The relationship between nasal airway obstruction and OSA shows the importance of dental-sleep clinicians’ assessment of nasal obstruction in relation to the nasal valve. Read more about this here.
by Edward T. Sall, MD, DDS, MBA
While there has been increased acceptance of Mandibular Advancement Splints (MAS) in the treatment of OSA, physicians have concerns about the overall efficacy of OA’s to the known high efficacy of CPAP. It is clear that OSA is a complex disease and that the “gold standard” notion of CPAP or the one treatment approach to OSA is not consistent with our current understanding of the pathophysiology of OSA. While there has been increased awareness of the nonanatomic factors (loop gain, arousal index, and pharyngeal collapsibility) in the pathogenesis of OSA, anatomic factors are still felt to be responsible for the majority of the etiology of OSA.
Oral appliances have greatly evolved since the introduction of monobloc and non-custom appliances, and previous papers have shown increased efficacy of custom appliances versus monobloc. Many physicians are only familiar with legacy appliances and are unaware of fourth generation precision appliances. Precision Oral Appliance Therapy (OAT) is characterized by bite transfer with <1mm of variance and a titration mechanism that holds the jaw in the target position throughout treatment. A recent poster presented at the 2022 World Sleep Congress on 115 consecutive cases showed that a precision oral appliance is capable of successfully treating patients with all levels of severity with most patients treated to an AHI <5. 29 severe patients with an average AHI of 51.5 were treated to a final average of 9.5 (Figure 1). This suggests that precision oral appliance therapy should be considered as the primary form of therapy for all levels of severity of OSA depending on the preference of the patient.

It is known that multilevel anatomic obstruction is often present in snoring and obstructive sleep apnea. Since the nose is the first anatomical boundary of the upper airway, nasal airway obstruction may contribute to sleep disordered breathing. The Starling resistor model, the unstable oral airway, the nasal ventilatory reflex and the role of nitric oxide (NO) may potentially explain the role of nasal pathology in OSA. While there is not a linear correlation between the degree of nasal airway obstruction and the severity of OSA, patients with nasal obstruction have increased problems and decreased efficacy with OAT. Zeng et al. demonstrated that high levels of nasal resistance measured using supine posterior rhinometry predicted poor treatment outcomes with mandibular advancement. This article will introduce a novel in-office procedure for treatment of NAO that should increase the efficacy of OAT, particularly when used in conjunction with fourth generation precision oral appliance therapy.
Nasal Airway Obstruction
Nasal airway obstruction is responsible for many symptoms which include nasal congestion and stuffiness, headache, fatigue, sleep disturbance, daytime sleepiness, snoring, and an overall decline in health-related quality of life (Qol). NAO is one of the most frequent reasons that patients consult an Otolaryngologist and may affect up to 50% of the population. After correction of their nasal obstruction patient’s often report significantly better sleep, less awakenings, and less difficulty falling asleep as well as improved concentration and productivity.
The nose accounts for more than 50% of the total resistance of the upper airway, and nasal breathing serves important physiological functions, including humidification, heating, and filtration. Hipprocrates in “de Morbis Popularthis” noted that nasal polyps were associated with restless sleep and snoring. Additionally, most people have experienced difficulty sleeping during episodes of virally induced nasal congestion. It has been shown that when nasal resistance exceeds a certain level there is a switch from nasal breathing to oral breathing. Mouth breathing is associated with up to 2.5 times higher total resistance and with narrowing of the pharyngeal lumen and a decrease in the retroglossal diameter as a result of further retraction of the tongue. In addition, there is increased oscillation of the soft palate and redundant pharyngeal tissue. All these changes contribute to increased episodes of sleep related breathing disorders.

Common causes of nasal obstruction include deviated nasal septum, inferior turbinate hypertrophy, nasal polyposis, and allergic and nonallergic rhinitis. Medical treatments include nasal steroids, decongestants, leukotriene antagonists, and nasal dilators. Traditionally, the most common surgical procedure for nasal obstruction has been a Septoplasty combined with reduction of the Inferior Turbinates. The most frequent cause of lack of relief of nasal airway obstruction with Septoplasty is failure to address the importance of the nasal valve.
Nasal valve collapse and dysfunction is now recognized as a primary source of nasal obstruction. That being said, it is often underdiagnosed and left untreated. The internal nasal valve is defined as the area between the cartilaginous septum, the caudal end of the upper lateral cartilage, and the anterior head of the inferior turbinate. It is the area of the nasal airway that has the greatest resistance to airflow. On physical examination, insertion of the nasal speculum bypasses the lateral nasal wall and thereby prevents evaluation of this critical structure of the nose.
