Dr. Benedict R. Miraglia’s conservative, non-surgical approach to sleep issues of a young patient led to her finally finding a solution to her medical, dental, and sleep problems. Read about her journey to a healthy life free from sleep struggles.
by Benedict R. Miraglia, DDS
Lauren was referred to my office by Dr. Michael Gelb for consultation to explore expansive orthopedic and orthodontic treatment options. Lauren was 14 years old, post orthodontics, with chief complaints of exhaustion and lethargy, dizziness, morning headaches, nausea, difficulty concentrating, microsleeps (seizures have been ruled out), anxiety-induced depression, and drooling at night. She had complained of aches and pains in the mouth for years, with a history of GI issues. An endocrinologist had evaluated her for substandard growth. Lauren had long been a step behind in school and could be defined as obstinate. She had weekly cognitive behavioral therapy which were helpful. Her polysomnogram revealed sleep apnea and a multiple sleep latency test confirmed narcolepsy. She was not a candidate for adenotonsillectomy and a CPAP was prescribed.
Dr. Gelb had diagnosed myofascial pain and TMJoint capsulitis and treated Lauren with day and night appliances. Within a few months she was stabilized and referred to my office.
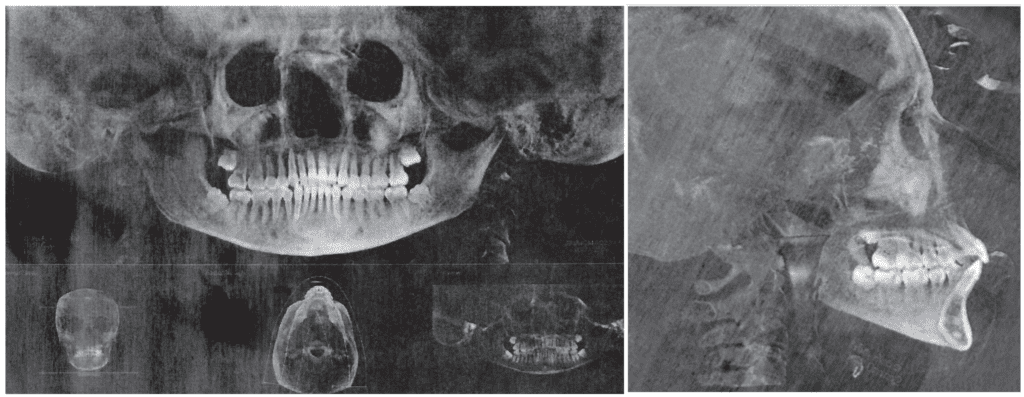
We took a full medical history, confirming the findings listed above, adding mild asthma and noting a history of clenching and grinding her teeth at night. Full orthodontic and dental records to supplement the CBCT volume provided by Dr. Gelb included photographs, transverse measurement, Marchesan Frenum Protocol and a clinical examination. Next: a consultation appointment to discuss the records, findings, diagnosis, and treatment options.
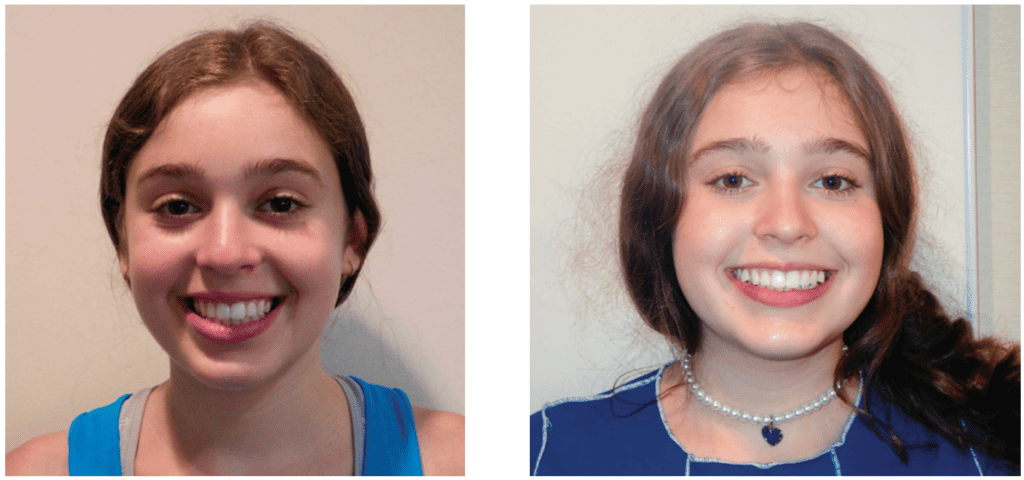
Our goal at the consultation appointment was to help her parents see what we saw: a primary foundation problem. After more than a decade being treated by the medical community for her symptoms, her many medical problems have resulted in a struggling, unhealthy child (Figure 1).

