Drs. Barry Glassman and Don Malizia delve into occlusal guards and the possible consequences.
by Barry Glassman, DMD, and Don Malizia, DDS
Oral appliances used in the treatment of primary snoring and obstructive sleep apnea (OSA) have been shown to be potentially as effective in mean disease alleviation as CPAP therapy.1,2 The active mechanism these oral appliances utilize is mandibular protrusion. Mandibular protrusion has been shown to increase the muscle tone of the pharyngeal dilators during sleep, thereby counteracting the tendency to have the sleep-induced loss of muscle tone contribute to pharyngeal collapse. It is also noted that mandibular protrusion also tends to stabilize the hyoid bone, which, in the human as opposed to other mammals, is a floating bone that does not articulate with the styloid process of the petrous temporal bone. Mandibular protrusion with hyoid stabilization stabilizes the anterior pharyngeal wall.
80-90% of those who have some degree of sleep disturbed breathing are undiagnosed.3 Consequently, patients who are treated in dental offices may indeed be among those who remain undiagnosed with OSA. Misconceptions that only overweight men suffer from apnea or that it is possible to identify apneics in a clinical examination must be dispelled if we are to properly diagnose more patients more effectively. Proper screening should be performed.4
Over 3 million occlusal splints to manage sleep bruxism and TMD are annually prescribed by dentists in the US.5 It was theorized by Gagnon, et al that these appliances, by the very nature of the interocclusal acrylic, would have several consequences, including a retruded mandible and decreased tongue space. The authors then hypothesized that “the use of a single maxillary oral splint may aggravate respiratory disturbance in sleep apneic patients.”6
The potential relevance of this hypothesis is noteworthy. The severity of OSA is associated with the significant cardiovascular disorders of hypertension, stroke, heart failure, and is potentially associated with sudden death.7 Other significant disorders associated with OSA include diabetes and migraine. Recent studies have noted a possible association with Alzheimer’s disease. OSA is often a major contributing factor to excessive daytime sleepiness, and thus can contribute to the cause of motor vehicle accidents and work mishaps.7 With the use of maxillary splints, could dentistry have a long history of inadvertently contributing to increasing the likelihood of these serious untoward consequences?
Sleep medicine is a young science. The potential effectiveness of oral appliances combined with the issues of compliance associated with positive airway pressure – the “gold standard” of OSA care – have made dental sleep medicine continuing education among the most popular courses available. After the publication of the 2004 Gagnon, et al study many esteemed lecturers authoritatively decreed from the podium that dentistry has been responsible for making OSA worse by using “night guards.” Accusations included the charge that anyone who uses a night guard or occlusal splint without testing their patient for OSA is committing malpractice. Further assumptions claimed that if a maxillary occlusal appliance can Increase the disease in patients with apnea, it most likely can create apnea in the non-apneic patient. Let’s review the 2004 Gagnon, et al study to uncover what it really shows and maybe more importantly, what it doesn’t show.
Methods of the 2004 Gagnon Study
Ten patients (3 women and 7 men) who had reported snoring and, after a single night study, were determined to have an AHI greater than 5, were the subjects of this study. It is noteworthy that three of the patients were taking anti-depressive anxiolytic medication.
All ten patients were fitted with a maxillary occlusal splint. They were given two weeks to adapt to the occlusal night guard. They then removed the oral splint for three weeks and participated in a “baseline” study without the appliance. The ten subjects were then instructed to wear the oral appliance for a week when they returned for the third study, this one with the splint in place.
Results of the 2004 Gagnon Study
The variables that were compared in the two studies included but were not limited to the apnea hypopnea index (AHI), the respiratory disturbance index (RDI), the Epworth Sleepiness Scale (ESS), upper airway resistance, percent of time with snoring sounds, and percent of time in the supine position.
Interestingly, it was reported that “there was no statistically significant difference in any of the sleep variables between the baseline and splint nights.” Yet it was noted that six subjects experienced an increase in AHI with the splint. This resulted in changes in the diagnostic classification of sleep apnea with one patient getting better (from moderate to mild) but four patients getting worse (two went from mild to moderate, and two went from moderate to severe). The RDI was increased in six patients as well. Eight patients had an increase in snoring time with the splint in place.6
“…many esteemed lecturers authoritatively decreed from the podium that dentistry has been responsible for making OSA worse by using ‘night guards.’”
Comments on the results
Night to night variability and postural effect
The small sample clearly limits the power of the study. Differences in amount of time spent in the supine position alone can result in an altered AHI beyond the normal night to night variability. In the discussion the authors comment that future studies should be done with a larger sample size using double blind rather than single blind methodology.
Does snoring time alone indicate the validity of increased snoring as a diagnostic tool?
