Dr. Allen J. Moses says that designing an oral prosthesis to treat OSA takes careful attention to the components of oral physiology.
 by Allen J. Moses, DDS, DABCP, D.ABDSM
by Allen J. Moses, DDS, DABCP, D.ABDSM
Evolutionary Focus
In lower animals the spinal column comes out the back of the head, is oriented horizontally and parallel to the ground. The head is cantilevered off the spinal column. Humans have evolved to an erect posture and the spinal column is vertical to the ground. Humans are bipodal – walk on two legs. Orchestrating balance of the big human head and enlarged brain on top of the spinal column requires coordinated, complex neuromuscular effort. Humans’ survival as a species evolved based on accomplishing this feat with repositioned, reconditioned, rebuilt, redesigned, miniaturized and in many cases less-capable, parts designed for olfaction, mastication, swallowing, hearing, breathing, and conditioning of inspired air. “Sleep Dentistry,” concerned with anatomic management of Obstructive Sleep Apnea (OSA) must direct stringent attention to the unique human evolutionary combination of foodway and airway. The design of an oral prosthesis to treat OSA by repositioning the anatomic components of the mouth, tongue, hyoid bone, neck musculature and achieve pharyngeal airway dilation and stenting is the subject of this article.
Pharynx
The human pharynx is a three-dimensional muscular tube lined with mucus membrane downstream from the mouth. It extends from the soft palate to the epiglottis. The anterior of the oropharynx is formed primarily by the soft palate and rounded tongue that has a 90 degree bend so 2/3 is horizontal and the posterior 1/3 is vertical. Behind the tongue at the anterior of the pharynx is a hole between the bottom of the soft palate and the upper edge of the epiglottis by which the mouth transcends into the pharyngeal tube (see figure 1). The pharynx is classified as non-intranarial because its design deflects food around the epiglottis into the esophagus while air passes into the larynx. This arrangement explains the combined foodway and airway, unique to humans. The posterior oropharyngeal wall is comprised of the superior, middle, and inferior constrictor muscles.
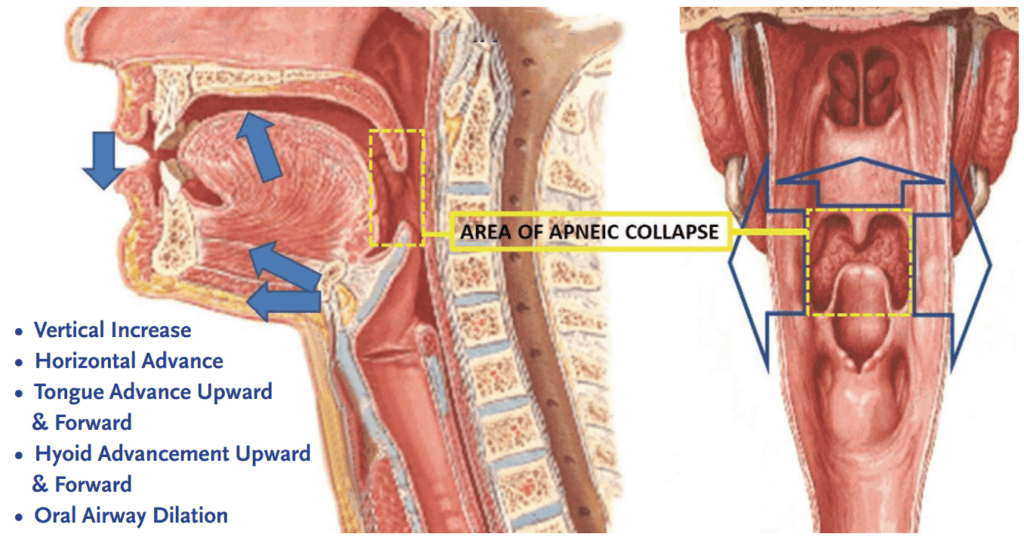
As a result of the nonintranarial arrangement, adult humans cannot breathe and swallow simultaneously. The positive evolutionary development is the ability to speak. The negative consequences are choking, snoring and obstructive sleep apnea (OSA). In most obstructive sleep apnea patients, the collapse or narrowing during sleep occurs in the retropalatal and retroglossal areas between the upper margin of the soft palate to top of the larynx. OSA occurs when the luminal cross-sectional area of the upper airway collapses during inspiration, at or below the level of the soft palate and above the epiglottis. The pharynx is the only collapsible segment of the human respiratory tract.
