by Allen J. Moses, DDS, Elizabeth T. Kalliath, DMD, and Gloria Pacini, RDH
Introduction
The diagnosis of obstructive sleep apnea (OSA) solely based a Poly-SomnoGraphic study (PSG) is a “rule-in” diagnosis. OSA is just one of many Sleep Breathing Disorders (SBD) that must be considered. There is more to treating OSA than Continuous Positive Air Pressure (CPAP) and intraoral appliances.1 The intent of this article is to identify the integral role sleep dentists can play in improving patients’ health by understanding the mechanics and consequences of patients’ breathing and facial growth. We present some of the dynamics, chemistry, anatomy, and physiology of human respiration, mouth versus nose breathing, under-breathing as well as over-breathing and how allergies and dentistry fit in the picture.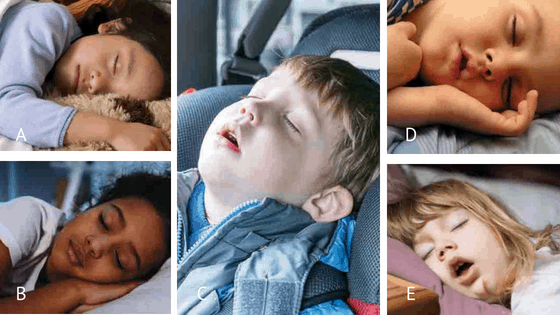
Environmental, intrinsic and structural factors all cause resistance to proper airflow. Humans must adapt to numerous obstacles to sustain breathing.2 Resistance to airflow in the upper airway varies over time but typically two-thirds is of nasal origin and one-third is contributed by the mouth and oropharynx.3
Human beings are designed to be nasal breathers. The union of the foodway and the airway, an arrangement unique to humans, has caused many adaptive problems. The use of the mouth as an emergency, back-up airway outweighs the possible dangers of choking and infection.4 During inhalation the nose performs some important, vital functions, namely warming, humidification, filtering and cleaning of ambient inhaled air into the lungs, as well as olfaction. It also provides the function of dehumidification of air exhaled through the nose.5,6 The nose is a highly complex organ, initiating reflexes affecting itself as well as the rest of the body, notably a sniff reflex, sneeze reflex, autonomic airway/lung reflexes and cardiovascular reflexes.
Anatomy, Histology, Physiology
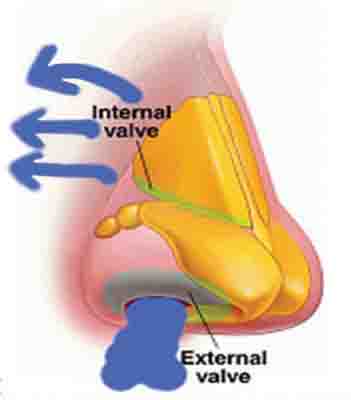
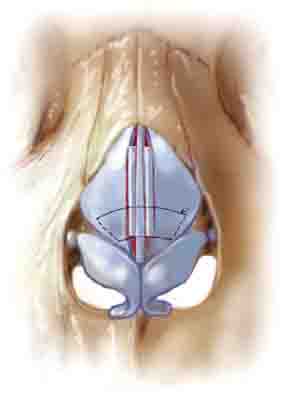