Eight patients had increased snoring time with the appliance in place. There was no reference to the thresholds to determine snoring or any discussion of decibel levels. There was also no discussion as to what that increased time was or if that time was within the limits of night-to-night variability or related to increased time supine.
Clinical relevance of the potential change in sleep disturbed breathing
Those who have taken the results of this study and admonished dentistry over the use of a maxillary splint for bruxism and/or TMD have leaned on the study’s report of increased AHI with the appliance in place. The AHI increase has been emphasized even though it has since been shown that there is no direct relationship between AHI and the associated disease states.8 This lack of a direct relationship puts into question any suggestion that a percentage of increase of AHI is clinically relevant
The percentage the AHI is increased can be statistically significant without being clinically significant, especially in the lower AHI ranges.
Could the use of the medications in the patient sample possibly have confounded the study?
In the 2004 Gagnon, et al study it was reported that three of the ten subjects were taking anti-depressive or anxiolytic medications and that the use of the medications was not interrupted. Neither the specific medication nor which patients were taking that medication was identified. The use of SSRIs, for example, can have a profound effect on sleep and can increase bruxism and negatively affect sleep quality.9,10 It should be noted that the Kuwashima, et al 2019 study that refuted the results of increased AHI with maxillary or mandibular splints excluded any patients taking any medication that could influence sleep.11
Can the use of a maxillary splint cause apnea in a non-apneic patient?
With the results of the Gagnon, et al study in hand, self-anointed gurus have unjustifiably pronounced that ‘night guards’ or ‘bite splints’ will worsen AHI in patients or cause sleep apnea when it didn’t previously exist. In 2019 Kuwashima, et al completed double blind randomized control study with 26 patients who were diagnosed with TMD.11 Subjects with an elevated Epworth Sleepiness Scale score or those that tested positive on the validated STOP-BANG screener were excluded from the study. Those patients who required appliance therapy for bruxism as determined by the AASM classification of movement disorders12 were randomly given either a maxillary or mandibular splint. A baseline home study was taken before and after the appliance insertion, and it was noted that the AHI tended to decrease in both appliance groups. It was concluded that neither the increased vertical dimension nor the decreased tongue space resulted in an increased AHI.
Have the study results been reproduced or refuted?
In 2011, Nikolopoulou, et al study utilized a sample group of eighteen patients with OSA.13 They underwent full polysomnograms and were then provided mandibular advancement devices that consisted of a maxillary and mandibular units which increased the vertical dimension in the anterior segment by six millimeters. The appliance was not advanced, and afterward a follow-up study was completed. “No significant difference in AHI was noted between the baseline night and the 0 % MAD night.” There were, however, two patients whose AHI increase was significant. The conclusion made in this pilot study was that it is possible that some patients may be at risk for aggravation of their OSA with appliance therapy.
With the pilot study behind them, in 2013, Nikolopoulou, et al, attempted to access the influence of occlusal stabilization splints on patients with OSA.14 Ten patients underwent three polysomnogram recordings with their maxillary “stabilization” appliances in place and three without their appliances in a crossover design. The study confirmed that the increased AHI with the appliance in place was small, and that there was no change in the subject’s Epworth Sleepiness Score. With that small increase, clinical significance was deemed unlikely.
The 2019, Kuwashima, et al study demonstrated in their double-blind controlled study that the increased vertical dimension with the use of either a maxillary or mandibular appliance tended to decrease the AHI of patients who were given an appliance for treatment of their TMD.11
Summary
Six of the ten 2004 Gagnon, et al subjects were shown to have increased AHI with the appliance in place, but the difference was not statistically significant.
In the discussion, the astute authors noted the potential confounding issues of altered posture from night to night that were not taken into consideration. They also noted that longer observational periods could have affected the results. It was observed that the study was not double-blinded and potentially affected by bias. Another stated limitation was that night-to-night variability could have contributed significantly to the results.
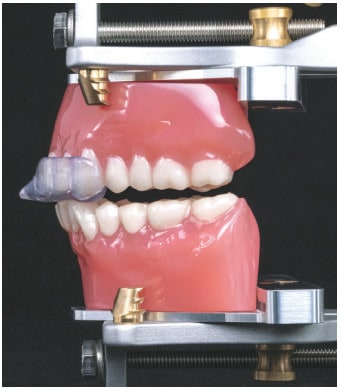
The Gagnon, et al study was an excellent pilot study that encouraged further work. The real concern is not with the study, but with the response of the dental sleep community that has ignored the limitations, the actual data, and irresponsibly developed conclusions purportedly confirming the tendency of splints to aggravate patient’s OSA. The misconception was further exaggerated to the assumption that a maxillary splint could cause OSA in non-apneic patients. These assumptions continue to pervade the dental community despite the subsequent, well-designed studies that have questioned the direct relationship between a maxillary appliance for TMD and/or bruxism and the aggravation of a patient’s OSA. Therefore, the concern for use of a maxillary appliance may not be valid. It’s also important to note that no studies have shown worsening of AHI with an NTI-tss device (Glidewell Dental, Newport Beach, CA) or other anterior segmented splints (Figure 1).
