The Problem
The Problem
Ankyloglossia, or tongue-tie, is a common congenital abnormality where the lingual frenum is overly short and tight (posterior ankyloglossia) or aberrantly attached anteriorly to the ventral surface of the tongue (anterior ankyloglossia),1 “tying” the tongue to the floor of the mouth.
The tongue is an important morphofunctional organ which is largely responsible for orofacial development and growth. Ankyloglossia has been linked to abnormal (deviant) suction swallow pattern in newborns2-4 and chewing in infants; it frequently leads to speech disorders.5 Aberrant lingual frenum results in low tongue position and tongue thrusting which contributes to the formation of high and narrow palatal vault – one of the features favoring collapse of the upper airway during sleep6,7 – malocclusion, prognathism, distortion of “harmonic face”8 with the mid third of the face smaller than the upper and lower thirds, and, most importantly, mouth breathing.9 Mouth breathing may be a factor in tonsillar enlargement – it increases upper airway resistance10 causing micro trauma to the back of the throat, inflammation and tonsillar growth. Hypertrophic adenotonsils, in turn, obstruct the airflow and exacerbate mouth breathing, and contribute to the abnormal orofacial growth. Therefore, tongue-tie potentially creates a vicious circle with the potential outcome in the form of sleep disordered breathing (SDB) and obstructive sleep apnea (OSA).
The tongue, which has origin and insertion points ranging from the internal portion of the mandible down to the hyoid bone, has many myofascial and muscular attachments to the cervical muscles. … ankyloglossia is associated with hyperactivity of the suprahyoids and forward displacement of the head. The restricted tongue requires the use of accessory muscles to perform functions such as breathing, breastfeeding, chewing and swallowing. This hyperactivity of the cervical muscles causes shortening of the muscles and induces forward head posture.11
Furthermore, ankyloglossia encumbers the proper function of a temporomandibular joint (TMJ). In the presence of restrictions, movements are compensatory leading to change in bony structure. Such change calls for further accommodations and compensations, which are stressors to the central nervous system. Attaining jaw stability is one of the most important goals of orofacial myofunctional therapy (OMT). Without jaw stability, proper function may not be achieved and the need for compensations is engaged.
The anatomical changes seen with ankyloglossia lead to development of abnormal anatomic support of the upper airway12 that is at a higher risk of collapse during sleep.
Frenectomy
Treatments for ankyloglossia include lingual frenectomy.2,13-17 This is a surgical procedure that leaves a diamond-shaped surgical wound, the edges of which are approximated and sutured or left to heal by secondary intent.15 Tongue-tie revision can be performed with a variety of techniques, e.g., frenotomy, z-plasty, y-plasty, and others. The procedure includes the removal of the frenal tissue and sometimes division of muscle fibers at the lingual base, taking care not to involve vascular structures and nerves under the tongue or the sublingual glands located on both sides of the frenum close to where it attaches to the floor of the mouth. When the frenal attachment is fibrous, some form of anesthesia is usually indicated.
Surgical Modalities for Lingual Frenum Revision
A number of surgical modalities have been utilized for tongue-tie revision, such as scissors, scalpel, and electrosurgery. Most up-to-date techniques involve lasers.13-17 The disadvantage of a conventional tongue-tie revision with a scalpel is intra-operative bleeding (which entails poor visibility of the site and creates the potential for scarring), need for sutures, post-operative discomfort, and the risk of infection. Use of electrocautery is not recommended in patients with old pace makers and in close proximity to orthodontic devices or implants; the thermal injury may prolong healing. Special attention must be paid to avoid thermal injury to the underlying periosteum and bone.
With CO2 laser frenectomy, patients reported less post-operative pain and discomfort than with the scalpel.14 Erbium lasers have been effectively used for lingual frenectomies, but the clinician needs to manage intra-operative bleeding, because erbium laser is not an efficient coagulator. CO2 laser cuts while coagulating capillaries and small blood and lymphatic vessels; this creates a clear surgical site and helps minimize post-surgical edema. Typically, tongue-tie revision with the CO2 laser does not involve suturing of the wound, and usually there is no scar. Minimal to no scarring is critical for post-operative OMT exercises that involve the tongue. Most of the time, patients quickly return to everyday routine immediately after the tongue-tie revision procedure, and are advised to follow the prescribed OMT program.
