Table of Contents
Does New Legislation Mandate TMJ Treatment in your State?
by Rose Nierman
Would medical reimbursement help your practice increase both the number of TMJ Disorder (TMJD) cases you treat and the revenue per case? If so, you may be in luck because the Affordable Care Act (ACA), commonly known as Obamacare, has prompted close to 70% of US states to mandate this coverage!
With so much opportunity for reimbursement, I cringe when I hear about dental practices eating up patients’ dental insurance by billing the wrong insurer when the treatment may be medically necessary.
Prior to the Affordable Care Act (ACA), 20 States mandated treatment of TMD. My research has uncovered 34 states that either have coverage in their “Benchmark Plan” or have deemed “TMJ” to be an Essential Health Benefit (EHB). The ACA’s improvements for TMD coverage doesn’t stop there! Some of the states that had already mandated coverage have enhanced rules or have eliminated barriers such as dollar limitations, though a few states continue to allow such limits.
TMD Billing Rules
- You’ll be asked by the medical insurer to demonstrate that TMD treatment is medically necessary. A SOAP type narrative report showing the patient’s subjective complaints, objective exam findings, assessment and plan is the most common format for medical necessity. Include the ICD diagnosis codes in your narrative report to corroborate medical necessity.
- Verify pre-authorization rules and precise coverage for each policy. Confirm every procedure code you expect to bill during a verification phone call and let the insurer know the expected length of treatment.
- Physical therapy procedures may require that a Registered Physical Therapist perform the services. I make it a rule to ask about this during the verification process.
- When the patient does not have out-of-network benefits, request a GAP exception using the “network insufficiency rule.”
- Across the markets and plans examined, Durable Medical Equipment (DME) is an Essential Health Benefit in 49 states. As a rule, sleep apnea appliances are categorized as DME and, for this reason, are covered! TMD appliances are considered DME by some commercial carriers but not by Medicare.
- Remember, even if your state does not mandate TMD, many insurance carriers cover exams, radiographs, TMJ orthotics or appliances and follow-up visits so it’s well worthwhile to verify each plan. You may also want to check into your state’s nondiscrimination statute regarding health care providers and if TMJ treatment legislation is pending.
TMJ Treatment State Examples of Coverage
Each state has a Benchmark Plan connected to the ACA that “sets the bar” for other health plans in your state. With up to 34 states having different mandates, we can’t list them all, but here are a few examples of some of the new state-specific Benchmark Plans. If your state didn’t make the example list, don’t worry, just contact us and we will help you understand where your state stands.
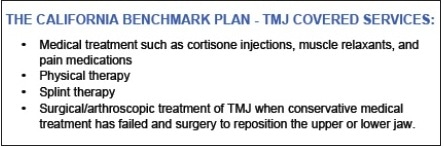
California: Covers TMJ surgical, diagnostic and medically necessary procedures:
 Florida: Since 1996, Florida has required that surgical and diagnostic services related to the temporomandibular joint and the jawbone must be covered, when medically necessary. Now, payment for splints for Temporomandibular Joint (TMJ) Dysfunction is an Essential Health Benefit.
Florida: Since 1996, Florida has required that surgical and diagnostic services related to the temporomandibular joint and the jawbone must be covered, when medically necessary. Now, payment for splints for Temporomandibular Joint (TMJ) Dysfunction is an Essential Health Benefit.

Mississippi: The MS Benchmark Plan limits TMJ Surgery/Diagnostic Services and removable oral appliances for TMJ to $5,000 Lifetime Maximum Benefits.”
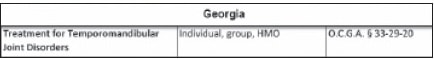
Georgia: TMJ treatment is an Essential Health Benefit. The policies I reviewed have coverage of “Treatment of temporomandibular joint syndrome (TMJ) or myofacial pain, including only removable appliances for TMJ repositioning and related surgery and diagnostic services.”
 Illinois: State law mandates coverage as an Essential Health Benefit.
Illinois: State law mandates coverage as an Essential Health Benefit.
 Washington State: As an EHB, “TMJ Treatment covers abnormal range of motion or limitation of motion of the TMJ; arthritic problems with the TMJ; internal derangement or pain in the musculature associated with the TMJ.”
Washington State: As an EHB, “TMJ Treatment covers abnormal range of motion or limitation of motion of the TMJ; arthritic problems with the TMJ; internal derangement or pain in the musculature associated with the TMJ.”
“Healing is a matter of time but it is also sometimes a matter of opportunity” – Hippocrates
In treating sleep patients, you will often uncover problems they have with TMD or using the device you provide will result in some jaw pain. Now you know that coverage might help you and your patient deal with this! Get prepared for this conversation and you’ll be ready to give better service to your patients.
For more information, feel free to contact me through http://www.dentalwriter.com/ for a TMJ Treatment Mandate Fact Sheet for your State.



