Len Liptak and Dr. Mark T. Murphy discuss precision intraoral devices and how ProSomnus EVO is engineered with cutting edge AI and robotic technology.
 by Len Liptak, ProSomnus Co-founder and CEO, and Mark T. Murphy, DDS, D.ABDSM
by Len Liptak, ProSomnus Co-founder and CEO, and Mark T. Murphy, DDS, D.ABDSM
Picture yourself on the cover of this journal, being praised by your peers for crossing the chasm with sleep physicians. It is likely you did not do it alone. You had the help of modern medical device manufacturing, artificial intelligent design with efficacy and adherence that was finally on par with CPAP. You used advanced medical grade class VI materials and had evidence-based logic that guided AADSM AASM treatment protocols.
Inconsistent efficacy is the cardinal reason physicians are reluctant to refer patients for Oral Appliance Therapy (“OAT”). Studies, surveys, and focus groups have been conducted on this topic, ad nauseum. The feedback is clear: convince physicians that DSM providers have resolved the problem of inconsistent efficacy and physicians will refer patients for OAT. In other words, if you can provide OAT that delivers consistent efficacy you will be the DSM provider of the year. You even might find yourself on the cover of DSP.
How does one resolve inconsistent efficacy? Where is that data going to come from? All oral appliances are the same, right?
In DSM, before the advent of precision medical device designs for OSA therapy, research studies indicated that all traditional oral appliances had similarly inconsistent efficacy. All oral appliances do share the same mechanism of action: 1. protrude and 2. stabilize the mandible at a target position where the airway is patent. This mechanism of action is well-established in medical guidelines. It is evidence based, constructed upon systemic literature reviews.
Yet, what DSM providers might not be aware of is that traditional oral appliances are inconsistent at performing this mechanism of action.
“The recent peer reviewed independent research on ProSomnus EVO demonstrates efficacy on par with CPAP. Because of superior objective adherence, ProSomnus EVO is likely to be more effective than CPAP. This is what physicians have been waiting for, better treatment options for OSA than CPAP or HNS. The results of the FLOSAT and Severe OSA trials, currently underway, will be transformative for sure. The new ProSomnus sensor technology will give physicians the final link to engage with us. Incredible stuff.” – John E. Remmers, MD
Traditional oral appliances do not consistently protrude the mandible at the target position. We measured this before founding ProSomnus. Protrusive positions deviated from target by an average of three millimeters. A more recent study reported an average protrusion variance of 3.7 +/- 1.4 millimeters relative to target. For those familiar with dental laboratory methods for fabricating oral appliances, this inconsistency is understandable. Building a complex, patient-specific, oral appliance by hand is very difficult, even if CAD/CAM assisted.
Nor do traditional oral appliances consistently stabilize the mandible at the target position. On average, traditional oral appliances allow the mandible to retrude approximately two millimeters for every five millimeters of mouth opening. Herbst arms and angled dorsal posts allow the mandible to retrude if a patient opens their mouth during sleep. Nylon and elastomeric strap titration mechanisms allow several millimeters of anterior-posterior play, in addition to stretching and deforming over time.
Might inconsistent efficacy be the consequence of traditional oral appliances’ inability to consistently protrude and stabilize the mandible at the target position? Do five or six millimeters of error affect efficacy? Consider that the mean minimum upper airway cross section for an OSA patient is 4.6 +/- 1.2mm (Ogawa, 2006). The magnitude of the inconsistency of traditional oral appliances exceeds the mean minimum upper airway cross section!
Not surprising, scientific investigations by Esaki in 1997, Kato in 2000, Walker in 2003, Gindre in 2008, and Aarab in 2010 report a “dose dependent” relationship between efficacy and mandibular protrusion. After standardizing definitions, these studies suggest a one-millimeter change in mandibular protrusion is associated with a 10% change in efficacy. It seems logical that a five- or six-millimeter variance in mandibular protrusion might affect efficacy.
