
A Case Report, part 2
by Juan-Carlos Quintero, DMD, MS
Previously we discussed the correlation between dento-facial patterns and pharyngeal airway measurements as a risk factor for obstructive sleep apnea (OSA). All dentists should understand these relationships and be in tune with the role 3D imaging plays in the screening for patients at risk for OSA. Dentists are often in a unique position, compared to our medical peers, to screen for and triage patients, particularly children suffering from OSA because of our understanding of the mouth and jaws.
 Breathing is a function of craniofacial anatomy, so ensuring proper facial growth & development and the paralleled development of patent airways is an absolute mandate for any dentist who sees children. Recent imaging technology advances in the form of ultralow dose cone beam computerized tomography (CBCT), such as the new i-CAT FLX (Imaging Sciences International), have made everyday imaging of airways possible with dose exposure less than a panorex and as low as 8 µSv. The application and implication of this technology in the screening and prevention of OSA in the pediatric population are enormous. It is now possible to readily and safely screen for children with small airways who either have OSA, are at risk for OSA, or are at risk for developing OSA later in life and intervene. The following is a case study demonstrating the importance of early detection and treatment.
Breathing is a function of craniofacial anatomy, so ensuring proper facial growth & development and the paralleled development of patent airways is an absolute mandate for any dentist who sees children. Recent imaging technology advances in the form of ultralow dose cone beam computerized tomography (CBCT), such as the new i-CAT FLX (Imaging Sciences International), have made everyday imaging of airways possible with dose exposure less than a panorex and as low as 8 µSv. The application and implication of this technology in the screening and prevention of OSA in the pediatric population are enormous. It is now possible to readily and safely screen for children with small airways who either have OSA, are at risk for OSA, or are at risk for developing OSA later in life and intervene. The following is a case study demonstrating the importance of early detection and treatment.
Case Report
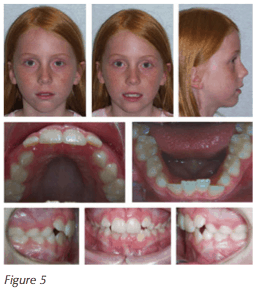
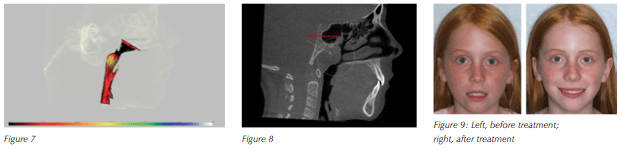
An 8-year-old female patient presented for an orthodontic evaluation with a chief concern of “wanting a prettier smile.” During the initial interview, it was revealed that the patient was a chronic mouth breather, and a regular snorer. The parents also reported a lethargic disposition during the day with inattentiveness at school and disinterest in sports. At the time of the exam, the patient appeared to be breathing only through her mouth and had signs of venous pooling (“droopy eyes”). A narrow smile and a constricted maxilla was noted. A 3D diagnostic session was completed consisting of photographs (Figure 5) and a low-dose CBCT taken on an i-CAT machine using 16×13 cm field of view and a 4.9-second exposure time. The evaluation revealed crowding with impacted maxillary canines in the mixed dentition, with a constricted arch form (Figure 6). The CBCT radiographic study showed an extremely narrow pharyngeal airway with a minimum cross-sectional airway (MCA) of 47 mm2 (Figure 7). The patient also presented with adenoid hyperplasia encroaching upon the pharyngeal airspace (Figure 8).
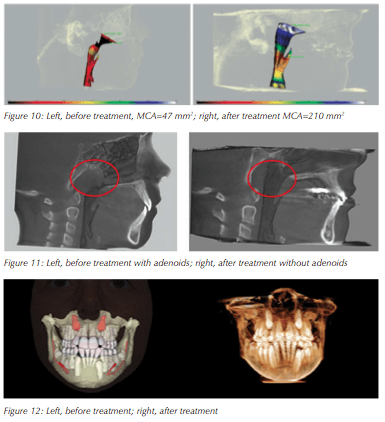 The treatment plan consisted first of ENT management in the form of adenoidectomy with coblation of turbinates followed by 10 months of orthodontic Phase I dual arch expansion treatment. Specifically, the patient received a Rapid Maxillary Expander off of a 2x 6 bracket system in the upper arch and a lower removable Schwartz expander followed by a 2X6 bracket system. Final Phase I records were taken consisting of photographs and a low dose CBCT. Figure 9 shows the facial changes before and after treatment, 12 months apart. Figures 10 and 11 show the changes in the pharyngeal airway volume and cross- sectional areas following adenoidectomy, coblation of turbinates, and Phase I orthodontic expansion. Figure 12 shows the resolution of the ectopically positioned permanent maxillary canines. Note the more upright and vertical positions of the canines.
The treatment plan consisted first of ENT management in the form of adenoidectomy with coblation of turbinates followed by 10 months of orthodontic Phase I dual arch expansion treatment. Specifically, the patient received a Rapid Maxillary Expander off of a 2x 6 bracket system in the upper arch and a lower removable Schwartz expander followed by a 2X6 bracket system. Final Phase I records were taken consisting of photographs and a low dose CBCT. Figure 9 shows the facial changes before and after treatment, 12 months apart. Figures 10 and 11 show the changes in the pharyngeal airway volume and cross- sectional areas following adenoidectomy, coblation of turbinates, and Phase I orthodontic expansion. Figure 12 shows the resolution of the ectopically positioned permanent maxillary canines. Note the more upright and vertical positions of the canines.
 Post treatment, the mother reported a dramatic improvement in the patient’s overall health, level of alertness, a reduction in daytime sleepiness, an improvement in academic performance, and increased athletic activity — all signs of better sleep and oxygenation.
Post treatment, the mother reported a dramatic improvement in the patient’s overall health, level of alertness, a reduction in daytime sleepiness, an improvement in academic performance, and increased athletic activity — all signs of better sleep and oxygenation.
Conclusions
In children, airway issues must be identified and treated as early as possible. Delays in treatment can only delay the suffering of the family and the child. Proper screening using ultra-low-dose CBCT imaging and early management through inter-professional collaboration with ENTs, pediatricians, and allergists during the growing years of the face may prevent OSA in future generations by promoting healthy growth of the craniofacial complex, and thus pharyngeal airway development, during childhood.
A special thank you to the participating ENT on the case, Albert Fernandez, M.D. (Coral Gables, Florida).
Stay Relevant With Dental Sleep Practice
Join our email list for CE courses and webinars, articles and more..