Orthodontics left her with straight teeth but a narrow smile that failed to fill her normal, wide lip line (Figure 2). With our help, Lauren’s parents could see her underdeveloped jaws and appreciate a foundation first, tooth alignment and bite coordination second, treatment choice.
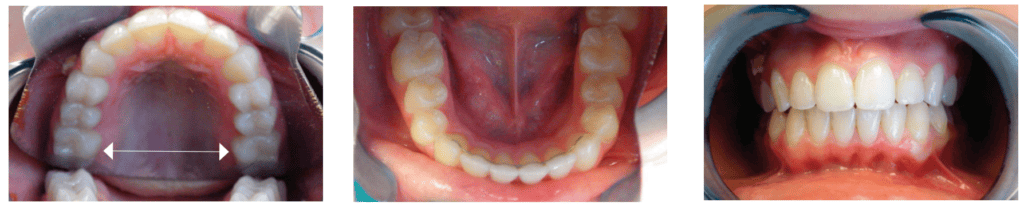
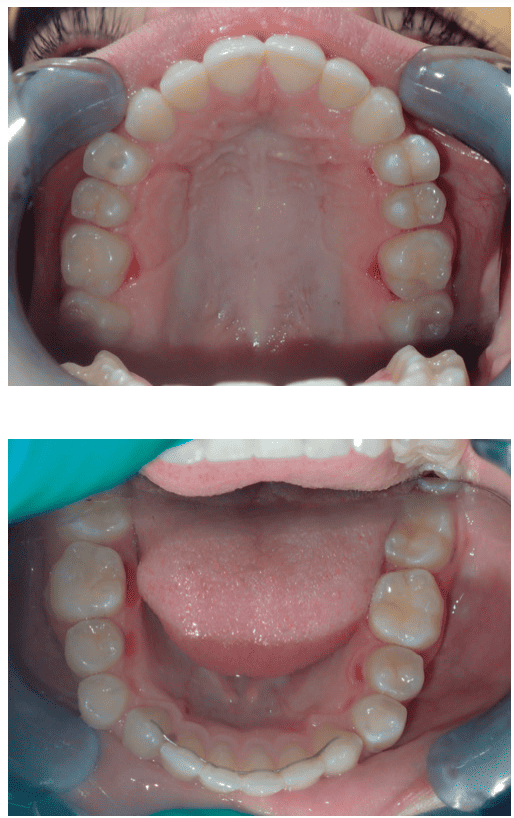
The transverse measurement is the shortest distance at the gumline between primary teeth A and J or secondary teeth 3 and 14. The transverse measurement has its history with Dr. Edward A. Bogue and Dr. James McNamara from the University of Michigan. Dr. Bogue’s research explained that a child of 4 years old with 28mm or less between primary teeth A and J is underdeveloped and will progressively have irregular eruption and crowded teeth (Figure 3). His work provides dentistry the maxim that a child who has little to no spacing between their primary teeth will have crowded permanent teeth. Dr. McNamara’s research on growth and development showed that kids who developed healthy, ideal occlusions without any orthodontic intervention had transverse measurements of 35-39mm by the age of 12, without considering third molars. Dr. Robert Corruccini’s anthropology research shows well developed jaws with 32 teeth in naturally healthy occlusion have transverse measurements starting at 45mm. At age 14.5, Lauren’s Transverse Measurement is 29mm, a barely acceptable number at age 4. The maxilla defines the palate and much of the nose, consequently the more narrow and vaulted the palate, the smaller or more compromised is the nasal chamber. This restriction increases nasal airflow resistance and leads to mouth breathing. The phenotype for OSA is a V shaped arch and a narrow, vaulted palate (Figures 5-8).
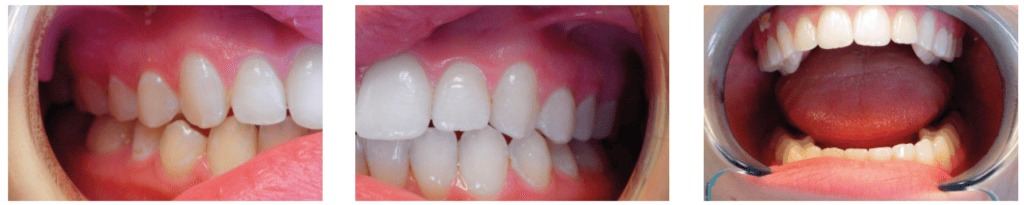
Lauren’s lower arch was narrower than the upper, with no crossbite, leaving insufficient space for her normal-sized tongue. Without considering the size of the arches, a sad perspective would be her tongue is ‘too big.’ Imagine what must happen during function – there is no place for her tongue to go except backwards into her airway – scalloping shows the body’s attempt to keep it forward, pressing it against the teeth (Figure 9). Another common directive is that crossbite is the only indication for expansion. Pre-treatment panoramic and cephalometric radiographs are included (Figures 10 and 11).
