Dr. Keith Thornton explains how dentists can help patients to effectively treat and manage their SRBD at home with the myTAP appliance.
by Keith Thornton, DDS
The COVID-19 pandemic has created a paradigm shift in the medical acceptance and patient expectation of telemedicine as a treatment pathway. The treatment of Sleep Related Breathing Disorders (SRBD) is no exception.
There are three aspects of the treatment of SRBD to be taken into consideration:
- Options and opportunities for telemedicine
- Use of an immediate appliance for diagnosis, treatment, and long-term management
- Future potential for dentists and physicians
 Options and Opportunities
Options and Opportunities
As we turn our attention toward telemedicine and SRBD, workflows must be developed for both diagnosed and non-diagnosed patients, and immediate appliances can play an integral role. These new workflows provide opportunities for dentists, sleep physicians, and other practitioners to address and support patients’ needs right now. With guidance, patients are able to fit some of these appliances remotely. Not all immediate appliances are created equally, and it’s recommended that clinicians provide patients with appliances that are proven most effective compared to other non-custom appliances that are available.
Why myTAP?
The myTAP is the culmination of more than 25 years of incremental improvements and developments. It is unique in that it not only positions the mandible protrusively but also vertically and encourages nasal breathing utilizing the proprietary mouth shield.
All oral devices have two characteristics in common: They all have a tray system for attaching to the teeth, and all have some kind of mechanism for positioning the mandible
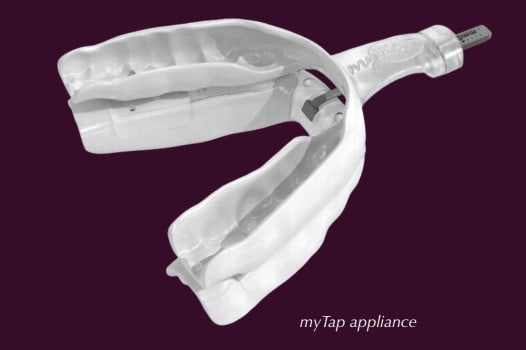 The myTAP is not made on casts. Instead, it is directly fit to a patient’s teeth without any interim steps that can lead to errors with fit and retention. The Flexible Precision™ unique property of the material allows the trays to fit the teeth precisely with the proper resiliency necessary to maintain appropriate retention with a passive fit. The trays themselves are thinner and take up less space in the oral cavity than any other non-custom device. Additionally, it can be refit an unlimited amount of times to create the correct amount of retention for that patient which is critical for a patient fitting themselves at home.
The myTAP is not made on casts. Instead, it is directly fit to a patient’s teeth without any interim steps that can lead to errors with fit and retention. The Flexible Precision™ unique property of the material allows the trays to fit the teeth precisely with the proper resiliency necessary to maintain appropriate retention with a passive fit. The trays themselves are thinner and take up less space in the oral cavity than any other non-custom device. Additionally, it can be refit an unlimited amount of times to create the correct amount of retention for that patient which is critical for a patient fitting themselves at home.
The myTAP is a modified version of the original TAP. The TAP has over 40 peer reviewed, independent studies and is both the most efficacious and effective device on the market. In the 2015 AASM guidelines, the TAP was the only appliance that was successful in treating all levels of apnea to below 10 AHI.1
- In three studies by Hoekema, the average AHI before treatment was 3 while the average afterward was 6 – an 85% reduction. All six studies on the TAP met the AASM oral appliance success criteria (greater than 50% reduction, less than 10 AHI.)
- In six studies, dorsal-style devices failed to reduce the AHI to below 10 even though the average starting AHI was only moderate.
- Herbst had three studies with only mild to moderate patients. One failed to achieve the 10 AHI criteria while the other two only reduced the AHI by 60%.
- An Army study (N=497) using TAP, had patients with an average pre-treatment of 30 (severe) while post-treatment it was 8.3, virtually the same as CPAP.
The newest feature improvements to the myTAP are vertical adjustments and a mouth shield to encourage nasal breathing.
The myTAP has 3 vertical shims available to give a 6mm, 9mm, and 12mm vertical opening. In the studies by both Hoekema and the Army, the “size of the box” of the oral cavity correlated to successful outcomes. Further studies have shown that the size of the tongue is dependent on weight, and it affects the severity of OSA. To compensate for tongue size, a larger vertical opening is necessary. Preliminary data from ACTA (Amsterdam) shows significant outcome improvements utilizing the 6mm for women (9mm for obese) and 9mm for men (12mm for obese).
The mouth shield encourages physiologic (nasal) breathing as most healthy sleepers tend to nasal breathe during sleep. The Guilleminault study found that airway resistance, and the risk for OSA, is significantly lower when breathing nasally. Physiologic breathing, which maintains proper CO2 levels, controls respiratory drive, reduces sympathetic tone, humidifies, heats, and filters the air. It also provides an uptake in nitric oxide.
Future Implications
The future is already here – NOW! The opportunity to develop a standard of care for evaluation and treatment of SRBD via telemedicine exists today. The value for the physician and dentist is the added perceived, and real, value in the “chronic disease management” of these patients through yearly follow-up to assess efficacy and coach the patient. In-office visits can be minimized to device replacement or repair.
In many situations, patients can effectively treat and manage their SRBD at home with a device such as the myTAP; it is the interface with their Dental Sleep Medicine professional for diagnosis, treatment, guidance, and follow-up that will be key in achieving superior outcomes. Clinicians are encouraged to develop a comprehensive approach, utilizing both CPAP and oral appliances, for SRBD evaluation and treatment.
MyTAP has changed the way dentists can treat and manage patients. Read Dr. Thornton’s interview about the development of adjustable mandibular positioning devices and the treatment of sleep apnea by dentists. https://dentalsleeppractice.com/clinician-spotlight/driven-help-world-sleep/
- Ramar, Kannan, et al. “Clinical Practice Guideline for the Treatment of Obstructive Sleep Apnea and Snoring with Oral Appliance Therapy: An Update for 2015.” Journal of Clinical Sleep Medicine, 11, no. 07, 2015, pp. 773–827., doi:10.5664/jcsm.4858.
 Keith Thornton, DDS, is a third generation dentist who practiced restorative dentistry for 40 years in Dallas. His practice is limited to the treatment of airway and breathing disorders. He is a member of nine different dental and medical organizations and has had numerous leadership positions. He has been a member of the American Academy of Dental Sleep Medicine since 1993 and was an original Diplomate of the American Board of Dental Sleep Medicine. He is a visiting faculty member at A&M College of Dentistry, and is a consultant to the Army, Navy, Air Force and the VA. He has developed a number of medical devices that treat snoring and obstructive sleep apnea and has 72 issued patents. He is the founder, owner, CEO and chief technical officer for Airway Technologies, Inc.
Keith Thornton, DDS, is a third generation dentist who practiced restorative dentistry for 40 years in Dallas. His practice is limited to the treatment of airway and breathing disorders. He is a member of nine different dental and medical organizations and has had numerous leadership positions. He has been a member of the American Academy of Dental Sleep Medicine since 1993 and was an original Diplomate of the American Board of Dental Sleep Medicine. He is a visiting faculty member at A&M College of Dentistry, and is a consultant to the Army, Navy, Air Force and the VA. He has developed a number of medical devices that treat snoring and obstructive sleep apnea and has 72 issued patents. He is the founder, owner, CEO and chief technical officer for Airway Technologies, Inc.