Figure 2: Perspective views of the nasal valves. Source for Fig 2B: Surgical Treatment of Nasal Obstruction in Rhinoplasty. Aesthet Surg J. 2010;30(3):347-378.
The vasculature of the nose is extensive, consisting of sinusoidal capacitance vessels, distensible venule capacitance vessels, arteriovenous anastomoses, arteries capillaries, and venules. The secretory tissue of the nose consists of epithelial cells, submucous glands, serous glands and pseudostratified epithelium. The arterial system determines blood flow. The venous system, or capacitance vessels, determines nasal patency. The capacitance vessels are regulated by the autonomic nervous system, contain smooth muscle and are most dense in the inferior and middle turbinates.7
Sympathetic and parasympathetic nerves play critical roles in regulating glandular, vascular and other processes in airway mucosa such as allergies. Sympathetic nerve stimulation causes constriction of the resistance vessels. Nasal congestion is more a withdrawal of sympathetic discharge than over activity of the parasympathetic system. Parasympathetic nerve stimulation of the nasal vasculature causes arterial dilation and active secretion of mucous resulting in runny nose. Allergy is a histaminic reaction characterized by vasomotor rhinitis, mucosal hyperemia, vascular engorgement, hyperrhinorhea, and obstructed nasal breathing.8
 Nasal airflow resistance is decreased by exercise which causes sympathetic vasoconstriction, erect posture resulting in jugulovenous distension as well as rebreathing which brings about increased blood CO2 and by nasal vasoconstriction.9
Nasal airflow resistance is decreased by exercise which causes sympathetic vasoconstriction, erect posture resulting in jugulovenous distension as well as rebreathing which brings about increased blood CO2 and by nasal vasoconstriction.9
Factors increasing nasal resistance are supine posture, hyperventilation resulting from mouth breathing, allergic rhinitis, infective rhinitis, cold air, alcohol, hypertrophic turbinates and/or nasal valve collapse. The key to successful nasal breathing is maintaining a critical balance.10
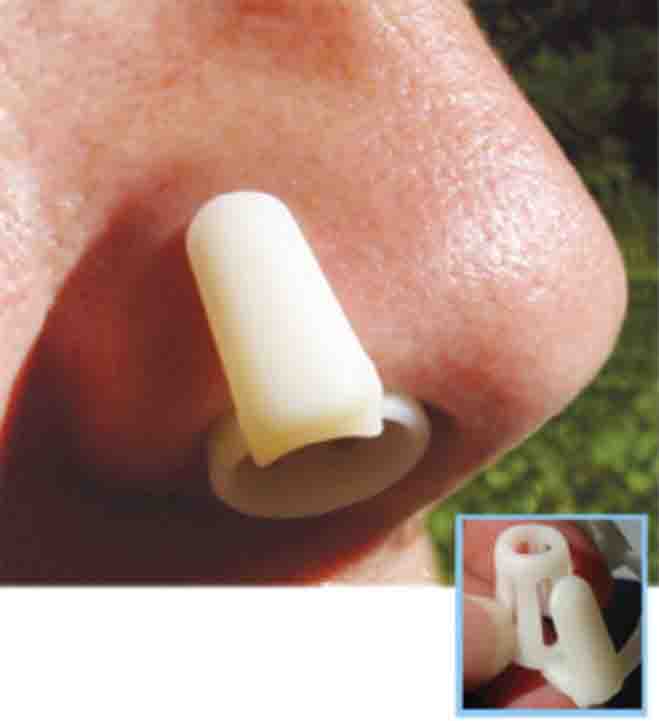
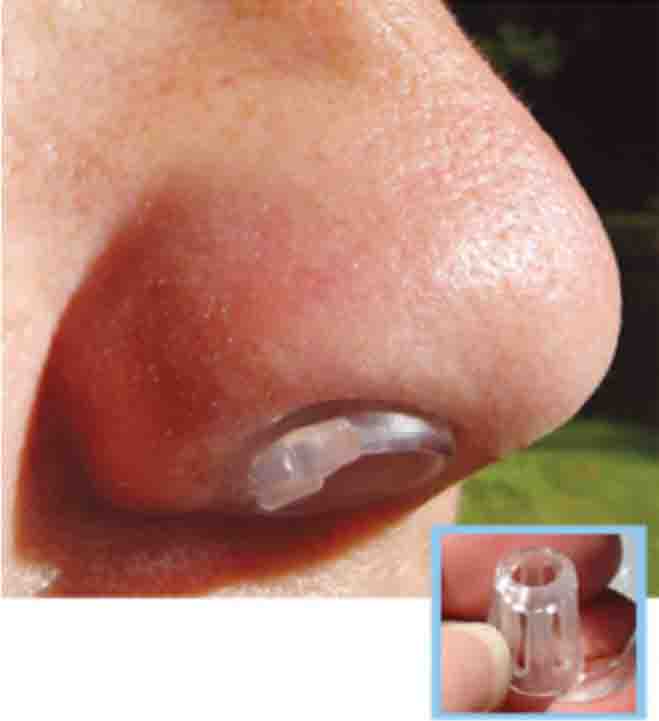
Figure 3: Internal nasal dilators. A. Sinus Cones® B. Max-Air Nose Cones®
Nasal Valve
The nasal vestibule, at the entrance of the pyriform aperture is the first component of nasal resistance. The clinical relevance of the nasal valve is that it is the narrowest part of the nasal airway system and contributes over 50% of nasal resistance.11 The nasal vestibule is composed of compliant walls that are liable to collapse from the negative pressures generated during inspiration. The valve area is dynamic; venous erectile tissue can cause marked obstruction. The nasal vestibule is primarily supported by alar cartilage and musculofibrous attachments. The angle between the septum and the upper lateral cartilage is 10-15°. The internal nasal valve is usually located less than 2 cm distal in the nasal passageway, approximately 1.3 cm from the naris. The average cross-sectional area is 0.73 cm. Studies have shown 30 L/min is the normal limiting flow during inspiration, beyond which nasal airway collapse is likely to occur in this area. Despite the tendency, airway collapse is prevented by activation of the dilator naris muscles during inspiration. During expiration, positive pressure is the driving force for nasal vestibule dilation.12
Oral appliances contribute to reduction of pharyngeal resistance by dilating the narrowest areas of airway diameter. Clinicians trained in oral appliance therapy should be capable of identifying nasal resistance and the non-invasive tools available for reducing nasal resistance.
Types of Nasal Airflow

