
Essential Technology for Any Dental Sleep Medicine Practice? You Decide!
Interest in Sleep Medicine (SM) and Dental Sleep Medicine (DSM) has grown considerably over the past decade; between 2002 and 2013 the number of articles published about SM/DSM grew from approximately 500 articles to more than 1500 and the trend continues. DSM’s growth has mirrored that of sleep medicine – there is abundant evidence demonstrating high efficacy of oral airway therapy devices (OAT) as an alternative to CPAP therapy for patients who have been diagnosed with mild-moderate Obstructive Sleep Apnea (OSA).
In 2006, the AADSM produced the first systematic DSM literature review and clinical practice parameters but the exponential growth of the field of Dental Sleep Medicine (DSM) demanded an update of the document. In February of 2013 the AADSM brought together a representative cross-section of notable leaders in the field of DSM to more correctly define what constitutes an effective oral appliance for the treatment of sleep disordered breathing based on then-current research and experience. This consensus committee produced a new definition, approved by the Board of Directors of the AADSM in March 2013. (Ramar, 2014) (Scherr, 2014)
Conclusions of the AADSM Report: “Definition of an Effective Oral Appliance”
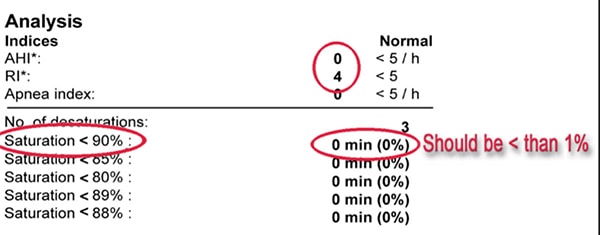
Subsection 5.1 entitled “Purpose of an Effective Oral Appliance” defines comparative efficacy of OAT vs. CPAP as the percentage of patients treated where AHI was reduced to <5 events/hour. Results for mild-moderate OSA: efficacy of CPAP=76% vs. OAT=62%; moderate-severe – CPAP=71% vs. OAT=51%.
If we take a half full look at efficacy of CPAP vs. OAT, the inescapable conclusion is that for all levels of disease, OAT is relatively quite effective (Weaver, 2008) (Chan, 2007). If, however, we allow ourselves to see outcomes from a half empty perspective of treatment failures regardless of method of treatment we are leaving roughly 30-50% of our patients with disease for all levels of disease severity!
Mandibular Advancement vs. Vertical Titration
Subsection 5.2.3 entitled “Protrusion Mechanism” notes that advancement of the mandible is a “key” feature of success with OAT. Surprisingly, the committee also reported that “…no recommendations regarding increased Vertical Dimension of Occlusion (VDO) adjustment were included in the definition”. While the committee failed to deal with the issue of VDO, there is published evidence and a multitude of case reports showing that in select cases, additional VDO may have a stabilizing effect upon the airway thereby increasing OAT efficacy. (Kryger MH, 1989) (George, 2001) In contrast, other studies suggest that increased VDO reduced patient acceptance. (Pitsis AJ, 2002)
An oft-cited study argued that only mandibular advancement “increases cross-sectional area of several segments of the upper airway” whereas increased VDO had a destabilizing effect upon them. (Isono, 1995)
These conflicting outcomes likely identify this as a case-specific issue. In this author’s experience, increasing VDO is often effective especially when the specific risk factors such as obesity, male gender, or a diagnosis of polycystic ovarian syndrome are present in the patient who is refractory to advancement of the mandible.
Currently Available Technology to Assess Oropharyngeal Compliance
If a patient is not responding to treatment with (mandibular) advancement, short of abandoning treatment is there technology available to help improve outcomes? There have been a number of technological advances to help us visualize the airway to better determine site of oropharyngeal compliance leading to OSA. Compliance is roughly equivalent with collapsibility of the airway. Some of the currently available technologies are:
- Drug induced sleep endoscopy (DISE)
- Magnetic Resonance imaging (MRI)
- Computerized Tomography (CT)/Cone Beam C.T. (CBCT)
- Cephalometric radiographs,
- Acoustic Pharyngometry
As with any medical technology, there are certain practical considerations which must be applied to determine whether the specific technology is appropriate for the disease condition & patient being evaluated. The criteria often applied are (Faber, 2003):
- Ease of implementation
- Accuracy and reproducibility
- Cost-effectiveness
- Availability in a clinical setting
Drug Induced Sleep Endoscopy (DISE)
Airway obstruction in obstructive sleep apnea (OSA) can occur at many levels. The principal regions most susceptible to collapse are the palate, hypopharynx, and the retrolingual area; all readily visualized with Drug-Induced Sleep Endoscopy (DISE) and provide useful information about upper airway stability. Although DISE has demonstrated substantial diagnostic validity and reliability, it has associated costs and risks that must be balanced against the potential benefits of the procedure vis-à-vis alternative diagnostic assessment with less cost and risk for harm. (Kezirian EJ, 2010)
Magnetic Resonance Imaging (MRI)
Upper airway MRI images can be useful in identifying soft tissue shapes which may affect airway size and compliance, notably tongue volume (Faber, 2003). MRI is noninvasive and does not expose the patient to ionizing radiation, however, this technique is time-intensive, costly, and not easily convenient for the DSM practitioner. MRI is also not always available for obese patients or those with pacemakers.