In the past, surgical procedures that targeted the nasal valve to correct nasal airway obstruction (NAO) or nasal valve dysfunction (NVD) were collectively referred to as a functional rhinoplasty and/or nasal valve repair and include spreader and batten grafts. These procedures were invasive and technically challenging and thus not widely applied to the general population. Possible reasons for undertreating nasal valve collapse and NAO were both the underdiagnosis of this problem and the scarcity of minimally invasive treatment options to address this relatively common problem as an alternative to surgical repair.
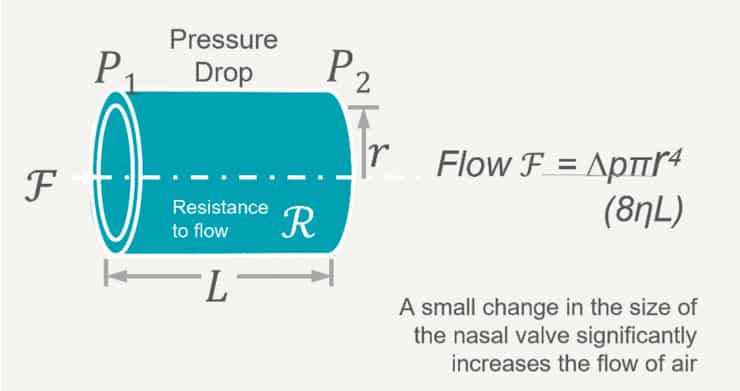
The nasal valve offers the greatest resistance to airflow in the nasal cavity. The normal angle between the upper lateral cartilages and the nasal septum is between 10 and 15 degrees. The narrower that angle, the more susceptible that area is prone to collapse (either static or dynamic). Normal airflow through the nasal valve depends on the Bernoulli principle and Poiseuille’s law. The Bernoulli principle states that as the flow of air increases through a fixed space, the pressure in that space decreases. Thus, if the decrease in pressure overcomes the inherent rigidity of the flexible nasal sidewall collapse can occur resulting in nasal obstruction (dynamic obstruction). Poiseuille’s law states that airflow is inversely proportional to the fourth power of the radius (Figure 3). Small decreases in the radius of the nasal valve will have a dramatic impact in the flow of air through the nose (static obstruction). This principal is the physics behind increased airflow with “Breath-Rite” strips in patients who suffer from a narrowed nasal valve.
Radiofrequency for Treatment of NAO
Radiofrequency (RF) induced heating has been shown to induce tissue tightening and contraction through effects of the collagen fiber network of the tissue. The effects induced by the RF treatment are both acute, through the immediate contraction of existing collagen proteins, and longer term, through induction of the production of new collagen. The VivAer intranasal remodeling is a minimally invasive procedure that uses a stylus to deliver controlled and targeted low energy, temperature RF heating the nasal side wall to gently reshape the tissues of the internal nasal valve (Figure 4). Based on Poiseuille’s law, a small increase in the radius (or angle of the internal nasal valve) will have a dramatic increase in nasal airflow due to decreased nasal obstruction. It is an outpatient procedure performed in the office setting under local anesthesia.
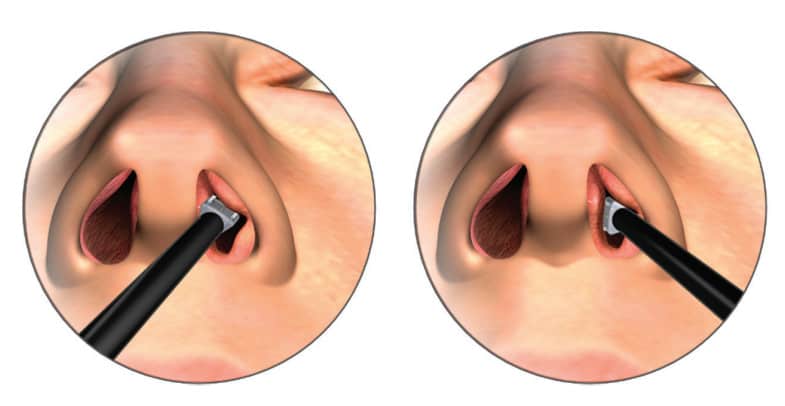
Ephrat, Jacobowitz, and Driver (2021) demonstrated the safety and efficacy of a minimally invasive temperature-controlled RF device that was designed to cause these tissue tightening effects within the submucosal layer of the lateral nasal wall. The VivAer Airway remodeling procedure (Aerin Medical) was associated with stable and lasting improvement in symptoms of nasal obstruction and QoL through 24 months in a noncontrolled single-arm study.
Screening and Assessment of Patients with NAO
The relationship of NAO to OSA necessitates that all practitioners systematically assess their patients for nasal obstruction with particular attention to the nasal valve. While endoscopic evaluation of the nasal cavity is not within the scope of practice of sleep dentists or medical practitioners, an evaluation of the nasal valve is certainly a necessary part of a thorough exam in a patient suspected of having OSA. The NOSE Score (Nasal Obstruction Symptom Evaluation) should be obtained on every patient as it has been shown to be a reliable indicator of nasal obstruction (Figure 5).
