CE Expiration Date: August 10, 2026
CEU (Continuing Education Unit):2 Credit(s)
AGD Code: 180
Educational Aims
This self-instructional course for dentists aims to help the reader understand more about the connection and the value of having an orofacial myofunctional therapist on the treatment team for most patients of nearly all ages. Oral-systemic connections are becoming common knowledge in Dentistry. The links are rapidly expanding beyond nutrition, medications, and microbiome to include movement and body work, including physical therapy and orofacial myology. There is a long history of therapy that is only now gaining widespread recognition as a key element in whole-body wellness, including oral health.
Expected Outcomes
Dental Sleep Practice subscribers can answer the CE questions online at https://dentalsleeppractice.com/continuing-education/ to earn 2 hours of CE from reading the article. Correctly answering the questions will demonstrate the reader can:
- Define the role orofacial myofunctional therapy (OMT) can play in their practice and lead their team to present this to patients.
- Discuss how OMT can be helpful at many age levels of patients for specific indications.
- Back up clinical observations with research supporting potential therapies.
In this CE by Nicole Goldfarb, M.A., CCC-SLP, COM®, she describes how having an Orofacial Myofunctional Therapist can be helpful for patients with certain conditions and also help to backup clinical observations.
 by Nicole Goldfarb, M.A., CCC-SLP, COM®
by Nicole Goldfarb, M.A., CCC-SLP, COM®
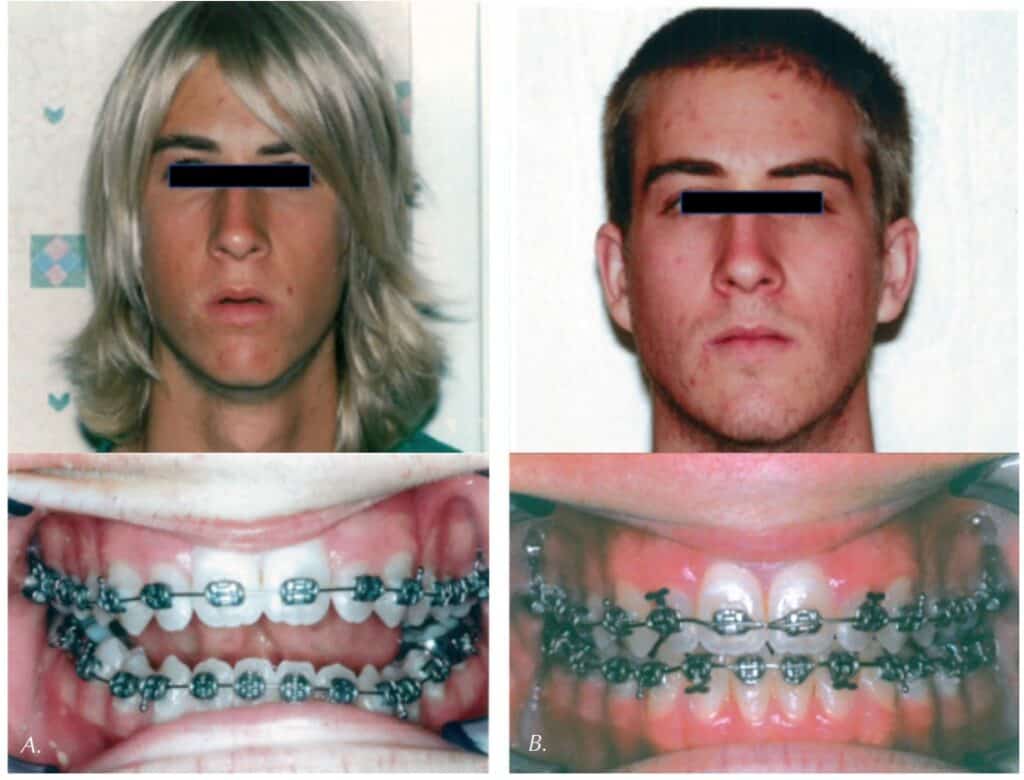
As knowledge about the etiology of sleep-disordered breathing (SDB) has expanded over the recent years, it is imperative to recognize that a team approach to intervention is paramount to the success of any treatment plan. In accordance with this multidisciplinary approach, an orofacial myofunctional therapist may be a key player on your dental team. Working directly with an orofacial myofunctional therapist may be one of the most effective ways to comprehensively treat your dental sleep patients. This article will explore the relationship between orofacial myology and dentistry and how these specialties can work together to better benefit patients of nearly any age. The team of the dental specialist and the orofacial myofunctional therapist can play a joint role in not only resolving malocclusion, but more importantly identifying red flags for soft tissue dysfunction, airway issues, and SDB.