The biomechanics of nasal resistance relates to understanding of the two distinctive types of airflow – turbulent and laminar. Laminar airflow is not conducive to air modification, heat and mass transfer occurs slowly, contact of airborne particles and pollutants with mucosa is minimal and filtration is impaired due to less surface area to pass over. Turbulent airflow brings about better warming, filtration and humidification of air, irregular flow, exhibits differing velocities and it increases the work of breathing.
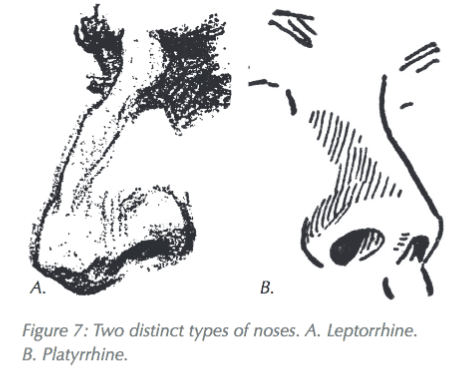
Types of Noses
On the bases of two distinct types of airflow, two distinct types of noses can be characterized – leptorhine and platyrhine. Leptorrhine noses are tall & narrow, have a downward and inferior direction of the nares, maximum mucosal surface to volume, they facilitate heat and moisture exchange in cold, dry environments, airflow must negotiate 90º bend from external nares to horizontal chamber, have well developed nasal valve, greater projection of the nose, high nasal sill and projecting turbinates that enhance turbulent airflow.
Platyrhine noses are short and broad. They have a lower surface area to volume ratio, less efficient heat recapture, nares more anteriorly directed, poor or no development of nasal valve, poorly developed or no nasal sill, little or small projection of turbinates, eco-geographically warm weather settler.


Figure 5: A. Nares constrict. B. Nares flare. Source for Fig. 5A: Hurbis, Charles Gerard. Arch Facial Plast Surg. 2008; 10(2):142-143.
SNIFF TEST
Seal your lips, take a deep breath through your nose as deep and as fast as you canNasal obstruction – the nares constrict (see Figure 5A)Nose breather – the nares flare (see Figure 5B)

Mouth Breathing
Nasal obstruction can cause the central nervous system to initiate oral breathing. The following functional adaptations must occur for nasal breathers to breathe through the mouth: the soft palate is raised to make a nasal seal with posterior pharyngeal wall, the mandible drops to facilitate oral breathing, the tongue is lowered from contact with the palate, anterior tongue shape flattens, greater inter-arch freeway space is created, swallowing occurs with the teeth apart (dysphagia), scalloped border of tongue develops, dentoalveolar intrusion of lower posterior teeth (step plane of occlusion), higher narrower palate results, as well as maxilary posterior crossbite, lowered tongue position (reduced cross-sectional area of pharyngeal airway), narrow palate results in narrow nasal passage and increased nasal airway resistance, dysphagia from anterior tongue thrust and the constantly open mouth results in extrusion of posterior teeth (anterior open bite).13
A characteristic of chronic mouth-breathers is forward head posture. The hyoid musculature contracts to pull the mandible distal and inferior for maintenance of the open mouth, the suboccipitals and SCMs extend the head, the mid and lower trapezius and rhomboid muscles are protracted (flexion) and internal rotation of the shoulders. The resultant clinical findings in mouth-breathers are long face, anterior open bite, high palatal vault, steep mandibular plane angle, malocclusion, inflamed anterior gingiva, incompetent lip closure, open mouth gaping expression, forward head posture, no diaphragmatic breathing, neck and shoulder breathing instead and rapid breath rate.14
Thumb or Digit, Sucking vs Propping
Infants and small children are often seen with a finger in their mouth. This is correctly referred to as “digit habit”. There are two distinct kinds of digit habit that must be differentiated – sucking and propping. There are children who truly suck their thumb or other finger. In these kids the digit is a nipple substitute. The lips completely surround the digit, the tongue engages the anterior segment of the digit, the soft palate is in contact with the back of the tongue, the child is nose breathing and there is negative pressure in the mouth. Try and remove the digit and you will experience the suction.15