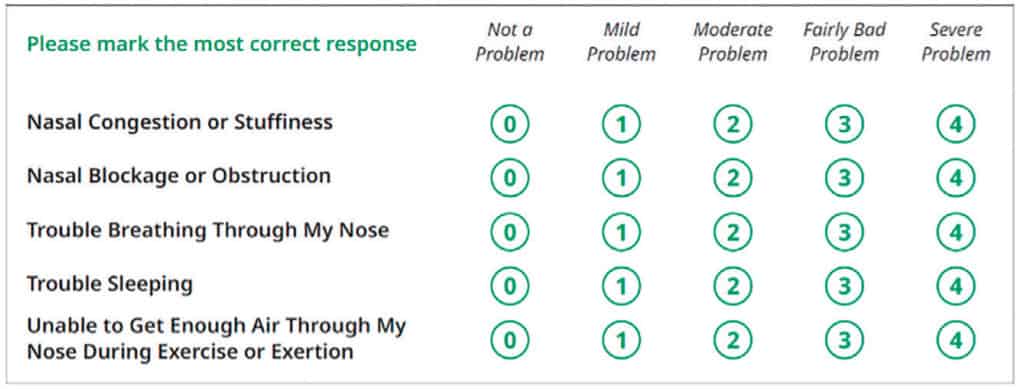
The score is obtained by adding the numbers and multiplying X 5 with the following key:
- Score 30-50 = Moderate Obstruction
- Score 55-75 = Severe Obstruction
- Score 80-100 = Extreme Obstruction
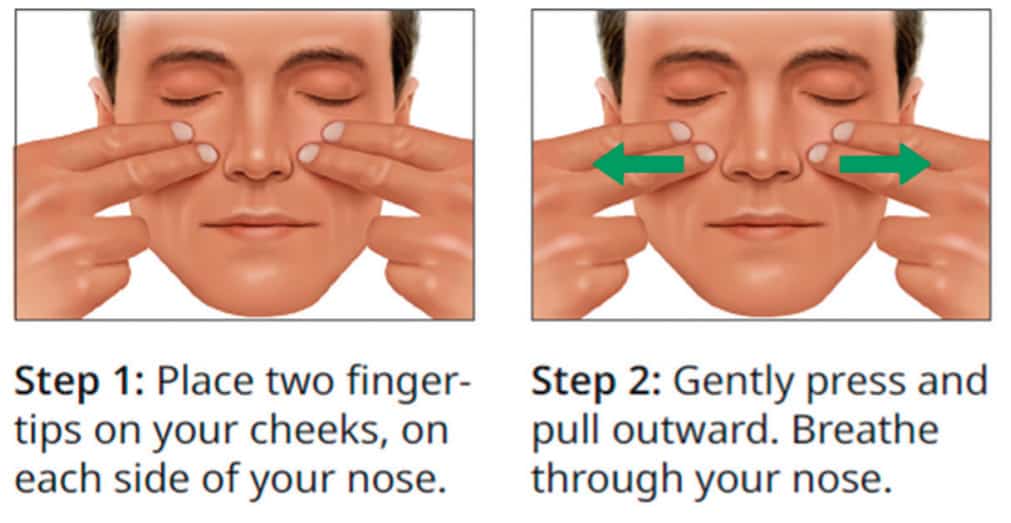
The Cottle Maneuver (gently pulling the cheek laterally with 1-2 fingers to open the nasal valve) is a subjective but relatively reliable indicator of NAO secondary to dysfunction or narrowing of the internal nasal valve (Figure 6). Alternatively, the modified Cottle Maneuver (internally supporting the nasal valve with a curette or probe) is a good test for NAO and can easily be performed by any practitioner.
NAO and Precision Oral Therapy
The field of sleep medicine and specifically our understanding of the different phenotypes of OSA continue to evolve. The more we understand and address both the anatomic and non-anatomic factors in the pathophysiology of OSA the more likely we will increase the efficacy of OAT in the treatment of OSA. The overall efficacy of the 115 patients treated with precision oral appliance therapy could only be improved by critically assessing the presence or absence of NAO. Additionally, a device with a big bulky vertical or anterior component might compromise lip seal and exacerbate any issues with NAO. Clearly the design and performance of a precision appliance is an improvement with respect to these anatomic findings. The more detailed and comprehensive the examination, the more factors may be addressed to improve outcomes. This relationship is an excellent way for sleep dentists, sleep physicians, and otolaryngologists to collaborate to achieve the best outcomes for their patients. Interestingly enough, one of the major reasons that patients discontinue treatment with CPAP is due to problems with nasal obstruction. Likewise, NAO is an important factor to address for optimal response to OAT in the treatment of OSA.
