Dr. Steve Carstensen and Karen Davidson’s article notes that while the first breath of life is by necessity through the mouth, every breath after that is best accomplished by nose breathing. Find out the benefits and ways to test and help your patients breathe correctly.
 by Steve Carstensen, DDS, D.ABDSM, and Karen Davidson, DHA, MSA, MEd, MSN, RN
by Steve Carstensen, DDS, D.ABDSM, and Karen Davidson, DHA, MSA, MEd, MSN, RN
To prepare yourself to read this article, take a breath. In, then out. Did it feel like every other breath – did you notice anything? Nothing? That is to be expected. It’s normal, and that breath was probably not as good for you as it could have been.
This is true for most people. And not just when their airway collapses during sleep and we label them ‘patient’ with a disease that requires our help. Pick up Breath by Nestor and The Breathing Cure by McKeown to learn more. Read on to learn what to say about where it all begins: the nose and how we make it work for or against our best health.
Oxygen is abundant: at sea level, about 21% of inhaled air, 16% exhaled after we’ve extracted all we need. But oxygen is only one of three critical gases related to nose breathing.
Carbon dioxide is 0.04% of the air we breathe but 4% of what we exhale – it is a byproduct of energy production in our cells. CO2 levels also control respiration rate and affect oxygen uptake in the blood.1 Hypocapnia results in less oxygen available for mitochondria to make energy.
Tanaka et al., found that end-tidal-CO2 concentrations were higher during nose breathing than during oral breathing. A group of healthy volunteers had an average CO2 of about 43.7 mm Hg for nose breathing and only around 40.6 mm Hg for oral breathing. The immediate negative biochemical effects of mouth-breathing related to CO2 are: Hypocapnia, reduced oxygenation to the body and vital organs, mental health conditions including anxiety, addictive behavior, and negative emotions. The emotional aspect can lead to stress and add to sleeping problems.2 Hypocapnia also leads to central sleep apnea and probably has a role in obstructive sleep apnea.3
While studies are ongoing for effects on COVID-19, NO was studied during SARS outbreaks and found to limit infections.
Our noses are no mere portals for gas flow. If we want to make sure our bodies can get oxygen to the cells, an exchange and transport process must take place. Healthy lung tissues are coated with a special surfactant – without it, the alveoli cannot stay open in the deepest part of the lungs. Transfer molecules responsible for moving oxygen from air to blood and CO2 into air are blocked when the tissues are hard, inflexible, and dry. A key ingredient that allows surfactant to be produced in the lungs is nitric oxide, NO.
Hummmmm. Do it with me – hum while you breathe through your nose and read this paragraph. A 2002 study measured nitric oxide in nasal- and mouth-breathing, with and without humming. The differences are startling: Mouth-breathing produced 104nl/min – humming had no effect. Switching to nose breathing resulted in 189nl/min NO production. Add humming: 2818 nl/min – a 15-fold increase.4 Nitric oxide is produced in the sinuses and drawn into the lungs during nasal inspiration. In clinic, suggest humming during breathing exercises to slow exhalations. Nestor’s and McKeown’s books are replete with helpful exercises you can promote to your patients.
Clear sinuses and 100% nasal breathing provide enough nitric oxide (Molecule of the Year in 1992, according to Science magazine) for proper lung function. Nitric oxide has antibacterial and antiviral properties. While studies are ongoing for effects on COVID-19, NO was studied during SARS outbreaks and found to limit infections. People who breathe through their noses were found to have fewer rhinovirus infections – colds and flu.5 There are many great properties of NO but getting people’s attention only needs a couple of key points, and these days, ‘antiviral’ is enough.
