by Dr. Gy Yatros
The clinical aspects of Dental Sleep Medicine (DSM) are relatively simple. There, I said it. From a clinical standpoint, DSM is much simpler than placing an implant, prepping a crown, or mounting casts for a full mouth rehab. If DSM is one of the most rewarding services that a dentist can bring into their practice then why aren’t more offices offering these services? And, why do many motivated offices eventually fail to realize their DSM vision?
Is it because of commitment issues, clinical challenges, software, team education, testing issues, medical insurance billing, TMD management, or a myriad of other challenges? After consulting with thousands of dentists around the United States, I can tell you, the answer is simply ‘YES’ to all of the above.
In Dental Sleep Solutions’ collective 20+ years immersed in DSM, Dr. Richard Drake and I have discovered that to successfully practice DSM, only two things are mandatory; commitment of the dentist and the dental team and implementation of successful systems. Too often, we see dentists that attend a weekend program and return to the office on Monday only to encounter resistance and a lack of team buy-in. This is the death knell for the fledgling DSM practice. Everyone must be on board. For those practices that achieve their DSM success the time and effort is always well worth the investment. Without this commitment to education and systems implementation involving screening, testing, communication, treatment, and follow-up, practices will fail. You know what motivates your team. Appeal to those sensibilities and get everyone revved up to move forward.
Once commitments have been made and a unified mission established, the next hurdle is implementation of simple, proven, repeatable systems. Each individual piece of this mosaic may be a minor hurdle but when viewed in aggregate, it often becomes an overwhelmingly complex puzzle. Simplifying the pieces into repeatable systems results in a checklist to success that can make nearly anyone successful.
The challenges are the same for nearly everyone. How do you:
- Identify these patients?
- Screen them?
- Get them tested without them falling into the
- “black hole of CPAP?”
- Set appropriate fees?
- Present the case to increase patient acceptance?
- Decide which device to use?
- Mitigate side effects?
- Decide on how and when to advance the device?
- Do follow up (titration) testing?
- Receive medical insurance reimbursement for
- your time and expertise?
- Document treatment?
- Communicate with referring physicians?
Once the challenges are understood a simple repeatable system for each hurdle should be defined. The entire team should be aware of these systems and what happens at each juncture. Falling short on just one hurdle can stop a DSM practice dead in its tracks. Imagine that you have your team educated, you begin to understand the links between OSA and medical comorbidities, you implement a seamless screening process and you now have patients who are ready to be tested! The patient eagerly approaches your front desk expecting your team to be ready to help coordinate the sleep test but instead there is confusion and the patient leaves without direction. This type of issue can occur at any step of the patient flow if systems aren’t clearly defined and followed by the entire team. The bottom line is that providing sleep medicine in the dental office will flounder unless all the aspects are covered.
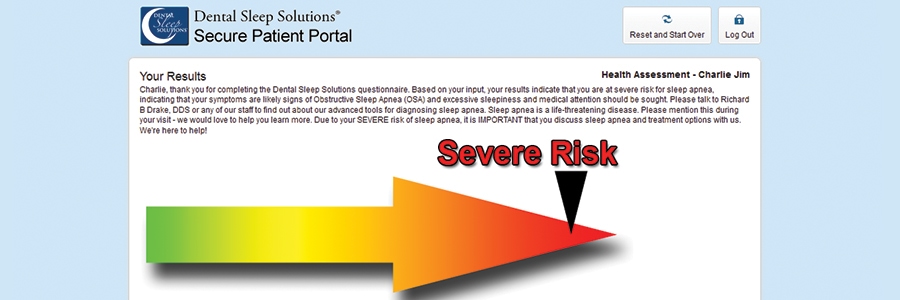
In subsequent issues, we’ll highlight DS3, an extremely effective implementation system that seamlessly provides solutions to all of the aforementioned hurdles, empowering you and your team to make dynamic strides towards realization of your DSM vision. From team education and pragmatic checklists to simple tools for every step from screening to testing to device selection and claims submission, DS3 is the most comprehensive Dental Sleep Solution available via the cloud or anywhere else. Stay tuned for the next issue when I’ll describe screening and testing protocols through the DS3 system.