Illuminating medical conditions that often accompany sleep disordered breathing can help patients understand the necessity of treating the disease causing their conditions. The prevalence of comorbidities can help assess the risk of having sleep disordered breathing. Since many medical providers must collaborate to ensure complete patient care, increasing interdisciplinary communication will enhance the integration of patient care between providers. The term Integral Sleep Medicine is proffered.
The many faces of SDB are revealed by examining frequently associated conditions such as: High blood pressure (hypertension), heart failure, heart rhythm disturbances, atherosclerotic heart disease, pulmonary hypertension, and insulin resistance. Additionally, cognitive impairment (memory problems), depression, anxiety, and gastroesophageal reflux disease (GERD) are among possible complications of untreated sleep apnea. People are often motivated to seek information by a family pattern of early death. Discussing medical history with patients, dentists have excellent opportunities to screen community populations for SDB. Since treatment options include oral appliances, starting the conversation in the dental office provides patients important information as they pursue resolution of SDB. To help the dental team understand some of these SDB-Comorbidity connections, the following is a list of commonly quoted statistics:
- 1/3 of population suffers from some sleep disorders: 20M SDB, 10M Periodic Limb Movements, 20M Insomnia, snoring and other disorders.
- Snoring Prevalence 67% general population. “National Sleep Foundation” 2005
- 94% of OSA population snores, 6% are silent apneics.
- Studies show anywhere from 9% to 24% of the population have OSA (Wisconsin Study 1988, SHHS, Young) The mechanism of harm seems to be Intermittent Hypoxia.
- Metabolic Syndrome effects 24% of general population.
- Weight loss of 10% can decrease AHI 30%-50%.
- If 90% of affected people have not yet been diagnosed, approximately 20% of your patient population may be at risk of SDB. A risk assessment questionnaire can identify who should have diagnostic sleep testing (PSG).
- Categories have been broken out to facilitate inter-disciplinary dialogue.
 Category 1:
Category 1:
(some of the standard screening questions)
“STOPBANG” questionnaire: Snoring, Tired, Observed apneas, Pressure (BP), BMI, Age, Neck circumference, Gender)
- Physical: BMI, Sex, Age >50, Neck Size, Tonsil Grade, Oral Pharyngeal Crowding, Tongue level, Hyoid position, Craniofacial characteristics Orthodontic type, Palatal vaulting, Family History of SDB
- Have you had unexpected weight changes recently?
- Have you ever had a PSG? Titration study? Home sleep test?
- Do you snore loudly enough at night to cause conflict with others?
- Have you been told you have stopped breathing at night?
- Did you ever wake up choking?
- Do you awaken unrefreshed?
- Do you have morning headaches?
- Do you feel sleepy during the day? (Rely on Caffeine or Prescription Stimulants)
- Do you feel fatigued during the day?
- Do you have difficulty breathing through your nose? (Post nasal drip, or dry mouth in morning?)
Category 2: Cardiovascular:
- SDB predicts an increased prevalence of CAD, Stroke, Arrhythmias, Hypertension. Endothelial Dysfunction.
- SDB in CAD patients is twice that of non-CAD patients
- Increase in free radicals (oxidative stress), homocysteine and decrease in nitrous oxide leads to damaged endothelium and loss of vessel elasticity, resulting in hypertension.
- Stroke OR is 3x if AHI>30
- Within OSA population, 50% are hypertensive
- Within Hypertensive population, 30% have OSA
- Drug Resistant Hypertension, prevalence of OSA: 96% men, 65% women
- For Hypertensives whose BP doesn’t “dip” at night, 90% have OSA
- 38,000 CV deaths/year linked to OSA
- Heart Failure patients: 26%-37% have OSA and or CSA
- Severe OSA patients OR=5.2 for CV mortality
- Within Angina Population 54% had OSA
- Nocturia (2 or more events) or Enuresis, May result from diuretic hormone in response to respiratory event.
- Endothelial Dysfunction leads to Erectile Dysfunction.
