of “The Power of the Tongue In the Beginning, We Were All Tongue Tie” and “Sleep Apnea and Pregnancy: The Female Response to Sleep Breathing Disorders”, a contributing author to “Growing Into Breathing Problems: The Quest for Collaborative Life Time Solutions” and “Health Informatics and Patient Safety in Times of Crisis”, and the author of an upcoming book, “Breathe Through Your Nose, Don’t Pay Through It: The Impact the Healthcare Industry has on Nasal Function and How We Breathe”.