by Kristie Gatto, MA, CCC-SLP, Certified Orofacial Myologist

Ideal health and function of the body is directly dependent upon optimal breathing patterns. Just as breathing impacts cellular regeneration; blood oxygenation; overall brain function; hormonal levels; and the strength and stamina of the muscular system, poor breathing patterns can also impact the development and function of orofacial complex. Orofacial myofunctional disorders can be found in both children and adults and often develop across the course of a lifespan. Orofacial myofunctional disorders (OMDs) are atypical patterns that emerge when normalized patterns are interrupted or impeded in some way. These maladaptive patterns often emerge during early growth and development, following a trauma or surgical procedure; and poor diet or not being able to breathe appropriately.
To date, Hanson (1982) still provides the most thorough definition of Orofacial Myofunctional Disorders:
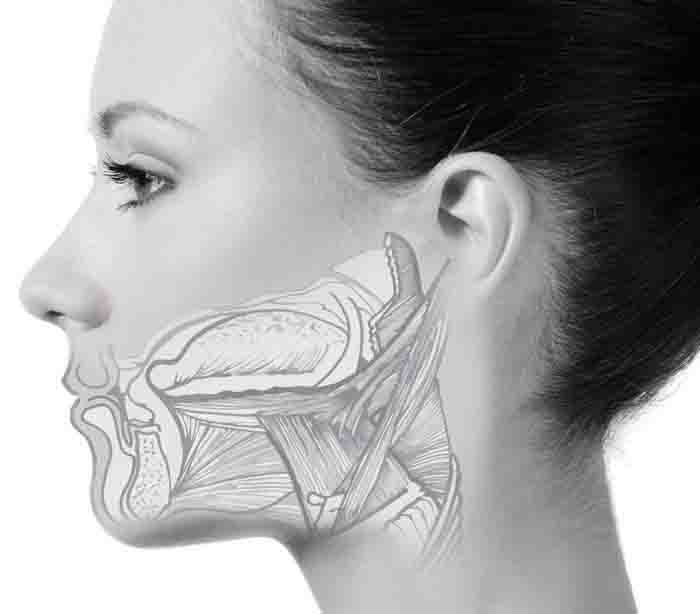
“Orofacial myofunctional disorder refers to abnormal resting labial-lingual posture of the orofacial musculature, atypical chewing and swallowing patterns, dental malocclusion, blocked nasal airways, and speech problems. These are patterns involving the orofacial musculature that interfere with normal growth, development, or function of the orofacial structures, or calls attention to itself.”
OMDs commonly seen in children, include an atypical swallowing pattern that requires dentalized tongue movement (anterior or interdental) and has historically been referred to as “tongue thrust.” OMDs encompass nonnutritive sucking behaviors such as thumb and/or digit sucking, cheek or tongue sucking, prolonged pacifier usage, clenching or bruxing, and so forth past 12 months in age. These patterns can lead to the development of other abnormal lip, tongue and jaw movement and posture patterns, affecting the eruption of dentition, and creating other changes to the oral cavity.
OMDs in the adult and geriatric populations occur secondary to various neurological impairments, oral hygiene problems, dental restorations, altered function of muscles due to aging, systemic diseases, or trauma to the oropharyngeal complex.
Orofacial myofunctional disorders are a cascade of dysfunction that emerges from a variety of etiologies.
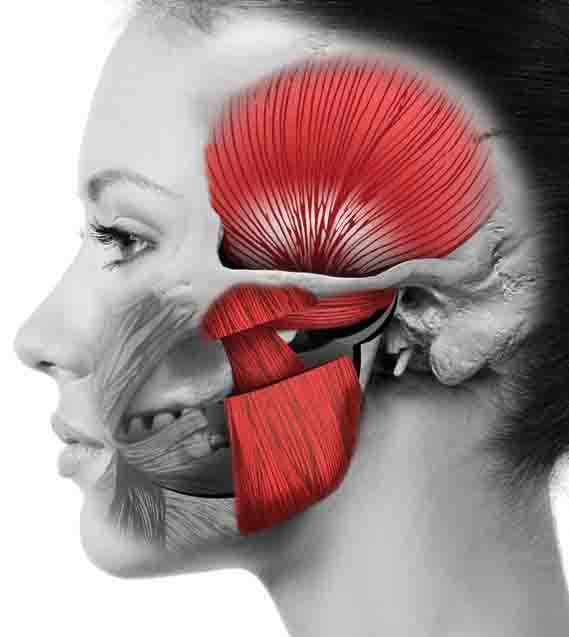
Oromyofunctional disorders are multifactorial in nature and are often the consequence of a sequence of events or lack of intervention at critical developing periods. This results in further oral dysfunction that can cause malocclusion, as well as changes in cranio and dentofacial development. The presence of systemic disordered breathing contributes to structural and functional symptoms of OMDs. For example, the impact of enlarged tonsils and/or adenoids and accompanying development of chronic upper airway obstruction. Growth and development can be negatively impacted by mouth breathing as a result of the hypertrophied tonsils and adenoids and their direct causal relationship with the anterio-posterior position of the maxilla. The reduced airflow through the nasal cavity forces the tongue downward in the mandible further impacting the vertical growth patterns when the lips part to breathe. The palate is then impacted when the absence of the tongue to palate fails to provide needed stability for maxilla development. This, in turn creates further soft tissues changes further altering muscle function. OMD’s are a cascade of dysfunction that emerges from a variety of etiologies.
Causes of OMDs include:
- Functional airway obstruction to include enlarged tonsils and adenoids, enlarged nasal turbinates, deviated septum, sinus infections, allergies (environmental or seasonal), chronic upper airway infections, asthma, sleep disordered breathing, including obstructive sleep apnea, and low oropharyngeal muscle tone resulting in airway collapse
- Oral resting postures, including mouth breathing
- Craniofacial disorder, craniofacial dysmorphology, malocclusion
- Sensorimotor dysfunction or disorder, functional limitations, low orofacial and oropharyngeal muscle tone
- Dysphagia
- Restricted oral frenula (early nursing difficulty with labial, lingual, and buccal movements for latching, sucking, lingual retraction, cupping, and elevation)
- Nonnutritive sucking & chewing habits – in utero or learned later that continue beyond the 12 months in age
- Chewing and eating behaviors, prolonged pureed feeds, or atypical soft food diets
- Idiosyncratic or aberrant movement behaviors
These changes require a multidisiciplinary approach including a certified orofacial myologist (COM™). An IAOM professional trained in orofacial myofunctional disorders specializes in the restoration of normalized function within the orofacial complex. Participation in their 48-year old Certification program is currently only open to professionals that have orofacial myofunctional disorders within the scope of practice for which they are currently licensed to practice. Those professionals include: dentists, dental hygienists, and speech-language pathologists. Proper assessment and intervention can vary from person to person and is dependent upon the underlying etiology or cause of the dysfunction. An effective treatment program consists: a comprehensive assessment, development of an individualized treatment plan, implementation of techniques to facilitate the dissociation of orofacial movements, followed by the coordinating the sequential orofacial movements for chewing, swallow and rest posture. A good program includes a period of follow-up checks to ensure that habituation outside the therapy setting.





