CE Expiration Date: November 1, 2026
CEU (Continuing Education Unit):2 Credit(s)
AGD Code: 730
Educational Aims
This self-instructional course for dentists aims to help the reader understand more about physical therapy. Dentists who provide airway therapy in their practice have expanded their focus beyond the oral cavity into adjacent structures, e.g., the nose and oropharynx. Dentists who have considered temporomandibular disorders part of their service mix have embraced some orthopedic principles. Linking these physiologic characteristics is physical therapy. Far more than just a rehabilitation service, PT can add significant value to a treatment regimen, increasing the stability of positive results. This article will help the dental team learn more about what PT can add and provide some simple screening tools to identify which patient may benefit from a thorough physical therapy evaluation.
Expected Outcomes
Dental Sleep Practice subscribers can answer the CE questions online at https://dentalsleeppractice.com/continuing-education/ to earn 2 hours of CE from reading the article. Correctly answering the questions will demonstrate the reader can:
- Recognize contributions of poor body function to clinical signs and symptoms
- Develop office workflows for screening patients in this area
- Open a conversation with physical therapists in their area to identify collaboration partners
An airway-centric approach to physical therapy can help patients with complex issues related to dental sleep medicine and TMD by correcting faulty postural and movement patterns.
 by Brad Gilden, PT, DPT, FFMT, FAAOMPT, PRC, CSCS, and Bill Esser, MS, PT, CCTT
by Brad Gilden, PT, DPT, FFMT, FAAOMPT, PRC, CSCS, and Bill Esser, MS, PT, CCTT
Role of an AirwayCentric® Physical Therapist in Dental Sleep Medicine
Physical Therapists are trained to recognize and treat faulty postural and movement patterns involving the human musculoskeletal and neuromuscular systems. When repetitive inefficiencies in skeletal alignment or aberrant movement patterns occur, compensations take over compromising the health of the system. The stomatognathic and respiratory systems are among the first regions of the body to be affected by these compensatory activities. Starting with the nasopharyngeal area extending down to the diaphragm. The primary driver of inhalation is the thoracic diaphragm. If the ribcage is not properly aligned over the pelvis, the diaphragm will remain in a hypertonic contracted state, leading to a cervical accessory muscle driven breathing pattern. When the neck becomes more involved in breathing, increased tension is developed in the craniofacial, orofacial, craniomandibular, cervical and thoracic regions that can lead to upper airway resistance. Increased nasopharyngeal resistance will manifest developing further compensations which may include: parafunction, nasal congestion, mouth breathing, excessive tongue activity, increased pressure on the cardiovascular system and alteration of the body’s pressure systems. Symptoms that arise from these compensations may include headaches, tinnitus, dry mouth and throat, vestibular/balance deficits, scoliosis, TMJD, neck pain, GERD, ankyloglossia and the development of malocclusion. The role of an AirwayCentric Physical Therapist (ACPT) is to correct inefficiencies in postural and movement patterns to prevent or reverse the resulting compensatory tendencies. Reinstating efficient posture and body mechanics will not only help the reduction or elimination of painful symptoms, it will also support any dental work to prevent relapse.
For the purpose of this text, ACPT is used to define a physical therapist that has specialized postgraduate education focused on the evaluation and treatment of patients with disorders related to the nasal and oral airway, such as obstructive sleep apnea (OSA). ACPT’s use a multi-disciplinary approach to provide medical and therapeutic interventions that aim to alleviate airway obstruction and improve patient’s quality of life. ACPT’s work in close collaboration with other healthcare professionals, including dentists, otolaryngologists, myofunctional therapists and pulmonologists, to ensure the patient receives the best possible care. You will not find a specific degree associated with this designation. There will be guidance at the end of this chapter on how to locate an ACPT in your area.