It is now recognized that dental specialists have a responsibility to screen their patients of any age for sleep-related breathing disorders and to assist in treating or referring out for treatment for this condition. In addition, it is important to emphasize that over the past century, empirical and clinical data has shown that orofacial myofunctional therapy (OMT) goes beyond the benefits to the dental structures and into other disciplines like sleep medicine as well. Therefore, this crucial collaboration between the dental specialist and the orofacial myofunctional therapist cannot be overstated. Let’s look at what OMT is and how an orofacial myofunctional therapist can help your patients.
What is Orofacial Myofunctional Therapy?
OMT is a treatment program to resolve oral muscular dysfunction in order to establish correct oral rest posture and functioning of the oral facial system. OMT identifies and treats dysfunction of the oral facial muscles across the 5 domains of:
- Oral rest posture
- Chewing and swallowing of food
- Swallowing of liquids
- Sucking and swallowing of saliva
- Speech (if the therapist is a Speech-Language Pathologist (SLP))
OMT can further be defined as “therapeutic exercise-based techniques, based on the principles of motor learning and neuroplasticity, to stabilize, tone, strengthen, or improve the range of motion of the skeletal muscles of the face and neck used to treat a range of orofacial myofunctional disorders.”1 Research and clinical evidence proves that OMT plays a crucial role in the identification and treatment of a variety of oral dysfunctions, and remediation of such soft tissue dysfunction can help prevent or assist in the treatment of the related sequelae of issues including dental malocclusion, oral health problems, feeding issues, speech disorders, postural issues, upper airway problems, sleep-disordered breathing, and the health and quality of life impacts of such problems.

History of Orofacial Myofunctional Therapy
Orofacial myofunctional therapy is not a new profession, to say the least, emerging in the early 1900s as a response from the orthodontic field to restore normal muscle function to remove unintentional pressure on the dental structures. OMT was initially developed by orthodontists as a means of improving orthodontic outcomes and preventing orthodontic relapse. As early as the late 1800s, Edward Angle, DDS, first recognized that mouth breathing and poor resting posture of the tongue can play a primary role in hindering orthodontic outcomes. In the early 1900s, Alfred Rogers, DDS, further advanced the field by acknowledging the role of soft tissue dysfunction on the oral skeletal system, and he developed exercises for the orofacial musculature.2 Rogers was an orthodontist born in 1873, and he was the President of the American Association of Orthodontists (AAO), the American Academy of Dental Sciences, and was also instrumental in forming the American Board of Orthodontics. Rogers was one of the first to develop a treatment program targeting orofacial muscular exercises which was indicated to stimulate desirable growth in the maxillofacial region, and he called this therapy “Myofunctional Therapy in Orthodontics.”3 As early as 1918, Rogers wrote articles and presented papers on this concept, including presenting at the annual meeting of the AAO in which he relayed the effects of the orofacial musculature and highlighted the foundation of OMT as a means of improving orthodontic outcomes, orthodontic stability, achieving facial balance and better growth and development of the oral structures. Rogers stressed that orthodontists must not focus solely on straightening teeth, but rather must attend to the role of the function of the oral facial muscles as having an impact on the skeletal system. Rogers asserted that alterations in functional activity of the oral cavity can cause malocclusion. The work of Alfred Rogers, DDS, over 100 years ago lay the foundation for OMT and the concept that muscular functioning has an impact on oral facial growth, development, and overall whole-body health. As the field of OMT advanced, over 50 years ago in 1972 the International Association of Orofacial Myology (IAOM) was developed, which is the first international organization to train and certify SLPs and dental hygienists in OMT.4
Orofacial myofunctional therapy is a specialty area on top of an individual’s already established licensure as an SLP, dental hygienist, physical therapist, or occupational therapist. Although some individuals choose to focus their clinic work solely within OMT, this practice cannot be separated or isolated from their primary licensure which regulates their practice of OMT. You can therefore view OMT as a “modality” of treatment.
