 There are many signs and symptoms to look for in our patients that are indicative of Sleep Disordered Breathing (SDB), but what signs and symptoms could we be missing? We can simply ask our patients how well they’re sleeping, but when answering that question; many patients won’t consider that they may be suffering from the most common form of SDB, Obstructive Sleep Apnea (OSA). The typical patient does not fully understand the consequences of untreated OSA, so in this article, I will discuss the visual indicators of OSA to look out for that could potentially save your patients’ lives, and reiterate that dentists are at the forefront for identifying and treating OSA with oral appliance therapy. I have included findings from an internal analysis I conducted in my practice that supports these visual indicators as indicative of OSA.
There are many signs and symptoms to look for in our patients that are indicative of Sleep Disordered Breathing (SDB), but what signs and symptoms could we be missing? We can simply ask our patients how well they’re sleeping, but when answering that question; many patients won’t consider that they may be suffering from the most common form of SDB, Obstructive Sleep Apnea (OSA). The typical patient does not fully understand the consequences of untreated OSA, so in this article, I will discuss the visual indicators of OSA to look out for that could potentially save your patients’ lives, and reiterate that dentists are at the forefront for identifying and treating OSA with oral appliance therapy. I have included findings from an internal analysis I conducted in my practice that supports these visual indicators as indicative of OSA.
SDB Symptoms Overlooked
 As dentists, we see our patients more regularly, and for longer periods of time than most other healthcare professionals. During your patients’ routine dental visits, it is important that not only we as dentists but our team members be on the lookout for both the obvious and not-so-obvious signs and symptoms. The obvious include reported snoring and choking/gasping during sleep, daytime fatigue, large neck circumference, and retrognathia.
As dentists, we see our patients more regularly, and for longer periods of time than most other healthcare professionals. During your patients’ routine dental visits, it is important that not only we as dentists but our team members be on the lookout for both the obvious and not-so-obvious signs and symptoms. The obvious include reported snoring and choking/gasping during sleep, daytime fatigue, large neck circumference, and retrognathia.
So what are some of the not-so-obvious signs and symptoms that we may be overlooking?
Some predictions of OSA probability include bruxism, abfractions, enlarged tongue size or a vaulted palate. The first example, bruxism, may be a way for the brain to attempt to reopen the airway in an unconscious state. Frequently, a patient who grinds their teeth at night has sore or clicking jaw joints, or flat, worn-down teeth. On the other hand, symptoms of bruxism might even be far less obvious, including earaches or sensitive teeth. Dentists need to be on the lookout for all symptoms and conditions beyond abfractions that might signal grinding and an even deeper problem. Evaluating tongue and palate size, uvula (elongated/battered) and airway space takes only minutes and can easily become standard in a routine dental exam.
Positive Intraoral Findings
As seen in the Summer 2016 issue of Dental Sleep Practice, there are many intraoral findings that strongly suggest a patient at high risk for some form of SDB. The question is: what do we do with these findings?
After dental school, we are immersed in the mindset of prevention, biannual dental hygiene appointments to prevent periodontal disease, placement of dental sealants to prevent caries, interceptive orthodontics and the list goes on. So why not prevent or reduce the risk of hypertension, cardiovascular disease, diabetes, stroke, and other conditions that are linked to OSA? In my opinion, as well as others’ opinions, we need to take a strong stand and become more active in assisting our medical colleagues in identifying potential patients at risk. Remember, early treatment is key to preventing the development of worsening symptoms and dangerous conditions.
To illustrate the power of your clinical judgment, I engaged in an internal analysis of patients that I identified with any of the indicators listed in Table 1. In 2010, I screened my patients for the visual indicators listed in Table 1 and referred patients with positive findings to a local sleep center for further evaluation.
After writing 51 consecutive referrals, I decided to evaluate how many patients got tested and what the outcome was. Out of those 51 referrals, 21 got tested with a full-night PSG study. What was interesting is that only one patient (arrow) did not have an AHI greater than 5 (dotted line) (figure 1).
I decided to repeat the same process in 2011, and out of 55 consecutive referrals, 26 got tested with a full-night PSG study. This set showed two patients (arrows) that did not have an AHI greater than 5 (figure 2).
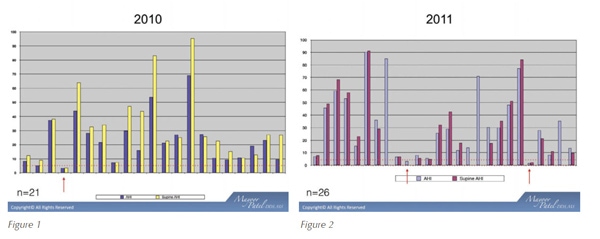 The findings from this internal analysis prove to be very powerful in that these visual indicators during our oral examination can help identify patients suffering from OSA, without considering age, BMI, medical history, gender, or even sleep questionnaires (Berlin, Epworth Sleepiness Scale). If we add these visual indicators to our tool box, more patients can be identified and treated for OSA.
The findings from this internal analysis prove to be very powerful in that these visual indicators during our oral examination can help identify patients suffering from OSA, without considering age, BMI, medical history, gender, or even sleep questionnaires (Berlin, Epworth Sleepiness Scale). If we add these visual indicators to our tool box, more patients can be identified and treated for OSA.
Expand Your Patient Pool
The ability to efficiently communicate with your medical community is crucial, not only to a successful practice but to ensure that our patients get tested and that comorbidities are addressed. Where I see many of my dental colleagues struggle in this arena is in building relationships with local sleep physicians. We keep these relationships intact is by consistently communicating with physicians. Our system is very efficient in that we enter the patient symptoms, clinical findings, assessment, and plan into DentalWriter software and share our cloud-based narrative reports with our mutual patients’ physicians. My staff also sends progress reports with post-treatment AHI’s which helps to promote awareness of the successes we have with OSA and TMD oral appliances. All of our physician reports are in a “medical-model” format and have proven to be essential to developing and maintaining referrals and relationships.
As we all know, SDB can lead to many secondary health conditions, which means treatment is essential. While we can ask our patients if they snore until we’re blue in the face, we might not get the answers we need until we can spot those commonly overlooked signs and symptoms of OSA. Dentists continue to remain in a unique position to screen patients for SDB, so take charge of your practice through continuing education and expanded screening tools for SBD.
