Excessive daytime sleepiness can be a lifetime disorder. But with awareness and early detection, you can help your patients awaken to a healthier life. Read the details about narcolepsy in this article by Dr. Jyotsna Sahni.
 by Jyotsna Sahni, MD
by Jyotsna Sahni, MD
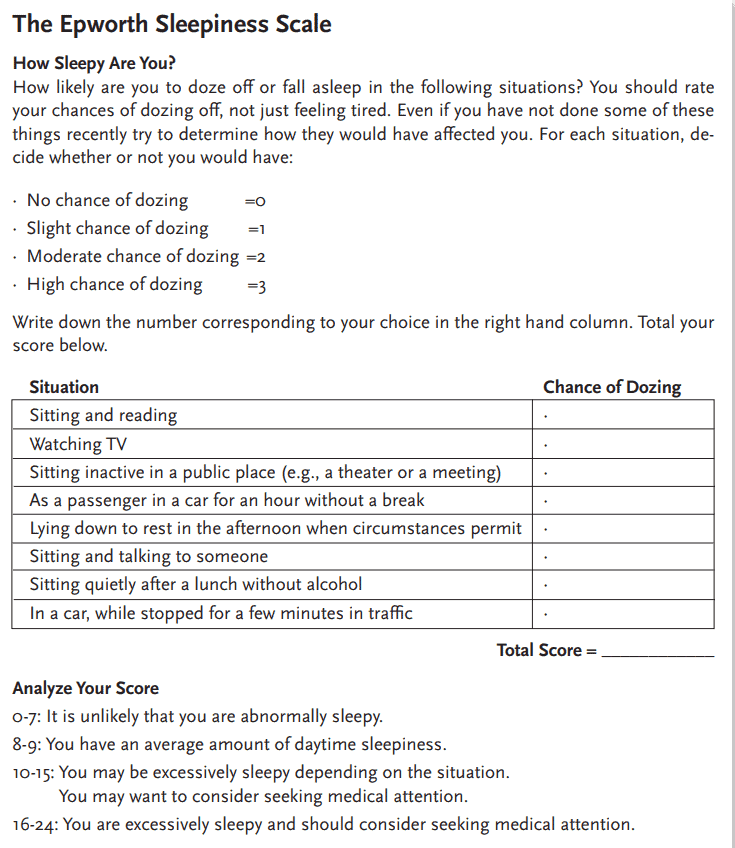
Narcolepsy is a rare neurologic disorder that is characterized by excessive daytime sleepiness. “Sleep” attacks, overwhelming episodes of sleepiness, may occur. The Epworth sleepiness scale score is a validated test that is frequently used to determine sleepiness. Scores vary from 0–24 and are based on likelihood of being sleepy in eight different clinical scenarios. Scores greater than 10 are considered excessive daytime sleepiness and most patients with narcolepsy show a severe amount of sleepiness with scores greater than 18.
Prevalence
Narcolepsy occurs in one per 2,000 people. Its age of onset varies from early childhood to the fifth decade with a peak around the second decade. The delay from symptom onset to diagnosis is typically very long, about 10-12 years. It occurs slightly more in men than women.
Symptomology
In addition to excessive daytime sleepiness, it has several other symptoms associated. These include sleep paralysis which is an inability move that occurs upon awakening from sleep or upon falling asleep. It can last a few seconds to a few minutes. Understandably, it can be frightening.
Sleep paralysis is also often seen in association with hypnagogic or hypnopompic hallucinations. These are vivid dream-like hallucinations that occur upon falling asleep or awakening from sleep, respectively. They are sometimes frightening, have a surreal quality, and can either be very vivid and detailed or sometimes just consist of shadowy figures or shapes.
Cataplexy is an abrupt and reversible decrease or loss of muscle tone, frequently provoked by strong emotion such as laughter, anger, or surprise. Consciousness remains intact and it can also last for a few seconds to several minutes. There is no sensory component to cataplexy. Its presence distinguishes type one from type two narcolepsy. It is the last symptom typically to evolve in this disorder.
Disturbed nocturnal sleep is also present in 50% of patients with narcolepsy. While they usually have no trouble falling asleep, they often have restless sleep that is highly fragmented and often complain of insomnia. They also typically have early onset dreams. The average adult falls into their dreams after about 90 minutes of sleep onset. Narcoleptics can experience dreams within seconds to minutes of falling asleep. In addition, they experience an increased amount of REM throughout the night. The average adult has about 20-25% of dreaming during the night; a narcoleptic patient can have 30% or more dreaming.
Co-morbidities
Patients with narcolepsy also tend to have a higher incidence of other sleep disorders such as obstructive sleep apnea (estimates are as high as 50% of patients with narcolepsy have OSA), restless leg syndrome, periodic movements of sleep, and REM behavior disorder. Their increased cardiovascular risks are especially concerning. The incidence of myocardial infarction and cardiac arrest is 1.6 x higher than the average population. Hypertension is increased by 1.3 x, whereas heart failure is up by a whopping 2.6 x. Stroke is increased by 2.5 x. There are also increased rates of obesity, depression, and ADHD.