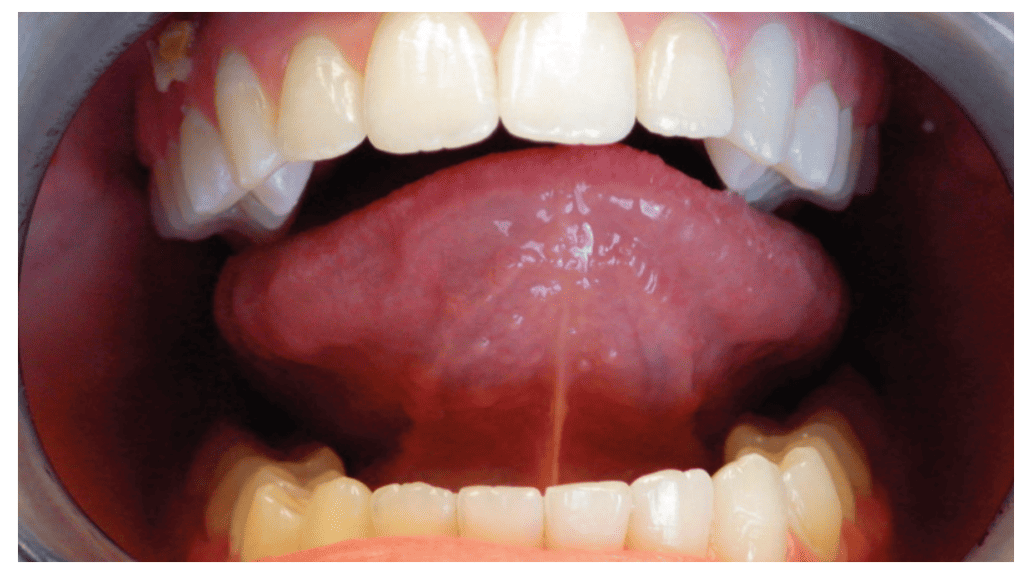
Dr. Irene Marchesan’s Frenum Protocol objectively scores the level of tongue restriction. Her research supports tongue mobility being related to jaw growth and development. The more mobile the tongue, the more developed the jaws are and the more restricted the tongue, the less developed the jaws. Her protocol incorporates measurements, frenum attachment locations, and tongue movements. The 0 (excellent) to 8 (fully restricted) scoring system guides clinicians to recommend revision with a score > 3. Lauren’s score was 5.
Lauren’s 2019 pretreatment polysomnogram (PSG) showed a respiratory disturbance index (RDI) of 9.3 per hour and an apnea hypopnea index (AHI) of 6.7 per hour. Pediatric OSA in non-obese children is a disorder of oral-facial growth.1 Her 2019 multiple sleep latency test (MSLT) results met both criteria for narcolepsy – sleeping in all four opportunities, with short sleep latency, and REM in 3 naps.
Lauren’s school struggles were well documented: trouble getting to school on time, staying awake, managing assignments, and performing well on tests. Both her pediatric pulmonologist and I were asked to provide accommodation letters so school officials could understand her situation.
Lauren’s diagnosis was Class 1 Malocclusion with maxillary and mandibular deficiency, transverse deficiency, lingual frenum and upper labial frenum restrictions, and soft tissue dysfunction. Multiple-level treatment recommendations followed a foundation first, teeth second approach: Upper and lower fixed expanders to address the maxillary, mandibular, and transverse deficiencies, followed by clear aligners to align the teeth and coordinate the bite. During the clear aligner phase, orofacial myofunctional therapy to treat the soft tissue dysfunction and coordinate with frenum releases by an oral surgeon. Nasal hygiene was to be performed daily. Lauren was advised to use a non-steroidal, natural nasal spray several times a day during treatment. Continuous nasal breathing was a primary goal of this treatment plan.