- Within Erectile Dysfunction population, 44% have OSA
- Nocturnal Arrhythmias occur in 50% of OSA patients
- 68% of patients with atrioventricular block have OSA
- Ventricular Arrhythmias in 66% of OSA patients (PVCs)
- In Severe OSA cohort, risk of AFib is increased 4x
- In AFib cohort studies: 42% to 45% to 81% have OSA
- Patients with AFib may benefit from screening for OSA because OSA is a treatable risk factor for the initiation and recurrence of AFib after ablation.
- In Pacemaker patients, 59% have OSA.
Category 3: Pulmonary:
- In OSA population, 10%-20% have COPD
- COPD with OSA = “Overlap Syndrome” increased mortality
- OSA increases BP of Pulmonary Artery leads to Pulmonary Hypertension and possibly COPD
- COPD causes Nocturnal Oxygen Desats, impairs sleep, decreases SWS and REM
- 11% to 20% of those with controlled asthma reported sleep disturbances
- OSA patients have OR of 2.87 for asthma
- Asthma cohort has 72% inc. risk for developing OSA
- Each disorder makes the other worse
- In Asthma cohort, 70% have Rhinitis
Category 4: Gastroenterology:
- In Western countries, GERD symptoms such as heartburn and acid regurgitation occur in about 20% of adults.
- While the airway obstruction is superior to the junction of the larynx and the esophagus, each “event” will cause increased negative pressure in the esophagus which may create aspirations of stomach contents.
- In Nocturnal GERD pop, OR of having OSA is 2.97.
- In OSA pop, 24% have GERD.
- Morbid Consequences of GERD include: changes of cells lining the lower esophagus. About 10% of people with chronic symptoms of GERD develop Barrett’s esophagus which is a precursor to esophageal adenocarcinoma, a serious and potentially fatal cancer.
- In GERD cohort, TMJ disorders are twice as prevalent
- Patients with GERD have a significantly higher risk of concurrent asthma compared with patients without GERD.
- Neurological disorders with primary neurological symptoms are improved by treatment of comorbid OSA include: dementia, stroke, epilepsy and headache.
- Intermittent hypoxia in OSA is an independent risk factor for axonal damage of peripheral nerves.
- Strong association between OSA and peripheral neuropathy and retinopathy. (60% of patients with diabetes and OSA also have a peripheral neuropathy)
- SDB common in patients with many neuromuscular disorders.
- 30%-70% Alzheimer’s patients have SDB
- 20% Parkinson’s patients have OSA
- Within OSA patients, OR of developing Glaucoma within 5 years is 1.67
- OSA treatment shown to reduce frequency of cluster headache.
- RLS=8% in general population, 90% of these have PLMD
- RLS symptoms in 40% of subjects with iron and B12 deficiency
- Hyperhidrosis (night sweating), may be related to excessive body movement.
Category 6: Endocrinology:
- Diabetes prevalence in America is 8.3%. Prediabetes (>20 yr olds) 35%.
- Within Type 2 Diabetes population, 36%-50% have OSA.
- Menopause: Decrease in Estrogen and Progesterone leads to increase in SDB due to weight gain and decrease muscle tone. HRT may help.
- 24% of the general population has Metabolic Syndrome, a cluster of conditions ( increased blood pressure, a high blood sugar level, excess body fat around the waist, and abnormal cholesterol levels) that, when occurring in combination, increase your risk of heart disease, stroke and diabetes.
- In Metabolic Syndrome cohort, OR for MI is 2.63 compared with normals
- Metabolic Syndrome + OSA= Syndrome Z
- 70% of OSA patients are obese, so 30% aren’t obese.
- Within obese patient population, 30% have OSA.
- In Metabolic Syndrome Cohort, prevalence of mod-
- severe OSA is 60%
- In patients with OSA, prevalence of metabolic syndrome is 40% greater
- Narcolepsy is result of reduction of Hypocretin (orexin) and can be accompanied by: Cataplexy, Hypnogognic Hallucinations, Sleep Paralysis (SP), and Sudden Onset REM Sleep (SOREMS).
Category 7: Otolaryngology:
- Nasal congestion patients are 2x as likely to have OSA
- A variety of sinus problems are: Post nasal drip, sinusitis, nasal resistance, rhinitis, deviated septum, dry mouth upon awakening.
- Nasal congestion is independently associated with snoring frequency. (Wisconsin study 5000 patients)
- Allergic rhinitis increases risk of asthma 3x.