Let’s go deeper. You know that Cranial Nerve 1, Olfactory, has specialized receptor neurons that allow our cortex to assess our environment for threat or reward by sniffing volumes of air into the upper reaches of our nose, around the superior turbinate. What is less well understood are the mechanoreceptor cilia connected to axons of CN1 that travel to the limbic system. In a landmark study,6 rare patients with epilepsy who had electrodes implanted in their brains were led through a series of breathing exercises. Neuronal activity in the piriform complex, amygdala, and hippocampus tracked along with nasal breathing but not when the subjects breathed through their mouths. While full conclusions of the physiologic importance of this synchrony are still being considered, the authors note “behavioral data in healthy subjects suggest that breathing phase systematically influences cognitive tasks related to amygdala and hippocampal functions.” Other experiments cited in this paper show nasal breathing serves as a common “clock” to organize spatiotemporal excitability (a sense of space and time) broadly throughout the brain. Nasal breathing helps your patients be calmer, smarter, and more graceful in moving through their environment.
Is there an objective way to know if patients can breathe well through their nose? Over a hundred years ago, Dr. Glatzel promoted a cold mirror inscribed with lines – by holding the mirror under the nose, fogging on the cold mirror would reveal differences between left and right nasal passages. Not quantifiable, but helpful to show patients.
Rhinomanometry is a non-invasive, 4- minute test that provides real-time objective data about nasal airway resistance and the patency of the nose. It measures the pressure and flow for left and right nasal passages during normal inspiration and expiration. It can independently measure one nostril at a time with active anterior rhinomanometry to provide a graphic illustration of airflow, or both nostrils simultaneously with active posterior rhinomanometry, but it does not tell the clinician where the site of obstruction lies. Interventions such as decongestants and rinses can be used and results measured with this device for short-term comparisons, patient education, and treatment progress. Since the nose undergoes normal cycling, which changes the shape of the turbinates and thickness of the mucosa on a 2 – 3-hour timeframe, in addition to other variables such as gender, age, testing position (sitting vs. supine) and time of day, to name a few, using rhinomanometry for clinical decision-making may be imprecise, yet a valuable assessment tool across many specialties. Studies show a profound relationship between nasal resistance, posture, and treatment options for sleep disordered breathing.
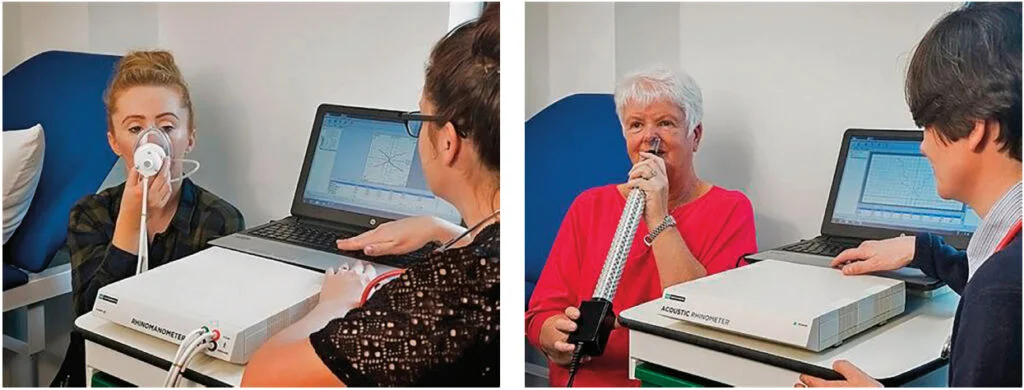
What about using rhinomanometry to see if children have normal airflow? Hosseini et al, recently published “the correlations identified between anatomic data and pressure gradient have clinical implications in pediatric rhinology, suggesting that certain aspects of airway anatomy in infants and children can be predicted through the measurement of intranasal pressure gradient measured with rhinomanometry.”7
Acoustic rhinometry provides, using a sound wave, an accurate picture of nasal airway anatomy. This can show with precision where the airflow is most restricted. Otorhinolaryngologists have found nasal endoscopy more useful for diagnosis. Using the camera while the patient is sedated is called Drug Induced Sleep Endoscopy, or DISE.
There is much more to understand about how the nose works and the myriad benefits of nasal breathing. While the first breath of life is by necessity through the mouth, every breath after that one is best done through the organ designed for it – the nose. When you can influence your patients at every stage of life to breathe through their mouth as often as they eat through their nose, you are on the right track. Are you thinking about your own breathing? Feel anything different?