To clarify, this is not to suggest more consistent protrusion and stabilization transforms non-responders into responders. Non-responders are non-responders. What this is suggesting is that there are responders who end up as non-responders because the oral appliance does not reposition and stabilize their mandible within an acceptable tolerance of the target position. When this happens, a patient who would respond, might not respond, despite the best efforts for the DSM provider to titrate and adjust the appliance. This inconsistency drags down the mean efficacy for the population treated with traditional oral appliances.

Why not adjust the traditional oral appliance to maximum protrusion? The same dose dependency research finds that the risk of side effects increases with protrusion. Each millimeter of incremental protrusion is, in general, associated with an incremental increase in side effect risk. It is important to find the target and select a device that can protrude and stabilize the mandible at that target position.
Yes, in the hands of select providers, or by following preferred protocols, or appliance titration, one could sometimes eke out a few more points of efficacy with traditional oral appliances. With inconsistent efficacy somewhat assumed, choosing an oral appliance was far more about patient preferences, dental considerations, comfort, management of side effects, ease of delivery and use. The initial price of the device along with the full cost of repair, remake and chair time were also fair game in the provider decision matrix. Most of the above choices might help improve patient adherence, create practice efficiencies, and save the provider money to round out the business case in DSM. This is all good. But none of it adequately addresses the root cause issues of inconsistent efficacy.
What if a new type of precision intraoral medical device could more consistently protrude and stabilize the mandible relative to target? What if a new type of precision intraoral medical device could virtually eliminate the five or six millimeters of inconsistency relative to the target mandibular position? Might eliminating these inconsistencies in mandibular protrusion yield more consistent efficacy? Might this also reduce the risk of side effects, with the assumption that providers would be less likely to over-protrude while chasing efficacy?
Precision intraoral medical devices are a new category of OAT devices. Precision intraoral medical devices, such as the EVO® by ProSomnus®, are engineered to consistently protrude and stabilize the mandible within one millimeter of the target mandibular position for each patient. ProSomnus precision devices, for example, have a quality control specification of 0.5mm of global variance. The term global refers to six axis total variance, including anterior posterior, vertical, lateral, roll, pitch, and yaw variances. The actual mean global variance for ProSomnus devices is 0.32mm, about 12x less global protrusion variance than the typical traditional oral appliance.

Precision intraoral medical devices such as EVO by ProSomnus stabilize the mandible in the target position. The ProSomnus EVO, for example, features a 90-degree post. This 90-degree post allows the mandible to move side to side and even vertically while still stabilizing the mandible in the target protrusive position.
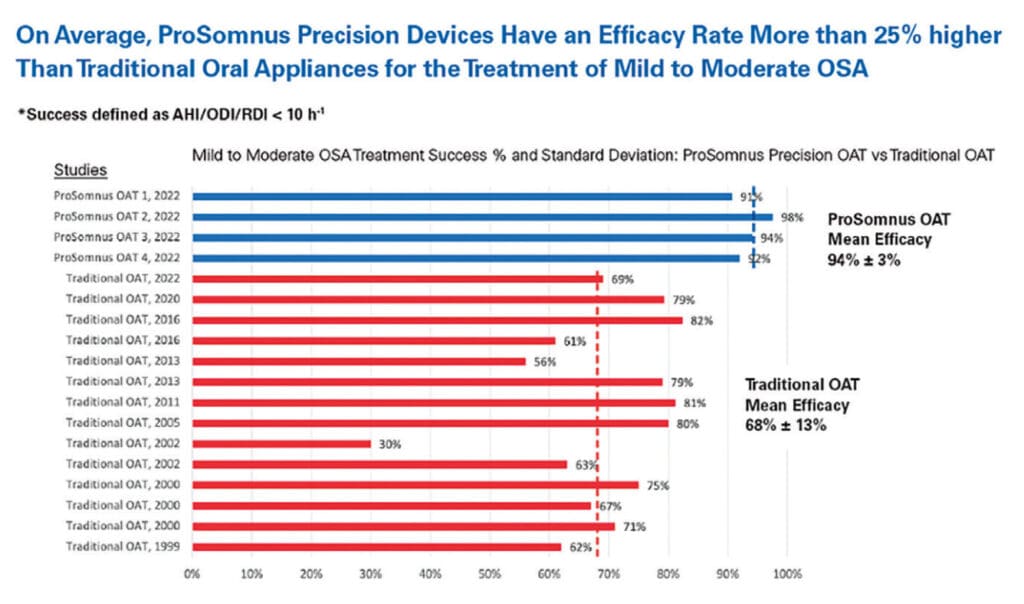
Utilizing AI-driven software and manufacturing robots to virtually eliminate protrusion inconsistencies, precision intraoral devices by ProSomnus that have demonstrated 94% success treating mild and moderate OSA patients to an AHI/ODI below 10 events per hour. This is approximately 26% points better than what has been previously reported for traditional oral appliances. These types of efficacy results suggest the overall effectiveness (efficacy times adherence) of precision intraoral devices may be on par with CPAP for mild and moderate OSA patients.