The human pharynx is unique among mammals because it is not supported by or attached to any bone and functions as a shared airway and foodway. Pharyngeal airway patency is maintained by two counteracting forces: the activity of the upper airway muscles which dilate and stiffen the airway, and negative intraluminal pressure. Atonia of the tongue and airway muscles during OSA reduces intraluminal pressure. Narrowing at the retropalatal region is associated with a further decline in intraluminal pressure during inspiration. Increases in nasal resistance will produce greater negative intraluminal pharyngeal pressure and reduced pharyngeal cross-sectional area. Airway dilation by increasing the pharyngeal volume such as in oral sleep appliances decrease intraluminal pressure
During nasal breathing with the mouth closed, the base of the tongue is in contact with the palatal mucosa of the soft palate. Mouth opening destabilizes the airway by freeing the mucosal contact of the tongue and soft palate allowing the freely moving soft palate to move posteriorly and compromise the pharyngeal airway.
Jaw posture also influences the size of the upper airway. Opening the jaw slightly (rest position for example) increases tongue space in the oral cavity. Progressive mandibular opening leads to posterior movement of the genu of the mandible. More movement causes the tongue and hyoid apparatus to move posterior and narrow the pharynx.
Hyoid
The hyoid bone is unique to humans. It is the only bone intimately connected to the pharynx. It is a floating bone at the base of the tongue, suspended between the temporal bones and the sternum by a series of muscles and ligaments. It is the center of action for most movements of the pharynx. The hyoid bone maintains the posture of the head with complex connections between the mandible and the cervical spine. It supports the tongue which sits above it and holds up the larynx which hangs below it.
The position of the hyoid bone is determined by the status of the eleven muscle attachments affixed to it.1 Muscles attached to the hyoid bone include geniohyoid and genioglossus, capable of moving the hyoid in anterior and superior directions. Changes in hyoid position tend to relate to changes in mandibular position and because of its unique anatomical position it also has a vital role in maintaining upper airway patency and dimension. Neck flexion changes the position of the hyoid bone, altering the anatomic relationships of other muscles attached to it.
Positioning and coordination of the hyoid, the tongue, jaws, cervical vertebrae, and larynx requires frequent intermittent adjustments during breathing, speech, swallowing, mandibular function, and apnea episodes. Maintaining head balance during this constant repositioning and coordination of changing function requires tremendous neurologic circuitry.
The position of the hyoid changes particularly in mouth breathers with their low tongue position. The lower the hyoid, the more forward is the head position on the spinal column and the lower the tongue, the smaller the pharyngeal airway. The largest oropharyngeal airway is created with nose breathing, lips sealed, dorsum of the tongue as far forward as possible and sealed against the hard and soft palate.
The tongue and hyoid must coordinate as the mandible moves posteriorly in relation to the other craniofacial structures or it would encroach on the airway and impinge respiratory function. The patency of the upper airway is preserved by inferior and posterior positioning of the hyoid apparatus as is seen in Class II subjects. The hyoid bone in Class III subjects is positioned in a more anterior position.2 Variations, however, are to be seen in both upper and lower oropharyngeal widths and posture of the tongue and hyoid bone position in all growth patterns.3
Variability of Pharyngeal Muscle Activation and Coordination
There are more than 20 skeletal muscles surrounding the pharyngeal airway.4 Medial pterygoid, tensor palatini, genioglossus, geniohyoid and sternohyoid promote a patent pharyngeal lumen by dilating the airway and stiffening the airway walls. They regulate the position of the soft palate, tongue, hyoid apparatus, and posterior-lateral pharyngeal walls.