When a patient presents to a medical professional with suspected nasopharyngeal abnormalities, there are both intrinsic and extrinsic factors contributing to the problem. Intrinsic factors may include anatomical anomalies that increase resistance to airflow such as a narrow maxilla, swollen tonsils/adenoids, retruded mandible, malocclusion or ankyloglossia. Extrinsic factors that can increase airway resistance may include forward head posturing, parafunctional habits such as nail biting, poor workstation or sleeping positions, an inflammatory diet and poor stress management skills. Having a multi-disciplinary approach to first recognize and make appropriate referrals to a trusted colleague can be the difference between success and failure. Building a team that includes an Airway Centric Physical Therapist to help identify and treat intrinsic and extrinsic factors is paramount.
Temporomandibular Joint Dysfunction (TMD)
In 1934, JB Costen, an otolaryngologist, published an article implicating occlusion as the primary cause of TMD. Ten years later a second article further solidified the framework for occlusion being the cause of TMDs. For the next 75 years, the field of dentistry embraced TMD as its own in an attempt to treat TMD by altering the patient’s occlusal schema. Taking on the mantle of responsibility for TMDs dentists are currently considered the primary providers for, authority on, and are considered legally responsible for, the evaluation and treatment of the TMD patient (H. Clifton Simmons III, DDS, Journal of Craniomandibular Practice & Sleep Practice. 2016, Vol 34, No.2). With the exception of a few physical therapists (Mariano Racabado, Steve Kraus, Harry VonPiekartz) the medical field appears grateful to have placed the burden of care and treatment of this complex diagnosis upon their dental colleagues’ shoulders. Over the past 25 years, a mounting body of research has questioned and is reaching the conclusion that occlusion does not stand alone as the initiator, sustainer, and perpetuator of TMDs. Jeffrey Okeson DMD presents at his annual University of Kentucky TMD, Orofacial Pain and Dental Sleep Medicine Residency in 2019 that a systematic review, looking at 349 studies from 1966-2002 (with only 4 relevant studies fulfilling the inclusion criteria) concluded “There were very few associations reported between malocclusions, functional occlusion, and TMD. Research shows that almost every type of occlusal relationship and maxillomandibular relationship can be found in equal proportions among patients with TMD and non – symptomatic patients (1. Pullinger AG.Selgman DA. Quantification and validation of predictive values of occlusal variables in temporomandibular disorders using multifactorial analysis. 2. Michelotti A, Iodine G. The role of orthodontics in temporomandibular disorders. J. Oral Rehab. 2010:37, 411-429). A recent article in AJO-DO (American Journal of Orthodontia and Dentofacial Orthopedics 2022 Jun;161 (6):769-774) “What have we learned from 1992 – 2022”, states orthodontists should avoid diagnosing and treating TMDs within the traditional mechanical and dental-orthodontic based frameworks and that TMD’s complexity may be best approached from a biopsychosocial standpoint. It is becoming clearer that the complexity of what initiates, sustains, and perpetuates TMDs is multidimensional requiring the expertise of both dentistry and medicine. To effectively address the TMD patient, dental and medical professionals need an interdisciplinary understanding of the anatomy and function of the teeth, occlusion, head, neck, and trunk as they relate to TMD. The TMD practitioner must understand the interrelation of these multiple components and how dysfunction of any single or multiple elements of this system can initiate and sustain TMD. Unilaterally treating TMD patients from a dental or medical therapy approach has led to the current confusion and often failed treatment the TMD patient experiences.
When to Refer a Patient to an AirwayCentric Physical Therapist?
The first step adding physical therapy to your patient’s plan of care is to properly identify when a referral for physical therapy is appropriate. Many of your patients may already be working with a rehabilitation professional – (Physical Therapist, Chiropractor, Occupational Therapist, Osteopath). It is a good policy to ask if they enjoy working with this professional and understand their approach to the airway. This could be an opportunity to add a qualified professional to your team whom your patient already values and trusts.