Pathyophysiology
The pathophysiology of patients with narcolepsy and cataplexy, type one, is low hypocretin-1 levels in the central nervous system. Hypocretin (also called Orexin) is the neurotransmitter that promotes wakefulness, helps maintain motor control and inhibits REM sleep. It stabilizes the sleep-wake state.
There is also a genetic predisposition to narcolepsy with cataplexy and occurs much more commonly in people with HLA – DQB1*0602. Genetics alone, however, are not sufficient for the development of narcolepsy. Often other environmental factors are also involved. There is an increase evidence of the role of winter associated infections, specifically an increase in antistreptolysin O (ASO) antibodies, a marker of infection with Streptococcus pyogenes. Interestingly, increased ASO was also found in narcolepsy patients who developed the disorder after vaccination against H1N1. This suggests an autoimmune component.
Diagnosis
Diagnosis is made based on the clinical scenario of excessive daytime sleepiness, sleep paralysis, hypnagogic/hypnopompic hallucinations, cataplexy, and disrupted nighttime sleep along with formal testing. First, ruling out other etiologies such as insufficient sleep syndrome, obstructive sleep apnea, hypothyroidism, depression, sedating medications, etc. should be done. If there no other reasons for these symptoms, then an overnight polysomnogram should be performed to observe sleep. The polysomnogram should be normal and the patient should sleep at least six hours. The following day, an MSLT (Multiple Sleep Latency Test) should also be performed. This is a daytime sleep study where the patient is given four or five 20-minute nap opportunities. If they fall asleep in 8 minutes or less, this is considered hypersomnolence. It is an abnormally short amount of time to fall asleep. If during their nap opportunities they display two or more sleep onset REM periods (SOREMP), this is positive for narcolepsy. A urine drug screen may be obtained to rule out the influence of substances that could affect sleepiness.
Treatment
Treatment involves good sleep hygiene with a regular wake and bed times, adequate sleep opportunity, scheduled naps (naps are restorative in patients with narcolepsy, at least for a short while) and medications. Medications will be chosen based on the patient’s severity and symptomatology. They could include alerting agents/stimulants, antidepressant medications such as selective serotonin uptake inhibitors (SSRIs) or serotonin and norepinephrine reuptake inhibitors (SRNIs) and sodium oxybate.
Prognosis
Narcolepsy is generally considered a chronic and irreversible lifelong disorder. Awareness, early detection and aggressive treatment can greatly improve quality of life at home and at work.
Whether it is excessive daytime sleepiness or one of the other comorbidities to sleep-disordered breathing, this article on a new screening tool can help you connect the dots. https://dentalsleeppractice.com/new-screening-tool-connects-cormobidities-sleep-disordered-breathing/
- Johns MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991; 14(6):540-5.
 Dr. Sahni has been in medical practice for 22 years. The first 11 years of her career she was an internist at Canyon Ranch Health resort. Since then, she has practiced sleep medicine exclusively. She opened her own practice, Swan Sleep Medicine, four years ago. When asked why she chose sleep medicine, she often jokes that she could not commit to a single organ. Fortunately, sleep medicine is a combination of pulmonology, cardiology, neurology, and psychiatry. Never boring, sleep medicine requires a multi-disciplinary approach to diagnosis and treatment. To that end, she has been certified in holistic medicine, nutrition, and Ayuvedic medicine as well as Sleep medicine. In general, sleep medicine is a happy field of medicine. When people are sleeping well, they feel more rested, of course, but also have better mood, sharper memories, lower heart risk, and stronger immunity. Dr. Sahni asks that you forgive the pun, but when sleep is improved, it’s like night and day! She evaluates patients in her office as well as administers home sleep tests to look for sleep apnea and insomnia studies to look at brain waves while sleeping. She treats a wide variety of adult sleep disorders. She is taking new patients.
Dr. Sahni has been in medical practice for 22 years. The first 11 years of her career she was an internist at Canyon Ranch Health resort. Since then, she has practiced sleep medicine exclusively. She opened her own practice, Swan Sleep Medicine, four years ago. When asked why she chose sleep medicine, she often jokes that she could not commit to a single organ. Fortunately, sleep medicine is a combination of pulmonology, cardiology, neurology, and psychiatry. Never boring, sleep medicine requires a multi-disciplinary approach to diagnosis and treatment. To that end, she has been certified in holistic medicine, nutrition, and Ayuvedic medicine as well as Sleep medicine. In general, sleep medicine is a happy field of medicine. When people are sleeping well, they feel more rested, of course, but also have better mood, sharper memories, lower heart risk, and stronger immunity. Dr. Sahni asks that you forgive the pun, but when sleep is improved, it’s like night and day! She evaluates patients in her office as well as administers home sleep tests to look for sleep apnea and insomnia studies to look at brain waves while sleeping. She treats a wide variety of adult sleep disorders. She is taking new patients.