Dr. David E. McCarty points out that variations in sleep apnea symptoms call for an in-depth and individualized approach to finding the appropriate treatment.
 by David E McCarty, MD, FAASM
by David E McCarty, MD, FAASM
Sleep Apnea. Say those words to a group of physicians or dentists, and then wait a minute. After you’ve let the words sink in, ask the most gregarious person in the room for
a definition.
Chances are, you’ll get a response akin to: “That’s a condition where soft tissues of the back of the throat collapse during sleep, leading to snoring, disturbed sleep, daytime tiredness, and cardiovascular consequences.”
Then everybody in the room will nod, because it sounds like a good explanation. Somebody might even clap, because the phraseology was so good. Your gregarious friend will blush.
Not to be a killjoy, but good as it sounds, this explanation also happens to be wrong. Well, not wrong, exactly. Incomplete may be a better word. And this is where all the trouble starts.
Your gregarious friend appears crestfallen.
Truth be told, the entity commonly known as Sleep Apnea has many “moving parts,” variably present in each individual, making the granular presentation of each case as variable as a fingerprint. Each person experiences Sleep Apnea differently, because the disease is different in every iteration.
Think about that.
Some individuals with this label can’t stay awake. Some can’t sleep at all. Some are heavy. Some are thin. Some have ruinous, catastrophic symptoms. Others don’t notice it. Some snore like a chainsaw. Some are completely silent. Some will die young if they don’t get treatment. Others will die old, of something else, and will never know they had it.
At the end of the day, the label can mean so many things, it flutters at risk of being meaningless.
To say Sleep Apnea is conceptually “complicated” is an understatement, kind of like saying Jesus is “famous.” McKeown et al do a wonderful job of picking apart this complexity in a recent review, a worthy read for anyone interested in this subject. The basic idea is that a floppy airway is just one piece of a larger puzzle, a revelation that helps to explain why a singularly anatomic treatment strategy (like CPAP or oral appliance therapy) doesn’t always work.
Let’s explore that.
In the jargon of the field, a “floppy” airway that’s easy to collapse is said to have a high pharyngeal critical closing pressure, usually designated as a “high Pcrit.“ Anatomic treatment strategies like positive airway pressure therapy and standard mandibular advancement devices tackle this component. When they work well, everyone goes back to your gregarious friend to tell him that he was right after all.
When they don’t work, though, we’ve got some more head-scratching to do. In these cases, it’s helpful to know that there are three other “moving parts” in this complex machine, namely: arousal threshold, loop gain, and upper airway recruitment.
Let’s take a tour.
A person is said to have a low arousal threshold when they’re easy to wake up from sleep. Mild shifts in CO2, mild discomforts associated with increased upper airway resistance and snoring vibrations will wake these folks up. These are the sleep-apnea-insomniacs, with autonomic overdrive, trending towards daytime anxiety and panic symptoms.
On the other hand, other individuals have a very HIGH arousal threshold, meaning they continue sleeping even when struggling to breathe against a closed airway. This can lead to much deeper oxygen desaturations, which drives more end-organ damage.
The arousal threshold is like a volume knob, and it can fluctuate over time. Things like pain, chronic mouth-breathing and psychological trauma can lower it, while some medications and chronic exposure to intermittent hypoxia can make it higher.
The concept of “loop gain” is an engineering term that describes the “twitchiness” of a self-correcting system. How aggressively does the system respond, when a parameter gets out of whack?
Let’s look at an example. If your home furnace has a high loop gain, as soon as the temperature drops below the desired setpoint, the furnace fires up so aggressively that it overshoots the goal, and makes the house sweltering hot, before it shuts off. It won’t come back on again until the house is too cold. Over and over it goes, too-cold alternating with too-hot, never achieving stability.
If control of breathing is like a thermostat, then the CO2 level is the “temperature” that the brain is trying to control. When a breathing pause occurs, CO2 level will rise, and trigger a corrective response: recovery breathing with an arousal from sleep. Those with a high loop gain tend to overdo it, taking several gigantic breaths, driving CO2 down low enough that the respiratory drive is temporarily erased.
Central apnea: it’s nice to make your acquaintance!
The thing about loop gain: it’s fluid over a lifetime, but, as a general rule, it increases with age, and it’s higher with mouth-breathers. Cardiovascular disease, by virtue of introducing a longer circulation time, also contributes to increasing loop gain. For example, if a person has atrial fibrillation, the pump function of the heart is simply less efficient. It takes longer for blood to get around the block. In our thermostat analogy, this would be akin to having the temperature sensor a long way away from the furnace. The delay in message delivery about the status of the system makes for a loping, periodic response, rather than stability.
The final element to consider is upper airway recruitment. This refers to the concept that the upper airway has a resting motor tone that changes between the sleeping state and the waking state. Whereas the concept of high Pcrit imagines a flaccidity to the upper airway (implying a status of “always floppy”), the concept of upper airway recruitment acknowledges that the many muscles comprising the upper airway may be differentially recruited during sleep.