Computerized Tomography (CT) and Cone Beam Computerized Tomography (CBCT)
CT is a 2D image which can reveal anatomic risk factors for OSA. Evidence shows that there are significant craniofacial differences between OSA and non-OSA individuals such as size and position of the mandible, size of the posterior airway space, tongue size and length of the soft palate.
The most clinically useful measurements of the upper airway to discern morphological risk factors for OSA are: minimum cross-sectional area of the oropharyngeal region and antero-posterior dimension of the smallest dimension of the airway. While 2D imaging is valuable, the complex shape of the airway is better revealed by 3D images from CBCT which also allows software manipulation of the data volume for sophisticated analysis.
CT & CBCT imaging, although sufficient for establishing if there is risk for airway instability, do not provide insight to a dynamic airway, i.e. are not real-time images so have limited usefulness. Such images require substantial exposure to ionizing radiation, which is particularly problematic with children or when repeat images are needed.
The major disadvantages of Cone Beam CT (CBCT) are perhaps, fourfold: 1) availability; due to the significant cost to acquire this technology, not every clinician will have this readily available when needed and the information (images) are static, not dynamic, so to speak which limits application to an every-day clinical setting, 2) high cost and radiation exposure 3) radiation exposure can be significant because multiple exposures may be needed if we are using it to predict airway response with repositioning, and 4) efficacy of CBCT to predict elevated risk for oropharyngeal instability with CBCT has been done evaluating both the A-P cross sectional diameter and/or air volume at the most compliant point of an airway of the patient with the teeth together. There is no data, currently to assess changes in airway stability with changes in vertical displacement of the mandible. This too degrades the practical application of CBCT in a dynamic clinical setting.
Cephalometric Radiography (CR)
An advantage of CR is that it is very quick, easy and the equipment is quite affordable for most all general and specialty dental offices.
CR has been used to assess mandibular deficiency, soft palate length, position of the hyoid bone and posterior airway space. Mandibular body length alone demonstrated a clinically significant association with risk for OSA. (Riley, 1983) (Scherr, 2014)
Acoustic Pharyngometry (AP)
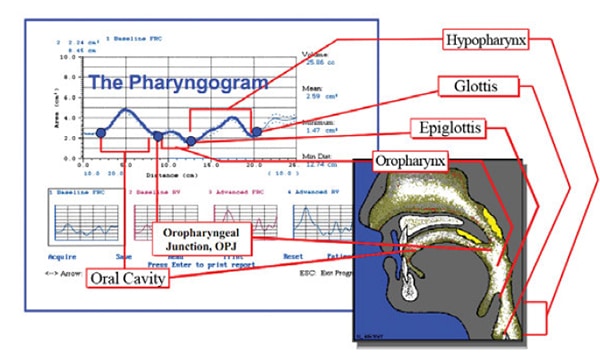
Evidence has shown that sound waves generated and directed towards either a rigid tube like a water pipe or a flexible tube such as an air vent or the muscular walled oropharyngeal airway, will be reflected by changes in impedance caused by changes in the cross-sectional area of that tube. By comparing the incident sound wave with the reflected waves changes in the cross-sectional area, can be accurately calculated. With the emergence of more compact, portable sound-generating units and the development of a proper mouthpiece to deliver the generated sound waves into the oropharynx, AP was now able to be applied to airway analysis and ultimately found application in DSM.
AP also provides useful information when assessing patients at risk for OSA. AP, because of the relative ease of use, reproducibility, availability, and cost-effectiveness, is slowly gaining importance in the clinical setting of the DSM practice to evaluate airway stability of the oropharyngeal cavity using reflected acoustic signals (Gelardi, 2007).
AP efficacy: studies have established a near 100% accuracy in the identification of which level(s) are most susceptible to collapse along the entire length of the airway. There is excellent agreement between data obtained with DISE when contrasted with data obtained from AP. The “data” obtained with AP which provides insight into the location and degree of volume changes of the airway is the Residual Volume (RV) (Terris, 2000).
A recent, and very elegant, study evaluating the predictive value OSA by AP appeared in the Journal of Clinical Sleep Medicine (DeYoung, 2013). It compared the gold-standard of polysomnography (PSG) to the reliability of AP as a viable method to triage patients at risk for OSA. It was concluded that AP “…when analyzed alongside other variables such as gender, age, and neck circumference…provides an objective and simple test with strong independent predictive value for the presence of moderate-to-severe OSA.”