Other muscles can have antagonistic effects on the pharyngeal wall. Levator palatini and superior pharyngeal constrictor narrow the retropalatal airway. Glossopharyngeus and palatopharyngeus dilate the airway in the retropalatal area. Extrinsic tongue muscles genioglossus and geniohyoid protrude the tongue – hyoglossus and styloglossus are tongue retractors. Pharyngeal muscles can have different effects when activated individually than when activated in concert.5
The same pharyngeal muscles can play a role in such disparate activities as breathing, swallowing, and speaking. Activation of a given muscle can have different effects on the airway depending on what other muscles are simultaneously doing and their precise anatomic arrangements at the time of activation. The ability of a given muscle fiber to produce different mechanical effects may be due to changes in muscle fiber orientation with concomitant changes in airway size and shape.6 Studies have also shown that a particular pharyngeal muscle may have different mechanical effects on the airway depending on the size of the airway at the time of muscle activation.7,8
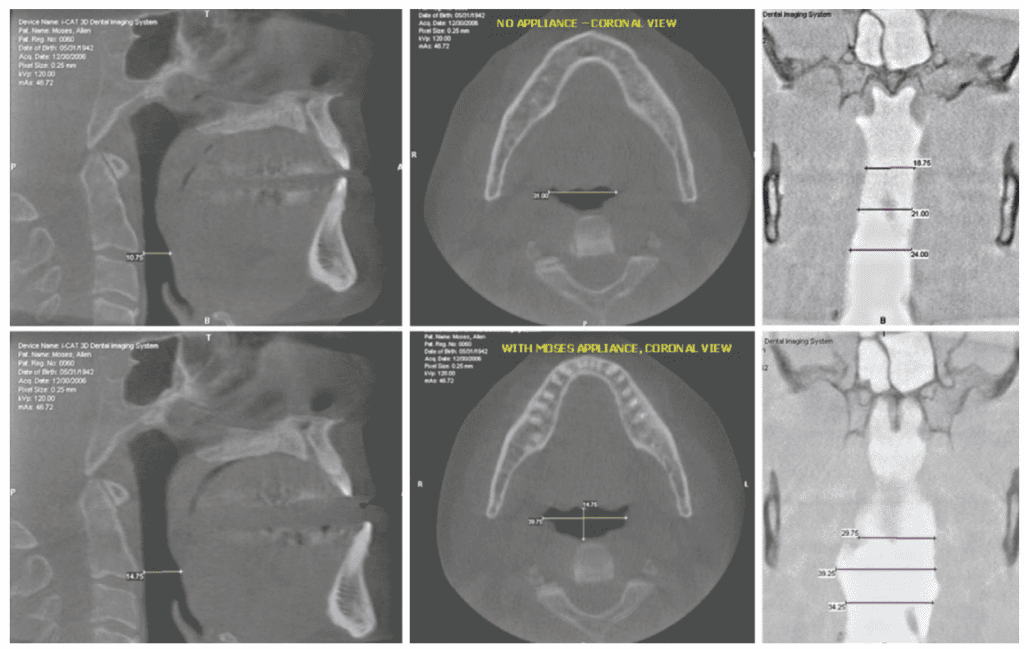
Mandibular repositioning devices increase airway size more in the retroglossal than in the retropalatal region because they advance the mandible and consequently pull the tongue forward.9,10 Another study has shown that mandibular repositioning appliances may in some cases increase cross-sectional area in the retropalatal as well as retroglossal region. The increase in the retropalatal area was mostly in the lateral dimension.11 This suggests that dilation of the oral airway by oral sleep appliances may be more complex than simply pulling the tongue and soft palate forward, the mechanical adjustment mechanism found on most oral sleep appliances.