In other words, the muscles aren’t floppy all the time. In fact, these muscles can be retrained, using a strategy called Breathing Retraining Exercises (BRE). The amazing thing? BRE also moves the needle in the right direction for the other “moving parts” of Sleep Apnea, too.
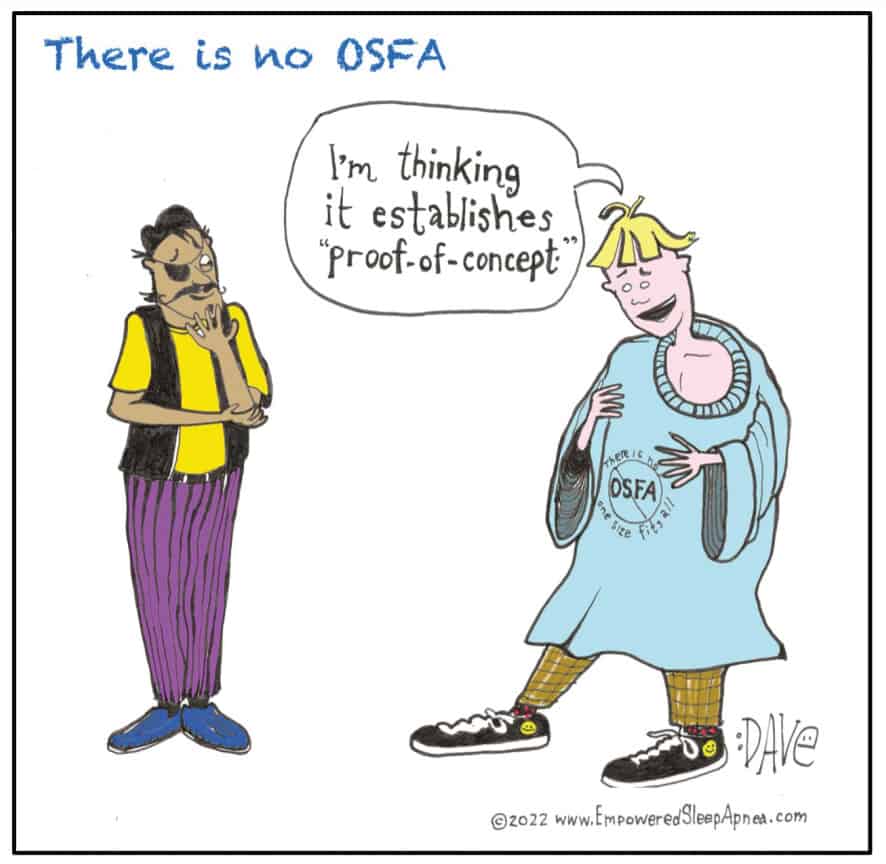
The main point of all of this? There is no One Size Fits All solution to the beast we call Sleep Apnea.
Fortunately, McKeown et al offer a more functional paradigm for Sleep Apnea management called Precision Medicine. Practically, this means deconstructing the functioning phenotypes of disease active in an individual patient, whilst simultaneously providing the right coaching to help that person understand what they might gain from a given treatment, and what they might be missing out on.
There is no OSFA. The complexity of Sleep Apnea demands that we can no longer dedicate ourselves to caring for a “label.”
We owe it to our patients to care for them, as individuals. That’s the human thing to do.
That’s a statement even our gregarious friend would probably agree with.
With variations in sleep apnea causes, it is important to show each patient empathy for their particular kind of issue. Read “They are Not Their Disease: Clinician and Providers Need to Feel That” at https://dentalsleeppractice.com/they-are-not-their-disease-clinician-and-providers-need-to-feel-that/
Recommended Reading:
McKeown P, O’Connor-Reina C, Plaza G. Breathing Re-Education and Phenotypes of Sleep Apnea: A Review. J. Clin Med. 2021, 10,471. https://doi.org/10.3390/jcm10030471


 David E. McCarty, MD, FAASM, is a board-certified Sleep Medicine specialist & co-founder of Empowered Sleep Apnea, a patient-centered educational project designed to enhance patient empowerment and personal agency, whilst navigating the diagnosis of Sleep Apnea. He is co-author (with Ellen Stothard PhD) of Empowered Sleep Apnea: A Handbook for Patients and the People Who Care About Them, and co-host of Empowered Sleep Apnea: THE PODCAST. More information at
David E. McCarty, MD, FAASM, is a board-certified Sleep Medicine specialist & co-founder of Empowered Sleep Apnea, a patient-centered educational project designed to enhance patient empowerment and personal agency, whilst navigating the diagnosis of Sleep Apnea. He is co-author (with Ellen Stothard PhD) of Empowered Sleep Apnea: A Handbook for Patients and the People Who Care About Them, and co-host of Empowered Sleep Apnea: THE PODCAST. More information at