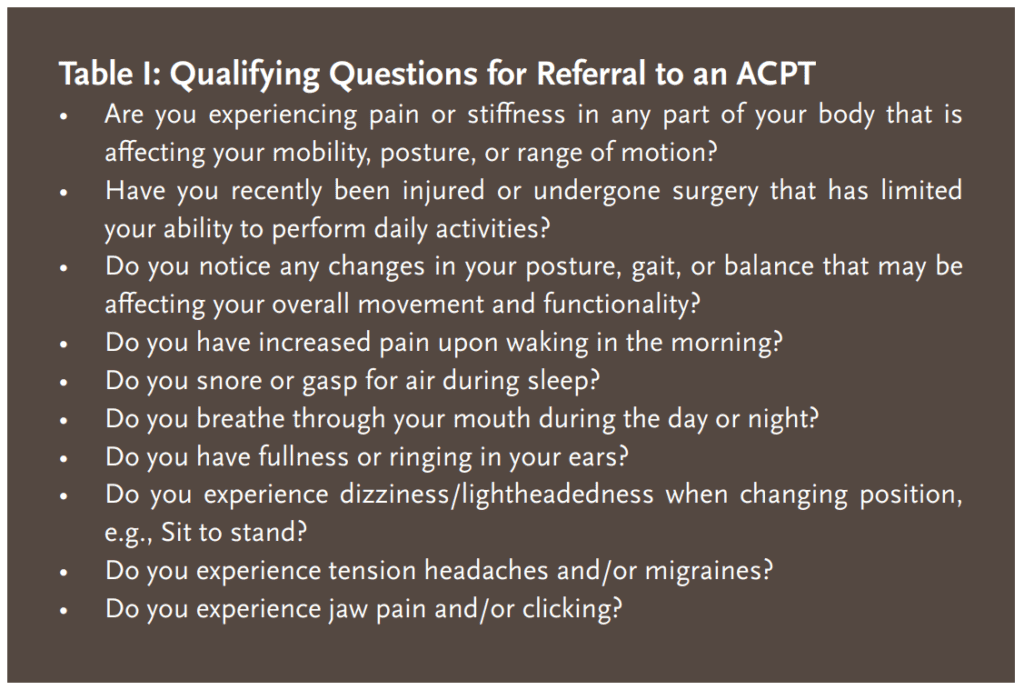
There are specific parameters to determine the appropriateness for a referral to an ACPT. Below is a list of qualifying questions that would lead you to consider making a referral.
Physical Therapy Airway Screen
The following represents a quick screen a dentist can use to determine if a patient is a good candidate for an ACPT referral. You should expect asymmetrical craniofacial patterns in every patient during this screen. However, when there is a large clustering of asymmetries, combined with subjective complaints of pain or loss of stomatognathic function, a referral to an ACPT should be considered.

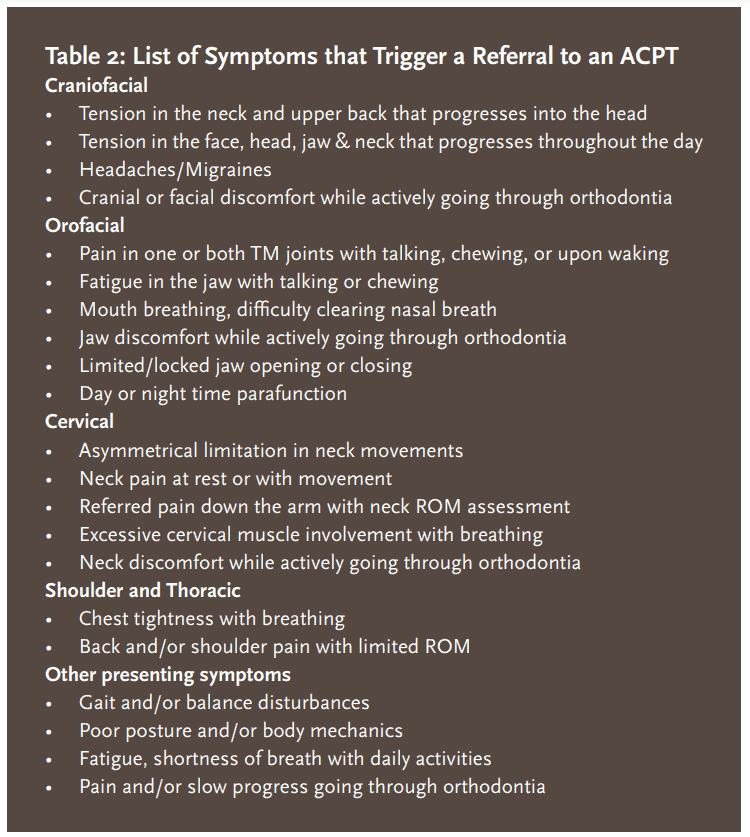 In conclusion, collaboration between physical therapists and dental professionals is crucial in addressing the complex issues related to dental sleep medicine and TMD. Physical therapists, specifically AirwayCentric Physical Therapists (ACPTs), possess the knowledge and expertise to identify and treat musculoskeletal and neuromuscular dysfunctions that contribute to airway obstruction and TMD. By correcting faulty postural and movement patterns, ACPTs can alleviate pain, improve mobility, and support dental treatments to prevent relapse. It is essential for dental professionals to recognize the symptoms that warrant a referral to an ACPT, such as pain, stiffness, changes in posture or balance, snoring, mouth breathing, and jaw issues. By incorporating physical therapy into the patient’s care plan, dental professionals can provide comprehensive and interdisciplinary treatment, leading to improved patient outcomes and quality of life. I encourage dental professionals to seek collaboration with qualified ACPTs in their area to enhance the care they provide and ensure the best possible outcomes for their patients. Together, we can optimize the management of dental sleep medicine and TMD, addressing the multidimensional nature of these conditions and improving patient well-being.
In conclusion, collaboration between physical therapists and dental professionals is crucial in addressing the complex issues related to dental sleep medicine and TMD. Physical therapists, specifically AirwayCentric Physical Therapists (ACPTs), possess the knowledge and expertise to identify and treat musculoskeletal and neuromuscular dysfunctions that contribute to airway obstruction and TMD. By correcting faulty postural and movement patterns, ACPTs can alleviate pain, improve mobility, and support dental treatments to prevent