This consultation process concludes with a discussion of the risks and benefits of treatment, alternatives, as well as the option not to treat. Her parents also understood that I was not treating Obstructive Sleep Apnea, ADHD, narcolepsy, insomnia, anxiety, depression, mild asthma, TMJ symptoms, morning headaches and/or any other symptom Lauren had struggled with over the last decade. I was treating her underdeveloped jaws. Lauren’s parents consented to treatment using fixed expanders first followed by CandidPro clear aligners. They also agreed to the orofacial myofunctional therapy with frenum revisions as described. A digital scan was taken and sent to Ohlendorf Appliance Laboratory in St. Louis, MO where maxillary and mandibular fixed expanders were fabricated.
One month later Lauren’s upper expander was placed. Since she was nearly 15, a slow expansion rate was prescribed with her parents making the turns. Four weeks later, the lower fixed expander with a slow expansion rate was added. After nine months, her Transverse Measurement increased from 29mm to 38mm (Figures 12 and 13).
The larger arch form and width increased the space available for the tongue and was a significant foundational increase when compared to pre-treatment (Figure 14). As expected, at this point in treatment the teeth are not well positioned nor is the bite correct. We basically ignore the teeth during foundational growth as the fixed expanders are designed to address the maxillary, mandibular, and transverse deficiencies and not the teeth. After 9 months, Lauren reports that she has been improving in all her symptoms. She states that she is starting to feel better and is excited to transition to clear aligners (Figures 15-18).


At the same appointment the expanders are removed, we took photos and scans to order CandidPro clear aligners. She wore interim Essix clear retainers day and night to ensure perfect fit when the aligners were ready. Lauren was referred to Connecticut Orofacial Myology – one of the skilled team members there worked with her leading up to the frenum revisions and for months afterward.
To follow maxillary and mandibular development, we needed an expansive clear aligner technique to continue the process, wider and forward. CandidPro clear aligners were chosen to align and coordinate the teeth into a healthy, stable, functional, comfortable, and esthetic occlusion. Within a few days, CandidPro posted a treatment plan that met our objectives, with no need for attachments, simplifying the process. An expansive plan removed any consideration of interproximal reduction. We accepted the plan and two weeks later Lauren started wearing her first set of aligners.
Lauren wore 22 CandidPro aligners over 11 months to deliver a wider arch form with excellent tooth alignment and bite coordination. She engaged with the myofunctional therapist and had the lingual frenum and upper labial frenum revised by Dr. Scott Siegel, with therapy afterward to ensure proper healing, mobility, strength, and function. A final set of photographs was taken, and a full interview with Lauren and her parents was conducted to review her symptoms. Lauren had become a day and night nasal breather and her parents reported quiet sleep. She no longer missed school or fell asleep in class. She had achieved A student status without extra help or time.
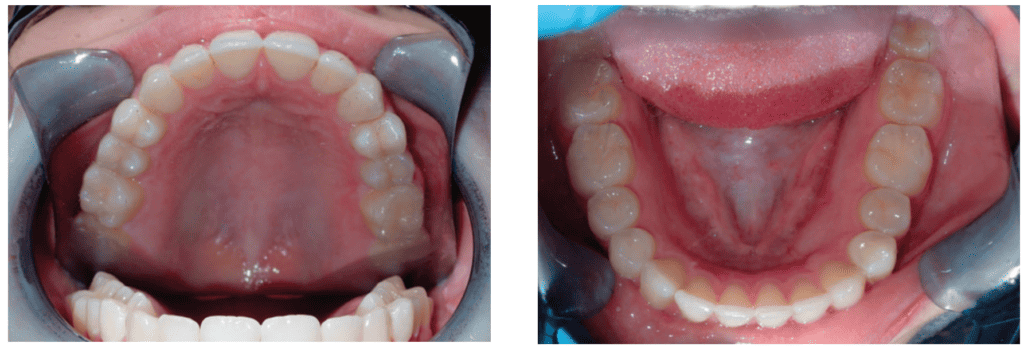
The fixed expanders increased Lauren’s Transverse Measurement from 29mm to 38mm; CandidPro aligners provided an additional 3mm for a final Transverse Measurement of 41mm – a 12mm improvement in space for her tongue (Figures 19 and 20). The frenum release and myofunctional therapy freed, strengthened, and trained the tongue to function properly in its newly developed oral space. Compare Lauren’s senior portrait (Figure 23) to her pretreatment photo – not all results can be objectively measured.