Michael Flannell shows the power of nasal breathing by showing how athletes can benefit. Read “The Athlete’s Secret Ingredient: The Power of Nasal Breathing” at https://dentalsleeppractice.com/the-athletes-secret-ingredient-the-power-of-nasal-breathing/.
- Hlastala MP, Woodson RD. Saturation dependency of the Bohr effect: interactions among H-+, CO2, and DPG. J Appl Physiol. 1975 Jun;38(6):1126-31. doi: 10.1152/jappl.1975.38.6.1126. PMID: 237871.
- Tanaka, Y., Morikawa, T., & Honda, Y. (1988, Oct. 1). An assessment of nasal functions in control of breathing. Journal of Applied Physiology, 65(4), 1520-1524. https://doi.org/10.1152/jappl.1988.65.4.1520
- Badr MS, Dingell JD, Javaheri S. Central Sleep Apnea: a Brief Review. Curr Pulmonol Rep. 2019 Mar;8(1):14-21. doi: 10.1007/s13665-019-0221-z. Epub 2019 Mar 13. PMID: 31788413; PMCID: PMC6883649.
- Weitzberg, E., Lundberg, J.: Humming Greatly Increases Nasal Nitric Oxide. Am J Respir Crit Care Med 166(2):144-145, 2002.
- Fabio Lisi, Alexander N. Zelikin, Rona Chandrawati: Nitric Oxide to Fight Viral Infections Adv Sci (Weinh)2021 Apr; 8(7): 2003895. Published online 2021 Feb 9.
- Zelano et al. • Human Limbic Respiratory Oscillations Neurosci., December 7, 2016 • 36(49):12448 –12467
- Hosseini, S. Schuman, T. A. & Golshahi, L. (2021, June). correlations to estimate the key anatomical dimensions of pediatric nasal airways using minimally invasive measurements of intranasal pressure gradient. Journal of Aerosol Medicine and Pulmonary Drug Delivery, 34(3), 171-180. http://doi.org/10.1089/jamp.2019.1586
 Steve Carstensen, DDS, has treated sleep apnea and snoring in Bellevue, WA since 1998. He’s the Consultant to the ADA for sleep related breathing disorders, has trained at UCLA’s Mini-Residency in Sleep and is a Diplomate of the American Board of Dental Sleep Medicine. He lectures internationally, directs sleep education at Airway Technologies and the Pankey Institute and is a guest lecturer at Spear Education and Louisiana State Dental School, in addition to advising several other sleep-related manufacturers. From 2014 – 2019 he was Editor of Dental Sleep Practice magazine. In 2019, Quintessence published A Clinician’s Handbook for Dental Sleep Medicine, written with a co-author.
Steve Carstensen, DDS, has treated sleep apnea and snoring in Bellevue, WA since 1998. He’s the Consultant to the ADA for sleep related breathing disorders, has trained at UCLA’s Mini-Residency in Sleep and is a Diplomate of the American Board of Dental Sleep Medicine. He lectures internationally, directs sleep education at Airway Technologies and the Pankey Institute and is a guest lecturer at Spear Education and Louisiana State Dental School, in addition to advising several other sleep-related manufacturers. From 2014 – 2019 he was Editor of Dental Sleep Practice magazine. In 2019, Quintessence published A Clinician’s Handbook for Dental Sleep Medicine, written with a co-author. Karen Davidson, DHA, MSA, MEd., MSN, RN, has held many positions in the medical device industry over the past 25 years, specifically in the ENT and Sleep markets, in addition to 29 years of clinical experience to include service as a Flight Nurse in the United States Air Force Reserves. Dr. Davidson serves as the Vice President at GM Instruments, Ltd. with a special interest in the technology of objective nasal measurements, nasal physiology, clinical application, reimbursement, health economics, and health policy.
Karen Davidson, DHA, MSA, MEd., MSN, RN, has held many positions in the medical device industry over the past 25 years, specifically in the ENT and Sleep markets, in addition to 29 years of clinical experience to include service as a Flight Nurse in the United States Air Force Reserves. Dr. Davidson serves as the Vice President at GM Instruments, Ltd. with a special interest in the technology of objective nasal measurements, nasal physiology, clinical application, reimbursement, health economics, and health policy.