Peter Vitruk, PhD, writes about how a LightScalpel CO2 laser can result in minimal postoperative pain and discomfort after frenectomies and frenuloplasties.
by Peter Vitruk, PhD, MInstP, CPhys
First described in 2016, the LightScalpel Functional Releases include the following steps:1-4
- Pre-surgical Oro-Myofunctional Therapy (OMT);
- LightScalpel laser release, combined with the intra-operative Functional Assessment;
- Post-surgical OMT exercise program to ensure long-lasting Functional Results.
The goal of a Functional Frenectomy in children, adolescents and adults is to release the restricted frena, i.e. Tethered Oral Tissues (TOTs) and to restore, with the help of mandatory pre- and post-frenectomy Oro-Myofunctional Therapy (OMT), the mobility and functionality of tongue and lips for optimal breathing, speech, chewing, swallow, and posture. Besides the surgeon, a Functional Frenectomy involves a team trained in myofunctional (or physical, craniosacral, osteopathic, or chiropractic) therapies.1-4 Post-frenectomy, the surgical site is healed by second intention with mandatory OMT exercises. During Laser Frenuloplasty, sutures are placed after the laser release of restrictions.3 A properly performed Functional Frenuloplasty results in as high as “87% rate of improvement in quality of life through amelioration of mouth breathing (78.4%), snoring (72.9%), clenching (91.0%), and/or myofascial tension (77.5%).”5


Why LightScalpel CO2 laser?
Not all lasers are equally good at vaporizing, i.e., ablating or cutting and coagulating the blood vessels in the soft tissue, which is critical for fast and efficient frenectomies illustrated in Figures 1 and 2. Typically, tongue-tie revision with the CO2 laser does not involve suturing of the wound, and usually there is no scar. Minimal to no scarring is critical for post-operative OMT exercises that involve the tongue.
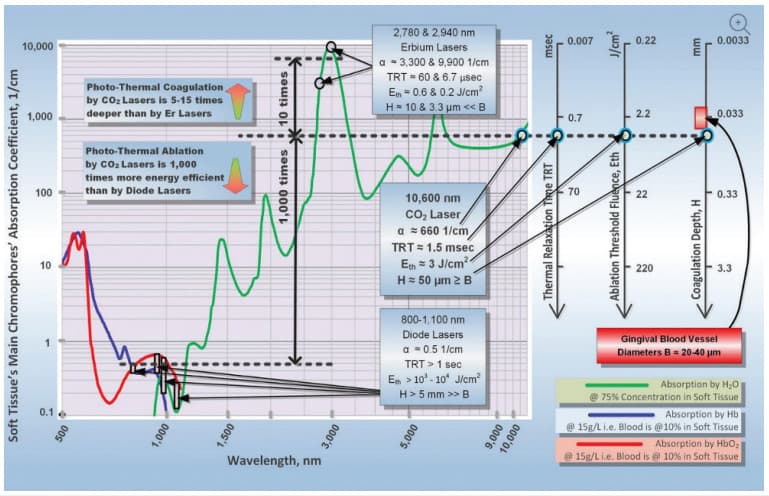
Figure 3 demonstrates the difference in the absorption spectra for the main soft tissue chromophores for different laser wavelengths and explains the following benefits of LightScalpel 10,600 nm CO2 lasers for oral soft tissue surgery:1-4
- Approximately 1,000 times greater photo-thermal cutting efficiency relative to dental diodes, and in approximately 10 times greater photo-thermal coagulation/hemostasis depth relative to erbium lasers;
- Close match between the coagulation depth of the CO2laser (approx. 50 µm for SuperPulse mode and 100-200 µm for non-SuperPulse) and the blood capillary diameters (20-40 µm).6 This distinguishes CO2 lasers from erbium lasers and provides for instant and efficient hemostasis and coagulation during high-speed ablation or cutting of the vascular tissues. The CO2 laser ablates tissue while coagulating small blood and lymphatic vasculature. It provides improved visibility of the surgical field and therefore enables more precise and accurate tissue removal;
- Minimal post-operative edema, pain and discomfort; due to the intraoperative closure of lymphatic vessels on the margins of the CO2laser incision. With CO2 laser frenectomy, patients report less post-operative pain and discomfort than with the scalpel.1-4
Depth of LightScalpel Laser Incision
During laser incisions, the power density of the focused laser beam is equivalent to the mechanical pressure that is applied to a cold steel blade. Greater laser fluence (i.e., power density times the duration it applied to the target) results in greater depth and rate of soft tissue removal. For short pulse steady state ablation conditions, the ablation depth is: A (E – Eth)/Eth, where A is the absorption depth and Eth is the ablation threshold fluence from Figure 3, and E is the fluence delivered to the tissue.1-4 For repetitive pulses that are scanned across the soft tissue, the depth of incision is proportional to laser average power, and is inversely proportional to focal spot diameter and the surgeon’s hand speed. For clinical cases illustrated in Figures 1 and 2, the LightScalpel CO2 laser was set to 2 W Non-SuperPulse, and gated at 20 Hz, 40-60% duty cycle, 0.8-1.2 W average power. A handpiece with a 0.25 mm focal spot diameter produces 300-400 µm depth shallow incisions at a 3-5 mm/sec hand speed. Such shallow incisions, combined with shallow coagulation depth (100-200 µm), allow for excellent and progressive visualization of larger diameter blood vessels.4
Summary
The choice for the CO2 laser wavelength and pulsing settings is based upon its unique absorption coefficient by the water-rich soft-tissue. Decreased wound contraction combined with minimal lateral tissue damage, less traumatic surgery, less post-operative pain, precise control over the depth of incision, and excellent hemostatic ability make the LightScalpel CO2 laser a safe and efficient tool for Functional Frenectomies and Frenuloplasties.1-4
Read more about LightScalpel and laser procedures in pediatric patients here: https://dentalsleeppractice.com/case-report/lightscalpel-10600-nm-co2-laser-procedures-in-pediatric-patients/
- Fabbie P, Kundel L, Vitruk P. Tongue-Tie Functional Release. Dent Sleep Practice. Winter 2016: 40-45.
- Riek C, Bahnerth S, Vitruk P. CO2 Laser Functional Frenectomy. Dent Sleep Practice. Spring 2019:34-36.
- Mugno M, Erson T. A Team Approach to Functional Laser Frenuloplasty and Optimal Orofacial Function. Dent Sleep Pratice. Fall 2019:48-52.
- Geis M, Kundel L, Vitruk P. Functional Frenectomy (Osteopathically Guided). Dent Sleep Practice. Summer 2018:30-32.
- Zaghi S, Valcu-Pinkerton S, Jabara M, Norouz-Knutsen L, Govardhan C; Moeller J, Sinkus V, Thorsen RS, Downing V, Camacho M, Yoon A, Hang WM, Hockel B, Guilleminault C, Liu SYC. Lingual frenuloplasty with myofunctional therapy: Exploring safety and efficacy in 348 cases. The Laryngoscope. 2019.
- Vitruk P, Levine R. Hemostasis and Coagulation with Ablative Soft-Tissue Dental Lasers and Hot-Tip Devices. Inside Dentistry. 2016 Aug;12(8):37-42.

 Peter Vitruk, PhD, is a founder of the American Laser Study Club and LightScalpel, Inc. in Bothell, WA, and a member of The Institute of Physics, London, UK. Dr. Vitruk can be reached at 1-866-589-2722 or
Peter Vitruk, PhD, is a founder of the American Laser Study Club and LightScalpel, Inc. in Bothell, WA, and a member of The Institute of Physics, London, UK. Dr. Vitruk can be reached at 1-866-589-2722 or