The importance of OMT cannot be overstated in the comprehensive treatment of orthodontic patients as well as playing a key role in the in the prevention of serious developmental problems within the orofacial respiratory complex. We begin with what defines correct oral rest posture before truly grasping the significance of OMT for the dental specialist.
What is Correct Oral Rest Posture?
Correct oral rest posture entails the following components: the lips closed/sealed at rest, the entire tongue gently suctioned to the palate (front, middle, and back of the tongue, with the sides of the tongue resting within the dental arch), and the teeth slightly apart with appropriate dental freeway space. This correct vertical alignment of the arches combined with a lips-closed posture will help maintain correct tongue posture. When the lips open or even slightly part, the tongue will likely lose suction from the palate and will drop within the oral cavity. Moreover, the tongue has enough weight to drop the mandible and cause the lips to open. This bidirectional relationship of lip and tongue posture cannot be overemphasized. This correct posture produces better relaxation of the facial and perioral muscles and promotes nose breathing, which is proven to be the healthiest way for humans to breathe. In addition, correct oral rest posture will assist in better dental and facial development, as the tongue and lips are natural growth supports for proper arch development.

What is an Orofacial Myofunctional Disorder (OMD)?
Given that we know what correct rest posture of the oral facial structural complex entails, we must seek to understand why a deviation in such patterning may exist. An OMD encompasses any of the following, often in combination:
- Any deviation in correct oral rest posture of the lips, tongue, and/or jaw
- A thrusting of the tongue during chewing and swallowing or speech
- Noxious or parafunctional oral habits such as digit sucking, tongue sucking, cheek biting, nail biting, lip licking, prolonged pacifier use, or bruxism, to name a few
An orofacial myofunctional therapist identifies and evaluates the causes of OMDs to determine the best treatment plan of such habits and soft tissue dysfunction. A key understanding in the myofunctional therapy evaluation process is not complete unless it identifies all the factors that are capable of causing or contributing to the OMD, which may include problems in the medical system, dental system, or the myofunctional system. Orofacial myofunctional therapists refer patients to ENT doctors, allergy doctors, and airway focused dentists or orthodontists to assist in the comprehensive treatment plan to resolve such dysfunction and the sequelae of effects that such soft tissue problems can trigger. There are many cases where the medical cause of the dysfunction must be resolved before the muscles are rehabilitated in OMT, and this may include certain cases of adenoid or tonsillar hypertrophy or other pathology impacting nasal patency. The OMT acts as a team player in initiating such referrals and in gauging when myofunctional therapy can be initiated. Timing of myofunctional therapy is also influenced by whether a malocclusion is too significant and needs to be addressed prior to the OMT. In some cases, OMT should be initiated before or during orthodontic treatment, whereas in other cases therapy is best to wait until after appliances are removed. Communication between the orofacial myofunctional therapist, ENT doctor, dentist, and orthodontist is crucial to outcome success.