Take Home Points:
- Assess all patients for NAO prior to initiating OAT.
- The NOSE Score is a validated survey that measures the reduced QoL attributed to nasal obstruction.
- Refer patient to Otolaryngologist if NAO suspected.
- VivAer nasal airway remodeling is a reliable and minimally invasive outpatient procedure for NAO secondary to abnormalities of the internal nasal valve.
- Educate sleep physicians on the efficacy of precision OAT as compared to legacy appliances in the past.
- Educate Otolaryngologists on the dentist’s role and expertise in treating OSA with Oral Appliance Therapy.
- Sawa, A, et al. Assessment of screening for nasal obstruction among sleep dentistry outpatients with obstructive sleep apnea. Dent J 2020 Dec; 8 (4): 119.
- Georgalas, C. The role of the nose in snoring and obstructive sleep apnoea: and update. Eur Arch Otorhinolaryngol 2011; 268 (9): 1365-1373.
- Zeng et al. Influence of nasal resistance on oral appliance treatment outcome in obstructive sleep apnea. Sleep 2008 April 1; 31 (4): 543-547.
- Jacobowitz, O, et al. In-office treatment of nasal valve obstruction using a novel, bipolar radiofrequency device. Laryngoscope Investig Otolaryngol 2019 Apr 4 (2): 211-217.
- Ephrat M, et al. Quality-of-life impact after in-office treatment of nasal valve obstruction with a radiofrequency device: 2-year results from a multicenter, prospective clinical trial. International Forum of Allergy & Rhinology; Volume 11, Issue 4: 755-765.
- Rossi A, et al. Clinical evidence in the treatment of Obstructive Sleep Apnoea with Oral Appliance: a systemic review. Int J Dent: 2021: 6676158.
- Rhee, et al. Clinical consensus statement: Diagnosis and management of nasal valve compromise. Otolaryngol Head Neck Surg 2010 Jul; 143 (1): 48-59.
- Brehmer D, et al. A prospective, non-randomized evaluation of a novel low energy radiofrequency treatment for nasal obstruction and snoring. Eur Arch Otorhinolaryngol 2019; 276 (4): 1039-1047.
- Sall, ET. 2022; Precision Oral Appliance Therapy: The Prime-Time Treatment for OSA. Poster presentation; World Sleep Congress, Rome, Italy. March 15, 2022.
- Smith et al 2022; Efficacy of a Novel Precision Iterative Device and Material. Poster presentation; World Sleep Congress, Rome, Italy. March 14, 2022.
- Mosca EV, et al. In-home mandibular repositioning during sleep using MATRx plus predicts outcome and efficacious positioning for oral appliance treatment of obstructive sleep apnea. JCSM. 2022; 18 (3): 911-919.


 Edward T. Sall, MD, DDS, MBA, is a licensed dentist and physician. He is board-certified in both Otolaryngology/Head & Neck Surgery, and Sleep Medicine. Currently, he is in full-time private practice in Syracuse, New York as an Otolaryngologist and Sleep Physician. In 2019, Dr. Sall accepted the position as medical director of ProSomnus Sleep Technologies with the role of increasing physician acceptance of OAT in the treatment of OSA. In 2020, Dr. Sall became the President and CEO of BetterNight Medical group as well as SD Diagnostics, Inc, a home sleep testing company. Currently, Dr. Sall has medical licenses in 40 states which allows him to do telemedicine consultations in sleep medicine for BetterNight. In 2021, Dr. Sall accepted a position as a consultant to Aerin Medical. His role at Aerin Medical is to increase collaboration between sleep dentists and otolaryngologists in order to improve outcomes in patients with OSA treated with both OAT and CPAP.
Edward T. Sall, MD, DDS, MBA, is a licensed dentist and physician. He is board-certified in both Otolaryngology/Head & Neck Surgery, and Sleep Medicine. Currently, he is in full-time private practice in Syracuse, New York as an Otolaryngologist and Sleep Physician. In 2019, Dr. Sall accepted the position as medical director of ProSomnus Sleep Technologies with the role of increasing physician acceptance of OAT in the treatment of OSA. In 2020, Dr. Sall became the President and CEO of BetterNight Medical group as well as SD Diagnostics, Inc, a home sleep testing company. Currently, Dr. Sall has medical licenses in 40 states which allows him to do telemedicine consultations in sleep medicine for BetterNight. In 2021, Dr. Sall accepted a position as a consultant to Aerin Medical. His role at Aerin Medical is to increase collaboration between sleep dentists and otolaryngologists in order to improve outcomes in patients with OSA treated with both OAT and CPAP.