As clinicians, we are responsible for critically evaluating research before making clinical decisions, and the onus is on opinion leaders to responsibly share information from the rostrum. Dentistry has been charged with screening all patients for obstructive sleep apnea with the use of a validated screening tool. Comprehensive screening and referral to sleep physicians when indicated would prevent any inadvertent increase in OSA with any dental procedure.
Occlusal guards can prevent some challenges. Read “Open Airways, Open Bites — Important Choices for your Patients” by Dr. Paul McLornan to find out more about positive effects of mandibular repositioning devices on SDB patients. https://dentalsleeppractice.com/open-airwaysopen-bites-important-choices-for-your-patients/
- Anandam, A., et al., Cardiovascular mortality in obstructive sleep apnoea treated with continuous positive airway pressure or oral appliance: An observational study. Respirology, 2013. 18(8): p. 1184-1190.
- Phillips, C.L., et al., Health Outcomes of Continuous Positive Airway Pressure versus Oral Appliance Treatment for Obstructive Sleep Apnea. American Journal of Respiratory and Critical Care Medicine, 2013. 187(8): p. 879-887.
- Finkel, K.J., et al., Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med, 2009. 10(7): p. 753-8.
- Jonas, D.E., et al., Screening for obstructive sleep apnea in adults: evidence report and systematic review for the US Preventive Services Task Force. Jama, 2017. 317(4): p. 415-433.
- Pierce, C., et al., Dental splint prescription patterns: a survey. J Am Dent Assoc, 1995. 126(2): p. 248-254.
- Gagnon, Y., et al., Aggravation of respiratory disturbances by the use of an occlusal splint in apneic patients: a pilot study. International Journal of Prosthodontics, 2004. 17(4).
- Knauert, M., et al., Clinical consequences and economic costs of untreated obstructive sleep apnea syndrome. World Journal of Otorhinolaryngology-Head and Neck Surgery, 2015. 1(1): p. 17-27.
- Malhotra, A., et al., Metrics of Sleep Apnea Severity: Beyond the AHI. Sleep, 2021.
- Garrett, A.R. and J.S. Hawley, SSRI-associated bruxism: A systematic review of published case reports. Clinical practice, 2018. 8(2): p. 135-141.
- Medscape, SSRIs Disrupt Sleep in the Elderly, May Contribute to Dementia. Medscape, 2016.
- Kuwashima, A., A. Virk, and R. Merrill, Respiratory effect associated with use of occlusal orthotics in temporomandibular disorder patients. International Journal of Oral-Medical Sciences, 2019. 18(1): p. 101-109.
- American Academy of Sleep Medicine International Classification of Sleep Disorders Third Edition. 2014, Darien, IL: American Academy of Sleep Medicine.
- Nikolopoulou, M., et al., The effect of raising the bite without mandibular protrusion on obstructive sleep apnoea. J Oral Rehabil, 2011. 38(9): p. 643-647.
- Nikolopoulou, M., et al., Effects of Occlusal Stabilization Splints on Obstructive Sleep Apnea: A Randomized Controlled Trial. J Orofac Pain, 2013. 27(3): p. 199-205.


 Barry Glassman, DMD, has earned Diplomate status with the American Board of Craniofacial Pain, the American Academy of Pain Management, and the American Board of Dental Sleep Medicine. He is also a Fellow of the International College of Craniomandibular Disorders. Among his recent publications are The Effect of Regional Anesthetic Sphenopalatine Ganglion Block on Self-Reported Pain in Patients with Status Migrainosus in Headache, and The Curious History of Occlusion in Dentistry in Dentaltown. He teaches and lectures internationally on orofacial pain, joint dysfunction, and sleep disorders.
Barry Glassman, DMD, has earned Diplomate status with the American Board of Craniofacial Pain, the American Academy of Pain Management, and the American Board of Dental Sleep Medicine. He is also a Fellow of the International College of Craniomandibular Disorders. Among his recent publications are The Effect of Regional Anesthetic Sphenopalatine Ganglion Block on Self-Reported Pain in Patients with Status Migrainosus in Headache, and The Curious History of Occlusion in Dentistry in Dentaltown. He teaches and lectures internationally on orofacial pain, joint dysfunction, and sleep disorders. Don Malizia, DDS, limits his practice to upper-quarter chronic pain and sleep disturbed breathing at the Allentown Pain & Sleep Center in Wilkes-Barre, Pennsylvania.
Don Malizia, DDS, limits his practice to upper-quarter chronic pain and sleep disturbed breathing at the Allentown Pain & Sleep Center in Wilkes-Barre, Pennsylvania.