relapse. It is essential for dental professionals to recognize the symptoms that warrant a referral to an ACPT, such as pain, stiffness, changes in posture or balance, snoring, mouth breathing, and jaw issues. By incorporating physical therapy into the patient’s care plan, dental professionals can provide comprehensive and interdisciplinary treatment, leading to improved patient outcomes and quality of life. I encourage dental professionals to seek collaboration with qualified ACPTs in their area to enhance the care they provide and ensure the best possible outcomes for their patients. Together, we can optimize the management of dental sleep medicine and TMD, addressing the multidimensional nature of these conditions and improving patient well-being.
For more information, contact the author of this article at gildenpt@gmail.com.
Read more about physical therapy in the dental sleep practice in “Whole Body Alignment: Physical Therapy for TMD,” at https://dentalsleeppractice.com/whole-body-alignment-physical-therapy-for-tmd/
 Dr. Brad Gilden has been practicing physical therapy since graduating from New York Medical College in 2000. He has worked in a variety of settings treating patients with various neurological, orthopedic and postural related dysfunctions. In 2004, he completed a clinical doctorate in upper quarter and hand therapy from Drexel University. He joined Elite Health Services as a managing partner and rehabilitation coordinator in 2005 and co-founded IPA Manhattan Physical Therapy in 2011, and Kinetichain Integrative Manual Therapy in Aspen, Colorado in 2019. He is certified in both Functional Manual Therapy and Postural Restoration aimed at illuminating movement dysfunction and postural awareness while integrating patients back to their highest level of health. In 2010, he completed an intensive certification in functional manual therapy through the Institute of Physical Art. In 2014, he completed a three-year long fellowship in functional manual therapy through the IPA and American Academy of Orthopedic Manual Physical Therapy. In 2020, he completed certification through the Postural Restoration Institute. He is an active member of the American Physical Therapy Association, American Academy of Orthopaedic Manual Physical Therapy, and the American Academy of Physiological Medicine and Dentistry. He lectures internationally at various medical conferences and on the adverse effects of breathing pattern disorders and chronic sympathetic overload on the human body.