- Otological Symptoms 85% in TMD population (tinnitus 42%, ear pain 42%, dizziness 23% and diminished hearing 18%)
Category 8: Urology:
- In OSA population, between 40% and 60% have Erectile Dysfunction “ED”. Within ED population, 40% have OSA
- With increased severity of OSA, there is also increased occurrence of: overactive bladder, urgency incontinence.
- Sleep Fragmentation from SDB may decrease circulating antidiuretic hormone, which normally prevents us from urinating at night.
- OSA should be considered whenever a patient reports frequent awakenings from sleep to urinate, even when the symptom was previously attributed to the presence of BPH.
- Sleep Bruxism “SB” reported in 8% of general population, 87% in TMD population, 25% in OSA population.
- WIthin SB population, 30% have SDB
- Within SB population, 65% suffers from headaches (OR for headaches in SB is 4.3)
- Within OSA population, the OR to have SB is more than doubled
- Within OSA population, 25% have SB.
- In general population,12% have TMD.
- In OSA population, 25% have TMD.
- Within TMD population, 75% have chronic pain.
- Within TMD population, 30% have OSA.
- Within TMD population, 85% have Otological Symptoms: tinnitus 42%, ear pain 42%, dizziness 23% and diminished hearing 18%. (in general population between 10%-31% have Otological Symptoms)
Category 10: Psychology and Psychiatry:
- Insomnia: between 10%-15% general population have chronic insomnia.
- In Insomnia cohort, 27%-67% have OSA.
- In OSA cohort, 50% have some type of insomnia.
- OSA concurrent with Insomnia is called “SDB+”
- Sleep Fragmentation and Deprivation leads to: activation of Hypothalamic-Pituitary-Adrenal axis and Sympathetic NS stimulation, and increased cortisol release.
- Within the psychiatric outpatient population the prevalence of OSA is increased.
- Within OSA population, the prevalence of Psychiatric comorbid conditions are increased.
- In OSA cohort, 21.8% have Depression, as compared to 9% in the general population.
- In OSA cohort, 11.9% have experienced PTSD, as compared to 3.9% in general population.
- In OSA cohort, 5.1% experience Psychosis at some point in life, double that seen in general population.
- In Depressive Cohort: @20% have OSA, OR for OSA is 4
- SDB causes increases in: Cognitive Impairment, Mood Swings, ADHD, Difficulty Concentrating, and Circadian Rhythm Disorder.
- Many anxiolytic medications affect sleep architecture. Benzodiazepines reduce muscle tone, compromise airway patency, and reduce REM sleep.
Category 11: Chronic Pain Patients:
- Chronic Pain: 15% in general population, 50% in elderly population.
- Chronic Pain causes a decrease in Slow Wave Sleep.
- Within chronic headache population, 80% have OSA (6:1 male over female)
- Pain reported in 66%-84% of patients with SB
- SB patients have 3x headaches compared with control
- Within Fibromyalgia cohort, 74% have chronic headache, IBS
- Many autoimmune disorders cause muscle and joint pain which can interfere with sleep.
- Bidirectionality Theory: Pain causes poor sleep and poor sleep lowers pain threshold.
- Morning headaches: (must differentiate to: sinus, muscle pain, or vascular)
Category 12: Pediatrics:
- SDB inhibits growth in 1-10% of children by decreasing Insulin Growth Factor.
- Childhood onset asthma predicted development of OSA with OR of 2.1
- 10%-30% of children with SDB are misdiagnosed with asthma
- OR for neurobehavioral problems is 2.98
- When AHI>10 there’s 6x increase in LV hypertrophy
Within “children with OSA” Population:
- Enuresis 7%-30%
- Persistent snoring 100%
- Mouth breathing 84%
Mouth breathing has been associated with altered craniofacial growth, including narrow maxillary arch, posterior crossbite, long anterior face height with clockwise mandibular growth rotation, anterior open bite and mandibular retrognathia. SDB in children has been associated with numerous systemic health consequences including reduced systemic growth, systemic hypertension, and pulmonary hypertension causing right and left ventricular hypertrophy, respectively, as well as behavioral problems such as hyperactivity and attention deficit, aggression, and lower grades in school. Additionally, if left untreated, the altered growth pattern increases the risk of adult OSA. All children should be carefully observed while sleeping and any breathing sounds made, or apparent struggles with breathing, must result in additional diagnostic steps. The Brouilette questionnaire is an excellent screening tool as well.