“I switched to ProSomnus precision devices based on patient experience and clinical outcomes. I published a retrospective analysis of 115 consecutively treated patients at the World Sleep Congress in Rome, March of 2022. The data showed that a precision oral appliance is capable of successfully treating patients with all levels of severity with most patients treated to an AHI < 5 and 29 severe patients with an average AHI of 51.5 were treated to a final AHI average of 9.9.” – Edward T. Sall, MD, DDS, MBA
Outcomes data consistently demonstrating greater than 90% efficacy with precision intraoral devices, although more data is warranted and those studies are in-process, may convince physicians to reconsider Oral Appliance Therapy as part of their overall prescription mix. It is estimated that there are over six million CPAP placements annually in North America. The prescription OAT market may represent as high as 5% or 300,000 devices. That estimated ratio has remained unchanged over the years and the CAGR for PAP and OAT have grown in parallel. A simple 10% shift in prescribing patterns will triple the demand for OAT. Traditional oral appliances will not drive this change; they haven’t for decades. Precision, intraoral devices that provide medical grade outcomes data, delivered by caring qualified therapy providers striving for improved efficacy, better adherence, and improved health outcomes likely will be what it takes.
The environment is ripe to educate physicians about the merits of precision Oral Appliance Therapy relative to traditional oral appliances. Physicians and their patients have very quickly learned that not all CPAPs are the same. Like oral appliances, for years physicians assumed that all CPAPs were the same. Like oral appliances, all CPAPs share the same mechanism of action. The mechanism of action for a CPAP is to overcome airway obstruction by applying an appropriate amount of pressure. Not enough pressure and the airway might still collapse. Too much pressure and the patient may be less likely to tolerate it.
Yet all CPAPs are irrefutably not the same. One specific brand of CPAP is under FDA recall. Why not recall all CPAPs, if they are all the same? The brand under recall uses different materials than the other brands. And those materials are associated with a higher risk to patient safety. Same mechanism of action as the other CPAP brands? Yes. Same performance profile as the other CPAP brands? No.
Moving forward, ProSomnus will continue to pursue efficacy. If we want to boost treatment effectiveness, there is no other option. Multiple studies have reported objectively recorded adherence rates of over 90% with ProSomnus precision intraoral devices. There really isn’t much opportunity to get better in the realm of adherence.
ProSomnus will also continue to invest in research that evaluates the role of precision intraoral devices on efficacy criteria beyond AHI. For example, ProSomnus devices are associated with some of the only papers published in medical journals that use Oxygen Desaturation Index endpoints. ProSomnus devices are being utilized for investigations evaluating the impact of OAT on sleep apnea specific hypoxic burden and sleep apnea specific delta heart rate.