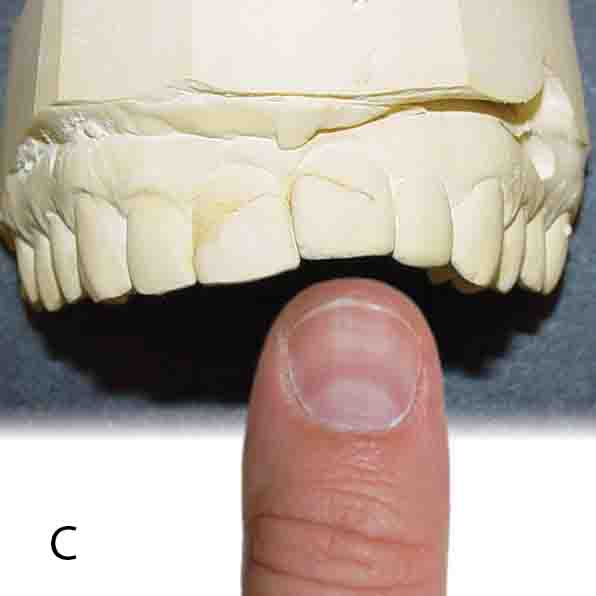

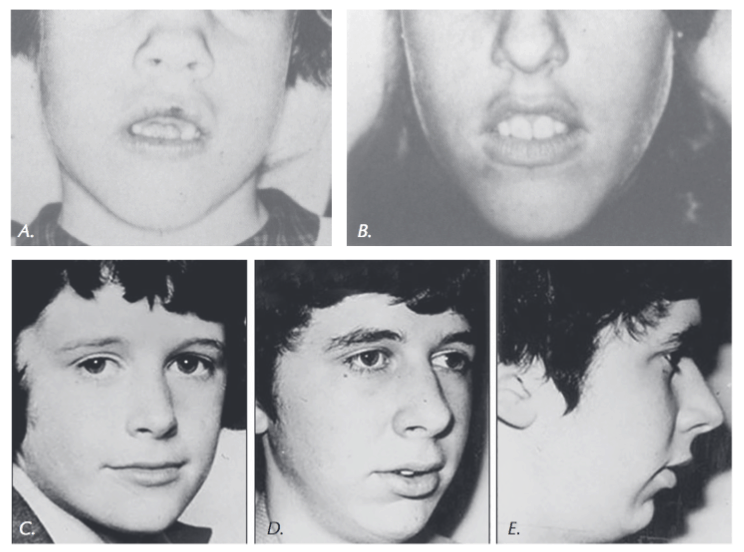
Figure 8: A. Thumb propper. B. Thumb sucker. C. When you see this and think of the thumb… D. You begin to understand this
With digit proppers the lips are not closed, the digit is between the lower front teeth and the hard palate, the tongue is in the floor of the mouth and the child is mouth breathing. The digit is propping the mouth open so the child can oral breathe because their nose is obstructed. Propping exerts repetitive, deleterious forces on the child’s developing dentition and face.
Clinicians trained in oral appliance therapy should be capable of identifying nasal resistance.
The question, “Can mouth breathing cause OSA?” has generated many studies. Deegan16 and McLean17 point out that a variety of defective respiratory and control methods are found in OSA including impaired respiratory drive, defective inspiratory load responses and local upper airway protective reflexes appear to be important. Sforza18 emphasizes that the lower position of the hyoid bone and abnormal pharyngeal soft tissue in mouth-breathers contribute to the upper airway patency. Horner19 also showed that the lower position of the hyoid bone and abnormal pharyngeal soft tissue in mouth-breathers contributes to significant collapsibility to the upper airway and that sleep reduces the activity of pharyngeal dilators and reduces the ability of the pharynx to defend itself from collapse. The summary of these papers is that because OSA is not exclusive to mouth breathers, it could possibly cause OSA or be a risk factor but that it is not the proximal cause.


Conclusion
There are daytime breathing problems that can exacerbate or possibly cause OSA during sleep. The complex functional and morphologic relationship of the nose and mouth was presented. A dysfunctional relationship between nose and mouth breathing can have serious health consequences. Dentistry is a health specialty well-qualified to prevent and treat the etiologies as well as the symptoms. It is important to not only treat both the causes and effects, but understand the respiratory physiologic effects. That is the subject of Part II in this series.