That the neurologically coordinated movement of over 20 muscles moving in multiple directions with unpredictable firing sequences anchored and guided by the irregular, asymmetric shapes of the hyoid bone, condyles and glenoid fossae should move in tandem and in a straight unidirectional dimension set arbitrarily in a dental lab is contrary to any known anatomic principles.
Finite Element Modeling (FEM) is a means to study complex mouth movements and muscle activation whose origin is in the temporomandibular joint. The mouth is an important human motion system whose positioning is essential in regulating airway volume. A wide range of functional and parafunctional movements are performed many times during the course of a day that are multidimensional rotation and translation.12 Mandibles, with two joints that each function in synchrony with cartilaginous discs, produce many movement patterns. The six muscle activation patterns shown by Sag13 et.al. were each different, asymmetric, unpredictable, and multidimensional.

Unidirectional mechanisms neither capture nor replicate biologic movement. Research into innovative methods for titrating the interarch jaw relationship for oral sleep appliances is warranted.
Discussion
Optimal pharyngeal dilation is a soft tissue phenomenon determined by the coordinated functioning of the mandibular condyles, articular discs, the hyoid bone, ligaments, muscles, and nerves. Stenting this coordinated effort position is difficult to predict precisely because it is a soft tissue stance. A close approximation to this stance position can be guessed at, stented with an oral appliance, and measured non-invasively by polysomnographic study. But polysomnography cannot predict how close that stent is to optimal performance. What direction and how much more or less the clinician must go to achieve greater airway dilation is an unanswered question. There are two means of addressing sleep apnea treatment: (1) make more room in the mouth for the tongue, and (2) dilate the pharynx open.
- Human jaw movement can be either multidimensional or asymmetric and is usually both simultaneously.
- There are recognized anatomic, biological, ergonomic and physiological principles of oral appliance design to establish appropriate vertical, antero-posterior and lateral support in a stabilized position of the dental arches that optimally enlarges the oral airway, prevents its collapsibility, comfortably supports the TMJ, muscles, nerves, and ligaments, facilitatating physiologic tongue position against the hard palate, closed lips, and nasal breathing.
- Optimal airway volume appears to be a multidimensional position. To initially achieve optimal airway dilation and stenting, the dimensions of vertical, lateral, protrusive and slant must be factored into positioning.
- Unidirectional movement does not appear to be the way to achieve optimal airway and stenting.
- Built-in mechanical expansion mechanisms are unidirectional, never having concurrent multi-dimensionality, almost universally horizontal, very rarely vertical or programmed for asymmetric movement.
- Built-in adjustment mechanisms in oral sleep appliances are not specifically pre-calibrated for the direction necessary to achieve optimal airway dilation/stenting.
- Current mechanical adjustment mechanisms consisting of tubes, straps, set-screws, rubber bands, hinges, hooks, and springs are unidirectional and do not replicate human condylar movement.
- If the position of optimal airway dilation and stenting were achieved at the initial fitting, a mechanical adjustment mechanism would be unnecessary.
- Most conventional oral sleep appliances do not employ ergonomic principles that integrate the biomechanical elements of the human oropharyngeal system into design and function to optimize overall system performance. Examples of non-ergonomic appliances are those with wires or hardware that prevent the tongue from resting on the palate, those with restrictive anteriors preventing the tongue from reaching the lips, or those whose vertical height in the anterior is so great that the patient cannot comfortably close their lips.

Conclusion
Mechanically adjustable oral sleep appliances are still in a primitive state of scientific development. Unidirectional mechanisms such as screws, tubes, hooks, springs, hinges, and rubber bands neither capture nor replicate biologic movement. Research into innovative methods for titrating the interarch jaw relationship for oral sleep appliances is warranted.
Being a collapsible tube, more expansion of the pharynx in one direction does not always predict greater dilation; it may result in less dilation. A clinician can keep guessing that more advancement in one direction is better, but it may be more conservative to introduce and manipulate more variable dimensions by just starting over.