Wrapping up, consistent efficacy was the key barrier to OAT earning more prescriptions from physicians. Today, precision intraoral medical devices are engineered to optimize efficacy by virtually eliminating the mandibular protrusion and stabilization errors inherent with traditional oral appliances. Precision intraoral medical devices, specifically ProSomnus devices, have demonstrated excellent efficacy for patients with mild and moderate OSA, and severe OSA too. The levels of efficacy associated with precision intraoral devices, combined with objective reported adherence, place precision oral appliances at least on par with CPAP when it comes to treatment effectiveness (efficacy times adherence). DSM providers who have evolved their appliance selection criteria to precision intraoral medical devices are seeing significantly more prescriptions from sleep physicians, better efficacy and improved outcomes. Precision intraoral medical devices are the bridge that crossed the chasm.
 Len Liptak is the CEO of ProSomnus® Sleep Technologies. An award-winning executive with expertise growing and operating innovation-oriented businesses, Len is a founding member of ProSomnus, and co-inventor of the company’s flagship product. Len also serves on the company’s Board of Directors. Prior to starting ProSomnus, Len was President of MicroDental Laboratories, where he led the commercialization of multiple, award-winning new products, guided business unit operations, and directed the expansion of the company’s digital supply chain. During Len’s tenure, the company grew three times faster than the industry average, expanded gross margins, and set company records for profitability. Len was named to ExecRank’s list of top executives for privately held companies in 2012 and 2013. In 2016, Len led the sale of MicroDental Laboratories to the Modern Dental Group (HKG:3600). Len also spent 10 years at 3M Company and Stryker Corporation in strategic business development, business unit management, and product development capacities. Len earned an M.B.A. from the University of Minnesota’s Carlson School of Management and a B.A. from Brown University. A lifelong learner, Len has completed executive education programs at John’s Hopkins, and is a member of the Young President’s Organization (YPO).
Len Liptak is the CEO of ProSomnus® Sleep Technologies. An award-winning executive with expertise growing and operating innovation-oriented businesses, Len is a founding member of ProSomnus, and co-inventor of the company’s flagship product. Len also serves on the company’s Board of Directors. Prior to starting ProSomnus, Len was President of MicroDental Laboratories, where he led the commercialization of multiple, award-winning new products, guided business unit operations, and directed the expansion of the company’s digital supply chain. During Len’s tenure, the company grew three times faster than the industry average, expanded gross margins, and set company records for profitability. Len was named to ExecRank’s list of top executives for privately held companies in 2012 and 2013. In 2016, Len led the sale of MicroDental Laboratories to the Modern Dental Group (HKG:3600). Len also spent 10 years at 3M Company and Stryker Corporation in strategic business development, business unit management, and product development capacities. Len earned an M.B.A. from the University of Minnesota’s Carlson School of Management and a B.A. from Brown University. A lifelong learner, Len has completed executive education programs at John’s Hopkins, and is a member of the Young President’s Organization (YPO). Mark T. Murphy, DDS, D.ABDSM, is an American Board of Dental Sleep Medicine Diplomate and has practiced in the Rochester, MI area for 40 years. He is the Chief Growth Officer at ProSomnus Sleep Technologies, serves on the DSM faculty at University of Detroit Mercy School of Dentistry, and is a regular presenter on Dental Sleep Medicine at the Pankey Institute. He has served on the Board of Directors of the Pankey Institute, National Association of Dental Laboratories, the Identalloy Council, the Foundation for Dental Laboratory Technology, St. Vincent DePaul’s Dental Center, and the Dental Advisor. He lectures internationally on Leadership, Strategic Planning, and Dental Sleep Medicine.
Mark T. Murphy, DDS, D.ABDSM, is an American Board of Dental Sleep Medicine Diplomate and has practiced in the Rochester, MI area for 40 years. He is the Chief Growth Officer at ProSomnus Sleep Technologies, serves on the DSM faculty at University of Detroit Mercy School of Dentistry, and is a regular presenter on Dental Sleep Medicine at the Pankey Institute. He has served on the Board of Directors of the Pankey Institute, National Association of Dental Laboratories, the Identalloy Council, the Foundation for Dental Laboratory Technology, St. Vincent DePaul’s Dental Center, and the Dental Advisor. He lectures internationally on Leadership, Strategic Planning, and Dental Sleep Medicine.