Numerous studies have concluded that AP has sufficient sensitivity and specificity to be clinically useful for airway measurement and assessment. Bradley T. et al maintained that acoustic pharyngometry demonstrates both reproducibility of results and excellent agreement in assessing airway cross-sectional diameter as compared to computerized tomography of the velopharynx (Bradley, 1986)
Concluding Remarks
AP is gaining respect in DSM practices because it provides real-time dynamic data about the potential responsiveness of the oro- and hypopharynx to mandibular repositioning device therapy for the treatment of sleep related breathing disorders. AP accurately and with good reproducibility, estimates cross-sectional diameter of the pharyngeal airway (Brooks LJ, 1989).
AP is not limited because it reveals broader pathways for treatment by enabling the clinician to exploit both x- and y-axes with repositioning. AP is very simple to utilize, non-invasive, and carries no risks for the patient. (Okun, 2010)
It is applicable in both the identification of patients at risk for SRBD who not have been diagnosed but also enhances the treatment of patients diagnosed with OSA who are utilizing a mandibular repositioning device to control their disease. More simply put, assists in “finding an airway” when the traditional approach of minimal opening and advancement alone are insufficiently stabilizing the oropharyngeal airway.
An attempt has been made to objectively review a number of currently available technologies which have been shown to have value in the analysis of airway compliance relative to the treatment of sleep-related breathing disorders with OAT devices. The analysis was done from the perspective of the criteria for practical application in a clinical setting, namely: 1) Ease of implementation, 2) Accuracy and reproducibility, 3) Cost-effectiveness and 4) Availability in a clinical setting (Faber, 2003).
A strong argument can be made that AP, given the modest cost to acquire, ease of use requiring just a few minutes from start to stop in most cases, coupled with the fact that it is non-invasive and virtually harmless, and easily delegated to support staff, should be high on the list of essential technology for the Dental Sleep Medicine practitioner. There are few opportunities in any other area of Dentistry where the demands for such service are so desperately high and failure can mean the untimely demise of a patient. If a single failing Mandibular Advancement Device case can be rendered more effective from the real-time information AP does provide, why would it not seem “essential”?
There are notable disadvantages of AP method: a) the generated sounds waves cannot access any of the airway area above the level or posterior to, the soft palate; that area, however, can be evaluated utilizing a different wave tube, namely the acoustic Rhinometer and has shown applicability in pediatric patients, b) another disadvantage of the AP is that the surrounding soft tissues are not visualized, and c) AP is usually performed with the subject erect during Wakefulness. This “disadvantage” has largely been overcome consequent to the work done by Kamal who showed that employing the Mueller Maneuver when acoustically analyzing the airway of the erect awake patient revealed both level(s) and degree of compliance airway compliance. (Kamal, 2004)
I will attempt to illustrate the practical application of AP in a clinical setting utilizing a clinical case report showing a patient who was refractory to mandibular advancement alone. Through application of information gleaned from AP analysis of the airway, we were able to substantially enhance efficacy of the oral device by increasing the VDO with minimal clinical time and virtually no outside laboratory expense. Although a case reports are considered to be relatively weak scientific evidence, this sort of report can provide a great deal of information and could stimulate future research and hopefully help improve the effectiveness of our treatment for patients who are not responding sufficiently to mandibular advancement alone (Greenhalgh, 2002).
Case Study: Employing Technology in Managing the Mandibular Advancement Device Therapy Patient Who is Not Responding to Advancement
JT is a Dental Sleep Medicine patient whom I have been treating for about 8 years. He is professor at a local community college, hunter and loves being a father to his 3 children…just a wonderful and grateful patient and person. He has had OSA since he was a young man and we have been able to control it well mandibular repositioning devices (OAT). He is now on his 2nd appliance, which we just had made for him, a Respire Blue dorsal appliance.
JT has always done as I have asked and returns regularly for DSM follow-up visits and each time he returns, we provide a HST monitor to check efficacy of his appliance. Each time, with little effort, we have kept respiratory indices well under control until this most recent annual DSM recall.
The last time he returned for his annual progress evaluation, I noted that he looked tired, pleasant as always, not complaining but his countenance was one of someone who appeared not be sleeping well.
Below, is a step-by-step account of why, what, and how we improved his response to mandibular repositioning device therapy.






(right) Q: Is Advancing more going to help?
A: benefit of AR is that it is a real-time test.
This Pharyngogram reflects JT’s maximum effort to protrude (100% of protrusion). Even with maximum advancement, airway stability actually DECLINES from 1.33 cm2 to 1.31 cm2. This phenomenon of a decline in airway stability has been well documented (Hoekema, 2007)