An oral sleep appliance that can easily remade from scratch, such as one generated by computer printing from electronic scans, may be more practical, more biologically appropriate, and have a stronger scientific basis than those built with unidimensional adjustment mechanisms.
This article by Drs. Allen J. Moses, Elizabeth T. Kalliath, and Gloria Pacini, RDH, shows the evolution of oral physiology and apnea. Read about how the science behind OSA has evolved here: https://dentalsleeppractice.com/ce-articles/evolution-human-oral-airway-apnea/.
- Auvenshine RC, Pettit NJ. The hyoid bone: an overview. Cranio 2020;38:6–14.
- Battagel JM, Johal A, et.al, Changes in airway and hyoid position in response to mandibular protrusion in subjects with obstructive sleep apnea. Eur J Orthod; 1999;21:363-76
- Adamides IP, Spryopolous MN. Hyoid bone position and position in Class I and Class III malocclusions. Am J Orthod Dentofacial Orthop.1992’101:308-12
- Netter F. “Atlas of Human Anatomy”2 ed Novartus, E Hanover NJ
- Schwab RJ, Kuna ST, Remmers JE. “Anatomy and Physiology of Upper Airway Obstruction” in Kryger, Roth Dement, Principles and Practice of Sleep Medicine; 4 ed; Elsevier Saunders; Philadelphia
- Schwab RJ, Kuna ST, Remmers JE. “Anatomy and Physiology of Upper Airway Obstruction” in Kryger, Roth Dement, Principles and Practice of Sleep Medicine; 4 ed; Elsevier Saunders; Philadelphia
- Kuna ST, Vanoye CR; Mechanical effects of pharyngeal constrictor activation on pharyngeal airway function. J Appl Physiology;1999;86:411-417
- Kuna ST, Brennick MJ, Effects of pharyngeal muscle activation on area-pressure relationships. Am J Resp Crit care Med 2002;166:972-977
- Bennett LS, Davies RJ. Stradling JR.Oral appliances for thefor the management of snoring and obstructive sleep apnea. Thorax, 1998:53 (suppl 2):558-64
- Ryan CF, Love LL, Peat D. et.al. Mandibular advancement oral appliance therapyfor obstructive sleep apnea: effect on awake caliber of the velopharynx. Thorax 1999; 54:972-77
- Liu Y, Zeng X, et.al. Effects of a mandibular positioner on obstructive sleep apnea. Am J orthod Dentofacial Orthop. 2000: 118:248-56
- Drake R, Vogl W, Mitchell A. “Gray’s Anatomy for Students” ed3. 2014 London, Churchill Livingstone
- Sagl B, Schmid-Schwap M, Piehslinger E, Kundt M, Stavness I. A dynamic jaw model with a finite-element Temporomandibular Joint, Frontiers in Physiology; v10:2019, 1156-67
 Allen J. Moses, DDS, DABCP, D.ABDSM, was in private dental practice for 48 years in Chicago Illinois and assistant professor at Rush University Medical School in the Department of Sleep Disorders and Research for 13 years. He holds three US Patents for intraoral sleep devices and a Patent Pending for a shim system for registering the posterior interarch jaw relationship for intraoral sleep appliances. He was a member of the United States Food and Drug Administration Dental Products Panel for 10 years, has authored a book on temporomandibular disorders and over 30 scientific papers on TMDs and sleep dentistry. He was book review editor of Cranio for 10 years.
Allen J. Moses, DDS, DABCP, D.ABDSM, was in private dental practice for 48 years in Chicago Illinois and assistant professor at Rush University Medical School in the Department of Sleep Disorders and Research for 13 years. He holds three US Patents for intraoral sleep devices and a Patent Pending for a shim system for registering the posterior interarch jaw relationship for intraoral sleep appliances. He was a member of the United States Food and Drug Administration Dental Products Panel for 10 years, has authored a book on temporomandibular disorders and over 30 scientific papers on TMDs and sleep dentistry. He was book review editor of Cranio for 10 years.