Using the statistics cited above, it is evident there are many clues to the presence of SDB. Being curious about these subjects will enhance your medical history-taking. Truly understanding them will greatly improve your ability to help your patient’s overall health.
The following questionnaire has been designed to aid in identifying patients at risk and form a medically appropriate basis for dialog with your patient and their other medical providers. Accurate diagnosis will lead to the most complete care for your patient. As future research provides more evidence correlating SDB and comorbidities, this document will be updated.
Scientific Support
Data has been compiled from over 400 articles, including peer reviewed international journals and the ABDSM reading list.
Principles and Practice of Sleep Medicine, Kryger, Roth, and Dement, 4th and 5th Editions, Elsevier, were major resources.
Reprints of this article, a list of the references, and the Lamberg Questionnaire are available at no cost at www.LambergSeminars.com.
The Lamberg Questionnaire “LQ 1.0”
1: Standard Questions
___ Do you awaken unrefreshed or feel sleepy during the day?
___ Is your snoring loud enough to disturb others?
___ How long have you been aware of your snoring?
___ Have you been told your breathing stops while asleep?
___ Do you ever wake yourself from sleep feeling that you are choking?
___ Have you ever had a sleep lab study? If you tried CPAP was pressure > 10.5 cm.
___ Is your BMI>27? Or is your neck size > 17 men, or > 15.5 women?
2: Cardiovascular
___ Do you have high blood pressure, take medicine for hypertension, or have a pacemaker?
___ Ever diagnosed with: CAD, Stroke, Congestive Heart Failure, A Fib, or other cardiomyopathy?
3: Pulmonary
___ Have you experienced difficulty breathing during the day?
___ Do you have shortness of breath, even with mild exertion?
___ Ever been diagnosed with COPD or Asthma?
___ Do you have a chronic cough, either dry or productive?
4: Gastorenterology
___ Do you experience heartburn or acid reflux at night or in the morning?
___ Have you or your dentist noticed erosion on molars?
___ Do you take heartburn medications, either prescription or over the counter?
5: Neurology
___ Do you experience numbness, tingling or pain in your feet or hands?
___ Do you ever experience muscle weakness or difficulty with coordination?
6: Endocrinology
___ Have you been diagnosed with diabetes?
___ Have you unexpectedly gained or lost weight lately?
___ Have you gone through menopause? Are you on HRT?
___ Notice repetitive limb movements or jerks in sleep, urges to move legs, or night sweats?
7: Otolaryngology
___ Do you experience a dry mouth upon awakening?
___ Do you have difficulty breathing through your nose?
___ Do you have allergies that make nasal breathing difficult?
8: Urology
___ Do you have difficulty getting an erection?
___ Do you ever leak urine involuntarily?
___ Do you have to urinate several times at night? Have you been diagnosed with BPH?
___ Experience decreased interest in sex or taken medications to enhance sexual performance?
9: Bruxism and TMD
___ Do you grind your teeth while sleeping? Do your front teeth have a worn look?
___ Have you had jaw muscles or joint pain, ringing in your ears, vertigo, or dizziness?
10: Psychology and Psychiatry
___ Are you irritable upon waking in the morning?
___ Do you experience insomnia (either falling asleep or maintaining sleep)
___ Do you experience: depression, PTSD, memory or concentration problems?
___ Do you take medications for any of these conditions?
11: Chronic Pain
___ Do you often wake up with a headache?
___ Do you experience any chronic pain anywhere in your body?
___ Do you take medications for pain on a daily basis?
12: Pediatrics
___ Do you know any children who are mouth breathers, or who make any sleep breathing sounds?
___ Do you know any children with bedwetting problems?
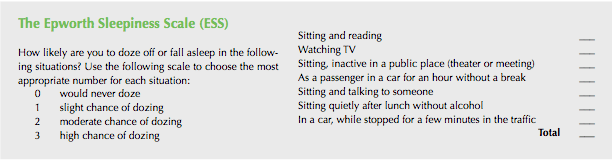
The Epworth Sleepiness Scale (ESS)