
I’m going to go out on a limb and assume that you do some type of a soft tissue evaluation and oral cancer screening in your office. I will also assume that either you or your hygienist routinely documents recession, probing depths and maybe even attachment levels. That’s a lot of soft tissue to look at, but it’s our responsibility and it’s in our patient’s best interest.
So, while you are there……looking at soft tissue……in the oral cavity……like you do every day……as a dentist……and documenting the findings……and discussing them with the patient……like you do……with every patient……would you be open to looking at another part of the oral cavity? I mean, with intention?
But before you say yes, you should know that you have to document it just like the rest of the oral cavity. And you might have to talk to the patient about it. Still in?
There is a big space in the back of the mouth in which we are always working. I call it “the air hole.” Like any other hole that is meant to transport fluid or air, the bigger the hole, the greater the volume. So, a smaller hole will usually result in less volume. A big hole that decreases in diameter anywhere along the path will result in pressure changes and even a compensatory or reflexive response, sometimes good, sometimes not so good.
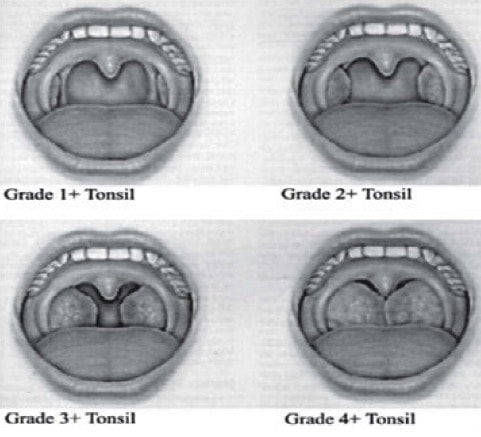
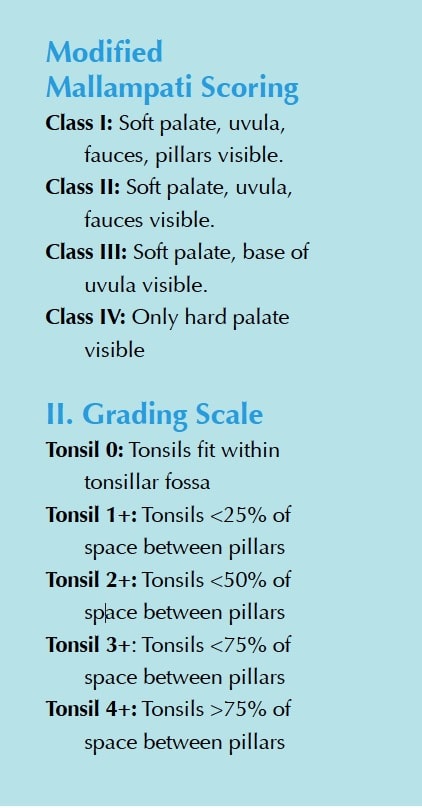
We can’t see too far down the air hole, but we can certainly see some structures getting in the way. Tonsils tend to fill up the air hole when they are inflamed or hypertrophied. We can at least note these, grading the right and left separately. One little note in your chart is sufficient.
Th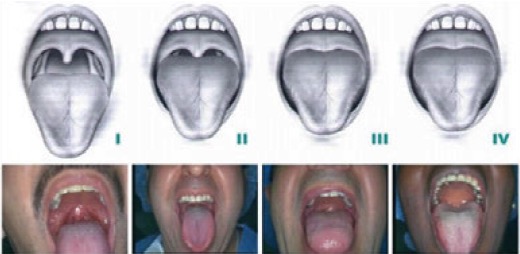 e soft palate and uvula can also hang down and cover the air hole. There is a well-accepted scoring system for this too, referred to as the Malampatti score, which is used in anesthesia to predict the ease of intubation.
e soft palate and uvula can also hang down and cover the air hole. There is a well-accepted scoring system for this too, referred to as the Malampatti score, which is used in anesthesia to predict the ease of intubation.
Although I have included the parameters for each scoring system below, if all we did was use the photos above and document the findings, we would be one step closer to helping our patents make healthy decisions.
 Remember the other disclaimer? You might then need to have a conversation about your findings with the patient. That’s ok. A simple discussion about an obstruction at the top of a pretty important air hole in their body is a great start. In future articles, I will discuss the implications that the obstruction can have, including snoring, upper airway resistance syndrome, apnea, chronic inflammation, acid reflux, and bruxism.
Remember the other disclaimer? You might then need to have a conversation about your findings with the patient. That’s ok. A simple discussion about an obstruction at the top of a pretty important air hole in their body is a great start. In future articles, I will discuss the implications that the obstruction can have, including snoring, upper airway resistance syndrome, apnea, chronic inflammation, acid reflux, and bruxism.
As you know, implementation is always difficult, even with the small changes. So, let’s keep it simple for now and acknowledge that we are the right people to be looking and that we have the opportunity to look there on a regular basis more than any other healthcare profession. Take a look, document, and start a discussion. We would want that for our friends and family, wouldn’t we?