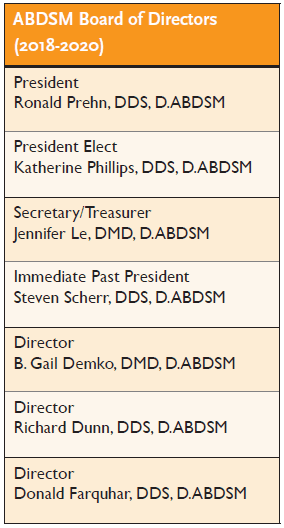
by Jennifer Le, DMD, D.ABDSM, and Ronald Prehn, DDS, D.ABDSM
 Few, if any, sleep practitioners are diffident about the inherent benefits and immense importance of a multi-disciplinary approach when evaluating and treating sleep related breathing disorders (SRBD). Skepticism does arise when qualifications and standard of care enter the discussion. An array of purported credentialing entities has entered the field creating cacophony of confusion. Is all education created equally, and do all credentialing boards abide by similar rigid process standards?
Few, if any, sleep practitioners are diffident about the inherent benefits and immense importance of a multi-disciplinary approach when evaluating and treating sleep related breathing disorders (SRBD). Skepticism does arise when qualifications and standard of care enter the discussion. An array of purported credentialing entities has entered the field creating cacophony of confusion. Is all education created equally, and do all credentialing boards abide by similar rigid process standards?
The American Board of Dental Sleep Medicine (ABDSM) plays a critical role in certifying Dental Sleep Medicine as a distinguished evidence-based profession, as well as fostering collaboration with physicians and other healthcare providers in the treatment of sleep related breathing disorders. Physicians treating obstructive sleep apnea (OSA) can feel confident when they are working with an ABDSM credentialed Diplomate as part of the healthcare team. In order to earn Diplomate status, dentists must first demonstrate competency in their overall knowledge of sleep disorders. Additionally, they must demonstrate the decision making and clinical skills necessary to treat SRBD with oral appliance therapy (OAT), surgical intervention and interceptive orthopedics. The ABDSM diplomate credential is widely respected by physicians, dentists and other healthcare providers as the “gold standard of excellence in dental sleep medicine.”
 ABDSM Achievement
ABDSM Achievement
How did ABDSM achieve this position in our profession? For the last 25 years the profession of Dental Sleep Medicine has been gaining in knowledge through broad based clinical experience and important research. Concurrently, the ABDSM has kept pace by continually raising the certification excellence bar. One of many qualities that sets the ABDSM apart from other boards offering certification examinations is ABDSM’s status as an independent not-for-profit organization.
More recently, the ABDSM certification process has subjected their certification examination to a rigorous, state-of-the-art psychometric test development process, which improves the ability of the exam to accurately discern candidate competency. Through the years, the foundation of the ABDSM certification exam has been peer-reviewed published research. In addition, testing of clinical experience and candidate knowledge of accepted clinical protocols have recently been added to the exam, augmenting what many consider the most accurate and well written certification examination in the field. The examination is now web based and conveniently offered in testing centers throughout the world.
Examination Criteria
The ABDSM Board of Directors works with psychometric professionals and subject matter experts to develop and validate a testing process designed to assess the competency of a dental sleep medicine practitioner. Currently, a licensed dentist may become eligible to sit for the ABDSM exam via two distinct pathways: The Traditional Track (requires submission of prerequisites and case studies for the ABDSM board to review) and the Mastery Track (requires completion of the American Academy of Dental Sleep Medicine (AADSM) Mastery Program offered through the AADSM or an Accredited AADSM Mastery Program Provider). The ABDSM testing model is built on three principles: test standardization, criterion-based testing and equitable difficulty over time. These three principles produce a certification exam that is valid, fair, reliable and defensible.
Test Standardization
The test makeup is based on overall general knowledge of dental sleep medicine and is based on a set of core content areas. These distinct areas of knowledge are weighted according to relevance for the dental sleep medicine provider. This test platform is designed to ensure consistency and fairness in testing by sampling material from each content area, proportional to importance. This contrasts with other testing protocols which have been found to vary wildly in content focus and overall difficulty from one exam session to the next.
Criterion-Based Testing
The ABDSM testing model is criterion-based, which means that all candidates are held to the same standard of competence which is consistent from each exam session to the next. The examination criteria are built on a profile termed the “Sufficiently Qualified Candidate” (SQC), defined as the minimum attributes a sleep dentist must possess to meet established competency standards. After the ABDSM exam testing window has closed, and before the pass/fail standard for that exam has been determined, the performance of each exam question is statistically and critically evaluated. Particular attention is paid to question clarity, fairness, and the ability to successfully distinguish those candidates that meet the standard of competency from those candidates that do not. Any question that performs poorly is not included in the final exam scoring.
In contrast, many other formal examinations use arbitrary standards that are not research based and score on an absolute pass rate of some set percentage of questions answered correctly; while others use normative standards (e.g. grading on a curve). Though popular, these methods set a pass score by using arbitrary criteria that have no relevance to identifying sufficiently-qualified candidates. Criterion-based testing is a proven model for delivering accurate, fair, and consistent results.
Equitable Difficulty Over Time
As our knowledge base increases over time, the examination content must also keep pace. An important design consideration is maintaining a consistent level of difficulty. Exam content, by nature, consists of some material that is more difficult than other material. As old content is replaced with new, the overall difficulty of the exam may also evolve. The method used to develop the ABDSM exam measures the difficulty of each question and adjusts the minimum passing test score to compensate. Unlike applying normative pass/fail standards that alter the passing score (or cutoff point) based on the performance of different groups of candidates, this model adjusts passing criteria based on the inherent difficulty of the exam itself and mitigates concerns about skewed test results that could occur with “easier” or “harder” versions of the test.
Conclusion
The need for consistent standards of care and skilled professionals in the Dental Sleep Medicine field continues to grow as sleep disorders pose growing health risks. As patients, physicians and payers seek dentists who have the competency to provide oral appliance therapy, there will always be confidence in the validation of the ABDSM exam and its ability to accurately identify qualified dentists in dental sleep medicine.