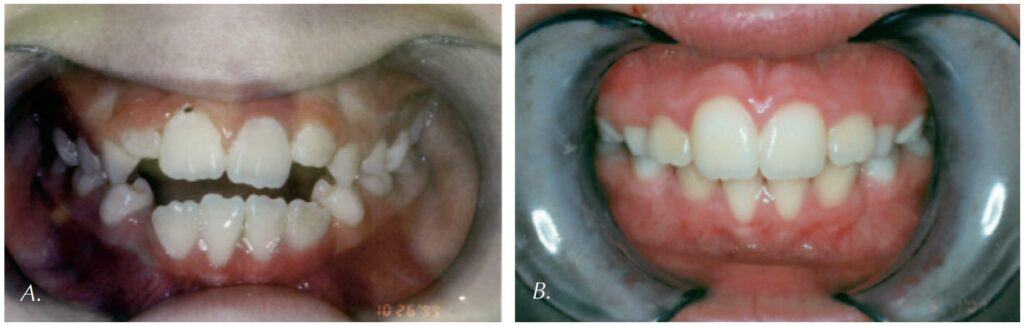
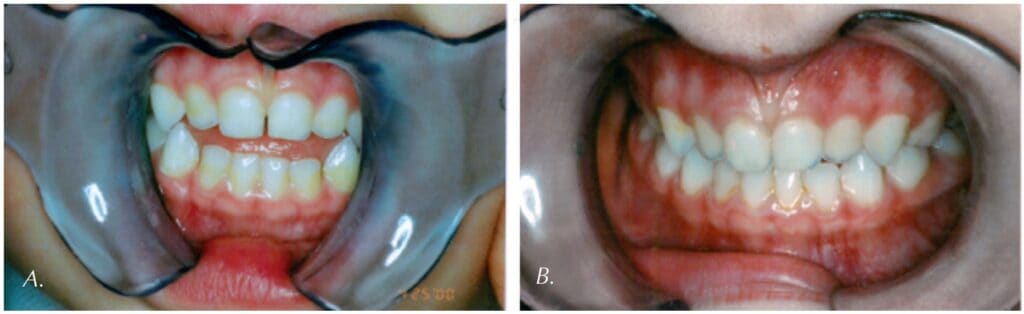
What are the Impacts of OMDs?
This foundational understanding of OMDs and what defines normal resting posture of the orofacial structural complex leads to a discussion of the negative health and developmental impacts when an OMD is present. Not only does soft tissue dysfunction contribute to dental malocclusion, but it is also important to understand the multitude of changes in the orofacial respiratory complex and entire body system that can occur when malocclusion is present. If there are alterations in the airway which interfere with normal nasal breathing, then facial growth and function may proceed along a different path, with the potential to change the skeletal growth not only of the entire face, but also head/neck posture, whole-body posture, breathing patterns, and sleep quality. Physical therapists have referred to the tongue as “the rudder to the spine” and understand that correct tongue posture helps with whole-body posture via connections of the tongue to the oral pharyngeal airway, down the hyoid bone, through the deep frontal fascial plane. When jaw growth is not ideal, the nasal and pharyngeal airway can become negatively impacted. When the airway is impacted, the head and neck can compensate in a “forward head posture” to help open the airway to facilitate better breathing. Moreover, any reduction in the airway size from the tip of the nose down the throat including factors such as nasal obstruction, narrow palate, retruded jaws, open mouth posture, low tongue posture, or any hypotonia of the orofacial complex can affect the quality of sleep in individuals of any age, from infancy through adults, leading to SDB and the end stage disease of obstructive sleep apnea (OSA). OMDs should be recognized early and must not be ignored once red flags are identified, which can often easily be recognized in the dental or orthodontic office.