Dr. Brad Gilden has been practicing physical therapy since graduating from New York Medical College in 2000. He has worked in a variety of settings treating patients with various neurological, orthopedic and postural related dysfunctions. In 2004, he completed a clinical doctorate in upper quarter and hand therapy from Drexel University. He joined Elite Health Services as a managing partner and rehabilitation coordinator in 2005 and co-founded IPA Manhattan Physical Therapy in 2011, and Kinetichain Integrative Manual Therapy in Aspen, Colorado in 2019. He is certified in both Functional Manual Therapy and Postural Restoration aimed at illuminating movement dysfunction and postural awareness while integrating patients back to their highest level of health. In 2010, he completed an intensive certification in functional manual therapy through the Institute of Physical Art. In 2014, he completed a three-year long fellowship in functional manual therapy through the IPA and American Academy of Orthopedic Manual Physical Therapy. In 2020, he completed certification through the Postural Restoration Institute. He is an active member of the American Physical Therapy Association, American Academy of Orthopaedic Manual Physical Therapy, and the American Academy of Physiological Medicine and Dentistry. He lectures internationally at various medical conferences and on the adverse effects of breathing pattern disorders and chronic sympathetic overload on the human body. Bill Esser, MS, PT, CCTT, graduated in 1979 with a master’s degree from Purdue University and in 1981 from the University of Iowa Graduate Program in Physical Therapy. Bill‘s career has been as an outpatient orthopedic physical therapist including being an owner/partner in private practices in Southern Oregon 1986-2013. He retired from ownership in 2013 to concentrate on teaching. He is a diplomate of the Physical Therapy Board of Craniofacial Therapeutics, established in 1999 by an international group of physical therapists, and he holds the title Certified Cervical and Temporomandibular Therapist (CCTT). There are fewer than 100 diplomates worldwide. Bill has over 4 decades of multidisciplinary training and clinical experience in management of TMD, complex facial pain, and cranial and cervical spine dysfunction. In 2019, he completed a dental mini-residency under Jeff Okeson, DMD. Bill has been an instructor for Empiridence and Myopain Seminars, Professional Therapies Northwest, and as an adjunct instructor on TMD for the Schools of Physical Therapy at Pacific University and George Fox University. Bill has also taught for the Oregon Physical Therapy Association and Oregon Dental Association on TMD.
Bill Esser, MS, PT, CCTT, graduated in 1979 with a master’s degree from Purdue University and in 1981 from the University of Iowa Graduate Program in Physical Therapy. Bill‘s career has been as an outpatient orthopedic physical therapist including being an owner/partner in private practices in Southern Oregon 1986-2013. He retired from ownership in 2013 to concentrate on teaching. He is a diplomate of the Physical Therapy Board of Craniofacial Therapeutics, established in 1999 by an international group of physical therapists, and he holds the title Certified Cervical and Temporomandibular Therapist (CCTT). There are fewer than 100 diplomates worldwide. Bill has over 4 decades of multidisciplinary training and clinical experience in management of TMD, complex facial pain, and cranial and cervical spine dysfunction. In 2019, he completed a dental mini-residency under Jeff Okeson, DMD. Bill has been an instructor for Empiridence and Myopain Seminars, Professional Therapies Northwest, and as an adjunct instructor on TMD for the Schools of Physical Therapy at Pacific University and George Fox University. Bill has also taught for the Oregon Physical Therapy Association and Oregon Dental Association on TMD.