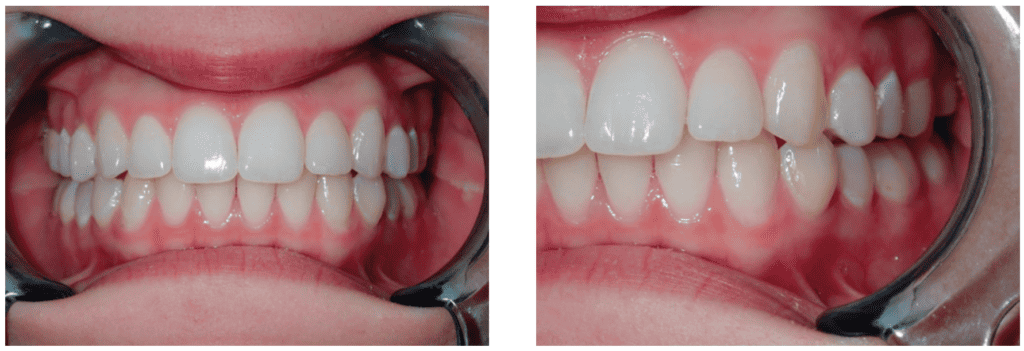

without dark buccal corridors.
After treatment Lauren repeated an in lab PSG and MSLT. Her AHI was 0.4 per hour and a repeat MSLT failed to show any signs of narcolepsy. Lauren’s parents forwarded the new results accompanied with a note saying “Very interesting how she no longer presents with apnea or narcolepsy.”
Lauren benefited from a conservative, non-surgical foundation first, teeth second approach to treatment. Her success was due to a supportive family and a collaborative care approach to treatment, incorporating necessary frenum releases and orofacial myofunctional therapy into her treatment plan. Developing her maxilla and mandible facilitated Lauren returning to nasal breathing as well as delivering an appropriate size chamber for her tongue to properly rest, swallow, speak, and function. After our 20 months of treatment, Lauren is no longer diagnosed with or treated for obstructive sleep apnea, insomnia, narcolepsy, ADHD, morning headaches, anxiety, depression, or any of the medical symptoms she had previously struggled with over the previous decade. Lauren is now over one year post treatment and enjoys living a healthy life free of the long list of struggles that previously held her back from her true potential.
Recently, Lauren shared that she had won first place in a New York State Science competition (Figure 24). The big surprise was that she used flies to show that if their sleep/rest cycle is disrupted, they are not able to perform their daily tasks at the same level as flies that are not sleep disrupted. She was accepted to a top tier college and plans to pursue a career in research.
One way to find out if the patient is able to have a non-surgical approach to sleep issues, is by better screening. Read about that in “Precision Medicine in a Dental Sleep Practice,” at https://dentalsleeppractice.com/ce-articles/precision-medicine-dental-sleep-practice/
- Guilleminault C, Huang YS. From oral facial dysfunction to dysmorphism and the onset of pediatric OSA. Sleep Med Rev. 2018 Aug;40:203-214. doi: 10.1016/j.smrv.2017.06.008. Epub 2017 Jul 6. PMID: 29103943.


 Benedict R. Miraglia, DDS, is a graduate of the State University of New York at Buffalo School of Dental Medicine, and he is a member of the ADA, the AGD, the NYSAGD, and the Ninth District Dental Society. Dr. Miraglia is a graduate of the United States Dental Institute where he learned his non-extraction, expansive orthodontic philosophy. He has been practicing dentistry in Mt. Kisco, New York for 30 years, including 20 years offering interceptive orthodontics. Dr. Miraglia is on the Board of Directors of the American Academy of Physiological Medicine and Dentistry as well as the Northern Westchester Hospital President’s Council. He is widely recognized for his lectures and continuing education courses focusing on craniofacial growth and development related to childhood sleep disordered breathing. Dr. Miraglia is the Chief Clinical Officer for Airway Health Solutions. He has trained thousands of dentists across the globe in all levels of clear aligner orthodontic treatment. Dr. Miraglia is currently the VP of GP Clinical Education at CandidPro.
Benedict R. Miraglia, DDS, is a graduate of the State University of New York at Buffalo School of Dental Medicine, and he is a member of the ADA, the AGD, the NYSAGD, and the Ninth District Dental Society. Dr. Miraglia is a graduate of the United States Dental Institute where he learned his non-extraction, expansive orthodontic philosophy. He has been practicing dentistry in Mt. Kisco, New York for 30 years, including 20 years offering interceptive orthodontics. Dr. Miraglia is on the Board of Directors of the American Academy of Physiological Medicine and Dentistry as well as the Northern Westchester Hospital President’s Council. He is widely recognized for his lectures and continuing education courses focusing on craniofacial growth and development related to childhood sleep disordered breathing. Dr. Miraglia is the Chief Clinical Officer for Airway Health Solutions. He has trained thousands of dentists across the globe in all levels of clear aligner orthodontic treatment. Dr. Miraglia is currently the VP of GP Clinical Education at CandidPro.