Research on OMT
Research shows that OMT is effective in helping to prevent orthodontic relapse, facilitating correct growth of the orofacial complex, assisting with correction of orthodontic problems during orthodontic treatment, and has a significant role in not only helping to treat but also helping to prevent SDB and OSA. Studies show that OMT:
- Significantly improves the outcome SDB post adenotonsillectomy
- Combined with rapid palatal expansion (RPE) leads to better treatment outcomes among patients with SDB than with RPE alone
- Can be the necessary factor in preventing the relapse of SDB in patients who have undergone RPE and lingual frenectomy
- May actually prevent much SDB in the young population
- Can decrease the severity of OSA, promotes improved oxygen saturation during sleep, and can improve sleep quality and life quality
- Improves CPAP compliance
- Can be an adjunct to hypoglossal nerve stimulation treatment for OSA
- Can assist in preventing orthodontic relapse in most orthodontic cases
- Can improve oral health in patients, including decreasing the risk of periodontal disease
Early Intervention
It is not surprising that the earlier an OMD is identified, the chances of a further sequelae of related issues is mitigated. Myofunctional disorders are progressive and if left untreated they will typically worsen over time. Therefore, early identification of such soft tissue dysfunction is paramount in the treatment process. Typically, it is an SLP with specialized training in feeding therapy and oral sensory motor therapy that has the skills and expertise to treat children younger than the age of 4. Often there are foundational feeding and oral motor skills that need to be addressed in the early intervention (infancy through 3-year-old age group) before a standard OMT program would ever be considered. After age 4, most children then have the cognitive ability to imitate, self-monitor, understand the goals, and therefore participate in an OMT program. In many cases even 4+ year old children need regular feeding and oral sensory motor therapy by an SLP in addition to OMT. It is never too early to seek an OMT assessment by a trained professional, whether it be a specially trained SLP for the birth through 3-year-old age range or an SLP or dental hygienist specially trained OMT for patients aged 4-years-old and above. Often multiple therapists including IBCLC, PT, OT are on the team for such patients who have multiple whole-body issues. Signs of dysfunction are often there before symptoms are present, and it is best to refer out for an assessment as early as issues are noticed.
It is Never Too Early, and It is Never Too Late
