
Treating obstructive sleep apnea with oral appliance therapy is a rewarding and challenging undertaking. Every doctor/clinician has patients who do not completely respond to oral appliance therapy (OAT.) Once this is known, decisions need to be made to modify treatment for the best possible outcome. In the case study below I will describe how an innovative device was combined with an oral appliance to manage a patient with severe obstructive sleep apnea (OSA).
An 85 year old CPAP intolerant male (neck circumference = 18 inches, BMI = 26) was referred for treatment of severe obstructive sleep apnea. His initial apnea-hypopnea index (AHI) was 46 and his supine-AHI was 51. A Herbst appliance was selected and over a six week period the appliance was advanced to a maximum comfortable protrusion. During this time, he experienced some improvement of symptoms, but was still snoring enough to disturb his wife. An efficacy home sleep study was administered and revealed OAT reduced the overall AHI by 49%, but a residual AHI of 24, with a supine-AHI of 53, and a snore index of 10.9 remained.

At this point, I was left with a clinical decision point of abandoning OAT in favor of PAP therapy, surgical intervention, increasing vertical dimension, and/or adding positional therapy. After speaking with the patient, he wished to exhaust all treatment options before returning to PAP therapy or considering any type of surgery. This left altering vertical dimension of his oral appliance and positional therapy as choices for what to do next.
This patient clearly was an appropriate candidate for positional therapy based on the Cartwright definition: supine-AHI at least twice the non-supine-AHI1. I have always been a strong advocate of positional therapy, but have found compliance with the tennis ball or positioning pillow approach to be poor due to the reliance on punitive techniques to restrict supine sleep. Recently I had read about a new approach for positional therapy devices that are worn around the chest or on the back of the neck and combine body position awareness with increasing levels of vibrations. These devices provide behavioral feedback so supine sleeping is avoided while also monitoring both efficacy and compliance. One article showed that vibro-tactile therapy significantly reduced the overall AHI, percent time SpO2<90%, snoring, and improved the sleep architecture (reduced stage N1 and increased stage N2 sleep) and sleep continuity (significantly reduced arousal index)2. The other article showed that an oral appliance combined with vibro-tactile therapy was far superior than either therapy used separately3.
I obtained a vibro-tactile positional therapy device (Night Shift™, Advanced Brain Monitoring, Carlsbad, CA) (Figure 1) for my practice and offered it to the patient on a trial basis for use in combination with his oral appliance. He agreed to use it for two weeks and return for a follow-up home sleep test. I was impressed with the results. The two therapies, in combination, reduced his overall AHI by 87%, from 46 to 6, with positional therapy contributing to the additional 40% reduction in the overall AHI from OAT alone, a finding consistent with the Dieltjens study3. The HST reported that his snoring index was reduced from 10.9% to 1.8%, and that he slept less than 3% of the night in the supine position (total of 14 minutes) with a supine AHI of 4 (likely explained by the fact that the Night Shift does not initiate feedback for the first 15 minutes of recording time to allow the user to fall asleep). As a result of the trial, the patient purchased a Night Shift device and states he has been sleeping much better with much less daytime sleepiness since the two therapies were combined. His wife is very happy since she no longer is disturbed by his snoring.
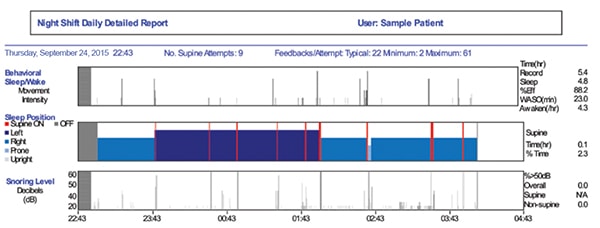
Figure 2 provides an example of the Night Shift report that I used to evaluate the efficacy of the combination therapy. Results showed that this patient had a strong drive to sleep on his back, as he attempted to sleep supine nine times over the course of the night (the red lines identify when these occurred, the thickness indicates how long it took to respond to the feedback). Most patients, on average, attempt to sleep supine five times per night4. He was somewhat of a heavy sleeper in that it typically took him 22 vibrations (or 44 seconds) before he responded to the feedback. Most importantly, his percent time snoring above 50 dB was less than 10%, and his sleep efficiency was greater than 80%, both strong indicators that the combination therapy was effective.
Since as many as 70% of patients diagnosed with obstructive sleep apnea are position dependent2, the potential for vibro-tactile devices in combination with OAT appears to show great promise. The use of positional therapy could reduce the amount of protrusion needed from OAT, since airway patency is easier to maintain in the non-supine position. The potential benefits include greater comfort, reduced side effects, lowered barriers to compliance, and improved efficacy across a wider range of patients. With CPAP intolerant patients, maximizing OAT is imperative. Combining positive airway pressure with OAT may not be an option, so effectively reducing supine AHI (and therefore total AHI) by adding a device like the Night Shift could mean better outcomes for this group of patients.
It is gratifying to effectively manage a patient’s obstructive sleep apnea with oral appliance therapy, and frustrating when we encounter a patient whose problem does not completely resolve. My experience with the patient in this case study will change the way that I look at patients who are not responding completely to oral appliance therapy. In the future, I will be considering combination therapy earlier in the course of treatment, maybe even starting patients on it if there is a strong pre-treatment positional component. I believe that vibro-tactile devices will become an integral part in the treatment of OSA in my practice. It is exciting when an innovative therapy comes along that can be combined with oral appliance therapy to improve patient outcomes.

Stay Relevant With Dental Sleep Practice
Join our email list for CE courses and webinars, articles and more..