Just as “it is never too early to learn normal oral function,”5 it is never too late to remediate problems in the oral muscular system. Currently, the youngest patient in our office with oral sensory/feeding dysfunction is 12-months-old, and our oldest patient with oral muscular dysfunction contributing to his OSA is 84-years-old. It is also important to understand that many cases of untreated OMDs may have begun in childhood and developed into end stage sleep apnea in adulthood as the oral muscular system, facial structure, and airway never properly developed due to these initial muscular problems. Although early treatment and prevention is of utmost importance, there is always an opportunity to help a person suffering from an OMD, as this can truly impact the quality of that person’s life.
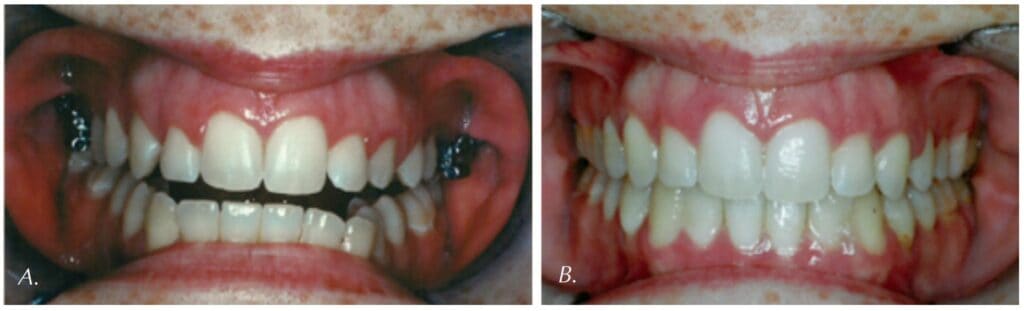
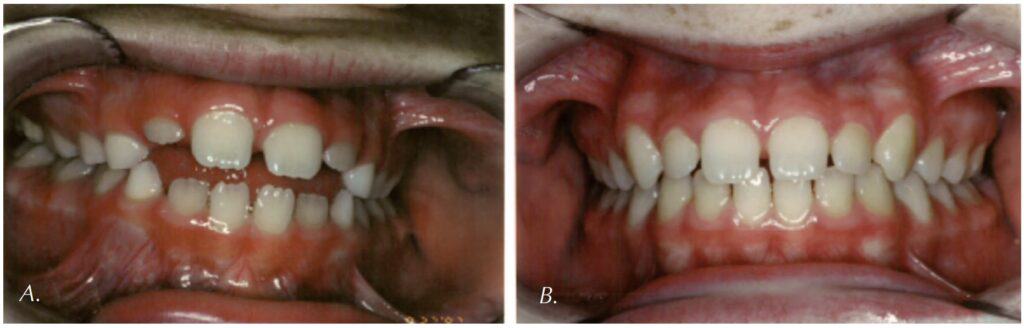
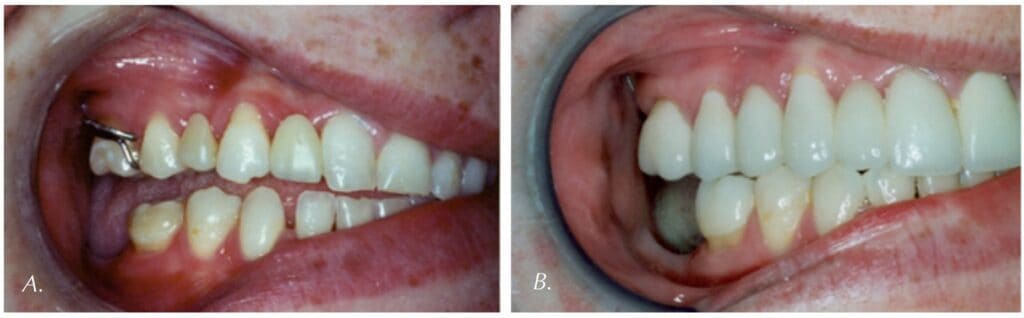
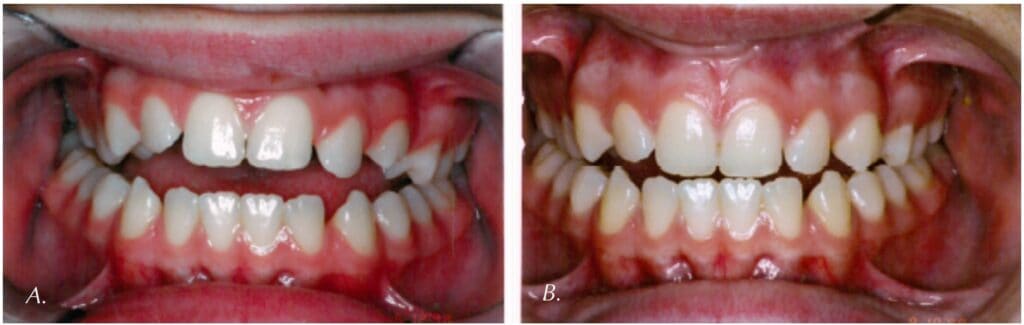
Correct oral rest posture assists in facial development, supporting natural arch development.
 How an Orofacial Myofunctional Therapist Can Help You
How an Orofacial Myofunctional Therapist Can Help You
Given this detailed description of OMT, it is obvious that dentists and orthodontists should team up with orofacial myofunctional therapists in the assessment and treatment of their patients. According to the ADA Policy Statement in 10/2017, all dentists should screen patients for sleep-related breathing disorders, and an OMD is a clinical marker to look for.6,7 It is important for dental specialists to be able to identify markers for OMDs which include red flags such as narrow palates, crowded teeth, malocclusion, dental wear or tori from bruxism, scalloped tongue, open mouth breathing, low tongue posture, tongue thrust, tongue tie, mentalis strain / lip incompetence, large tonsils, noxious oral habits, and even speech issues such as a lisp can be easily identified by the dental specialist and can trigger a referral to the orofacial myofunctional therapist in the team approach. Once we know something, we must not ignore it, and I am hopeful that this knowledge of our intermixed disciplines will help to bridge the connection between dental specialists and orofacial myofunctional therapists to better help our patients achieve the best care and quality of life possible.
After reading this CE, find out more about the benefits of adding an Orofacial Myofuctional Therapist by reading this article by Kristie Gatto: https://dentalsleeppractice.com/myofunctional-therapy/.
References
- D’Onofrio L. (2019, November 22). Publication trends and levels of evidence in orofacial myofunctional therapy literature. [Presentation]. ASHA 2019: Orlando, FL, United States.
- Rogers, A. P. (1939). Evolution, development, and application of myofunctional therapy in orthodontics. American Journal of Orthodontics and Oral Surgery, 25(1), 1-19.
- Rogers, A. P. (1918). Exercises for the Development of the Muscles of the Face, with a View to Increasing Their Functional Activity. The Dental Cosmos, LX(59), 857-924.
- Mills CS. International Association of Orofacial Myology History: origin – background – contributors. Int J Orofacial Myology. 2011 Nov;37:5-25. PMID: 22774699.
- Direct quote from D’Onofrio L, “It is never too early to learn normal oral function.”
- D’Onofrio L. Oral dysfunction as a cause of malocclusion. Orthod Craniofac Res. 2019;22:43-48.
- ADA Policy Statement: The Role of Dentistry in the Treatment of Sleep Related Breathing Disorders. Adopt ed 2017
 Nicole Goldfarb, M.A., CCC-SLP, COM, founded the San Diego Center For Speech & Myofunctional Therapy 20 years ago, and shas been practicing Speech-Language Pathology since 2003 and Orofacial Myofunctional Therapy since 2008. Nicole holds the distinction of being one of only a few Certified Orofacial Myologists® in all of San Diego County that also has a master’s degree in Speech-Language Pathology, an unparalleled combination of degrees which allows her to provide the most advanced and comprehensive treatment, as most patients with speech issues also have myofunctional issues. Nicole worked as a Speech-Language Pathologist in a school district for 7 years, servicing thousands of children with speech and orofacial disorders. She has a special passion and interest in sleep-disordered breathing (SDB) and diagnosing restricted frenums as they relate to myofunctional disorders. Nicole has presented internationally on myofunctional therapy as it relates to SDB in both children and adults. She is currently on the Child Airway Initiative Task Force (CAST), a national team of doctors, dentists, and orthodontists developing a universal screening tool for all dentists to use to screen patients for SDB as per the 10/2017 American Dental Association proposal that all dentists should screen all patients for SDB. Nicole is the host and developer of the audio and video podcast for Airway Circle Radio titled “Airway Answers: Expanding Your Breath of Knowledge”. Nicole is also a Breathe Institute Ambassador, a Talk Tools® Education Partner, author of the myofunctional therapy chapter in an upcoming medical textbook, and she is currently on the faculty for ASAP (Airway, Sleep, and Pediatrics Pathway) and the Sleep Education Consortium. Nicole’s life-long quest is to help in the early identification and treatment of SDB.
Nicole Goldfarb, M.A., CCC-SLP, COM, founded the San Diego Center For Speech & Myofunctional Therapy 20 years ago, and shas been practicing Speech-Language Pathology since 2003 and Orofacial Myofunctional Therapy since 2008. Nicole holds the distinction of being one of only a few Certified Orofacial Myologists® in all of San Diego County that also has a master’s degree in Speech-Language Pathology, an unparalleled combination of degrees which allows her to provide the most advanced and comprehensive treatment, as most patients with speech issues also have myofunctional issues. Nicole worked as a Speech-Language Pathologist in a school district for 7 years, servicing thousands of children with speech and orofacial disorders. She has a special passion and interest in sleep-disordered breathing (SDB) and diagnosing restricted frenums as they relate to myofunctional disorders. Nicole has presented internationally on myofunctional therapy as it relates to SDB in both children and adults. She is currently on the Child Airway Initiative Task Force (CAST), a national team of doctors, dentists, and orthodontists developing a universal screening tool for all dentists to use to screen patients for SDB as per the 10/2017 American Dental Association proposal that all dentists should screen all patients for SDB. Nicole is the host and developer of the audio and video podcast for Airway Circle Radio titled “Airway Answers: Expanding Your Breath of Knowledge”. Nicole is also a Breathe Institute Ambassador, a Talk Tools® Education Partner, author of the myofunctional therapy chapter in an upcoming medical textbook, and she is currently on the faculty for ASAP (Airway, Sleep, and Pediatrics Pathway) and the Sleep Education Consortium. Nicole’s life-long quest is to help in the early identification and treatment of SDB.