Tongue-Tie release in combination with OMT
The area to be operated on is much better defined when muscles are toned, therefore myofunctional therapy is a must before release of the frenum. Once restriction is removed, post-frenectomy OMT is also necessary in order to re-establish the swallowing, chewing, speaking and breathing patterns acquired as a result of the tongue-tie18. Repetition of the pattern entrains behavior which helps to establish jaw stability. Length of time of therapy before and after the release is established by the myofunctional therapist depending on the overall goals of the patient. Without such therapy, the incorrect swallow, speech impediments and compensatory posture and breathing habits remain, which can eventually lead to the relapse of OSA and a return of pre-operative sleep disordered breathing and other disorders.
Understanding the continuous interaction between muscle activity of the tongue and other oral-facial muscles, as well as the development of normal anatomic structures supporting the upper airway may lead to expansion of myofunctional reeducation as a therapeutic tool.19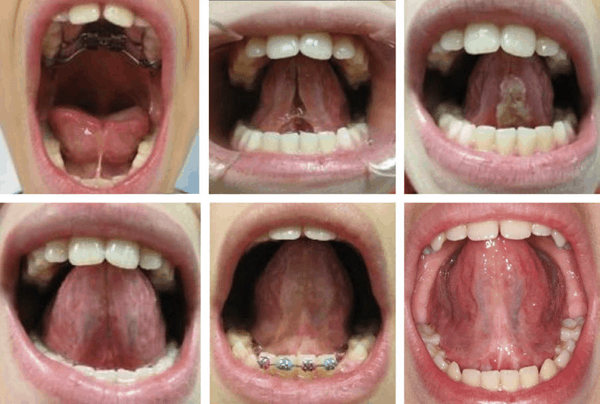
Tongue-Tie FUNCTIONAL RELEASE
Surgical goals of tongue-tie release are different for infant and adult. Infant lingual frenectomy14,20 pursues proper eating/breastfeeding and nasal breathing. Adult needs are much more diverse. Constant, repetitive, and incorrect use leads to deformation and damage done to orofacial structures that needs to be corrected. Therefore, the release is more extensive than for the infant, and it also involves the mandatory pre- and post-frenectomy myofunctional therapy.
Authors’ technique for the adult Tongue-Tie FUNCTIONAL RELEASE, includes the following steps:
- Pre-surgical OMT exercises to prepare and re-pattern tongue function once released;
- SuperPulse CO2 laser frenectomy, preferably under topical anesthesia and combined with Tongue Movement Assessment for ideal Release to achieve optimal function;
- Post-surgical OMT exercise program to ensure long-lasting functional results.
The Tongue-Tie FUNCTIONAL RELEASE is illustrated by clinical cases in Figures 1-3. Note both the immediate and the long-term improved mobility and lift of the tongue. The highly controlled hemorrhage, sealed lymphatics and significantly reduced zone of thermal impact result in less edema and discomfort to the patient. Magnification during the frenectomy is highly recommended as large blood vessels and nerves are in close proximity to the surgical site. Authors prefer to use topical anesthesia to increase the reliability of tongue function during the release. Topical anesthesia does not restrict tongue movement during the procedure when real-time assessment takes place.
In order to rebuild the necessary orofacial function in adult patients, it is not always sufficient to stop at just removing the extra connective tissue that is the aberrant frenum. Once the frenum is removed, the clinician should reassess the function. The clinician must take into account the jaw range of motion, the floor of the mouth flexibility, and the tongue’s ability to elevate, protrude, and achieve lateral functions. This will assist in determining if a full released was achieved. Therefore, the clinician should proceed slowly and cautiously in the middle of the site and to release tension thus allowing for full movement of the tongue.
It is important to remember that full range of motion is not always possible due to other limitations, i.e. clinician needs to know when to stop to achieve the maximum benefit. Frenum that restricts proper lingual motion feels tight to finger pressing in. Unrestricted tongue feels soft. To feel for restrictions one can grasp the tip of tongue with gauze and gently pull the tongue upwards.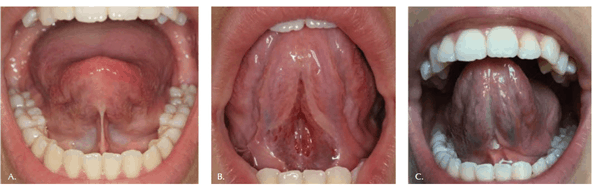
The patient typically returns to the dental office for healing assessment and myofunctional therapy weekly. The team then reviews and re-evaluates the benefits achieved. This is necessary for evaluation of the performance of the tongue, the tone and function changes of the lingual muscles and the suppleness of the healing tissue at the surgical site.

Why CO2 laser?
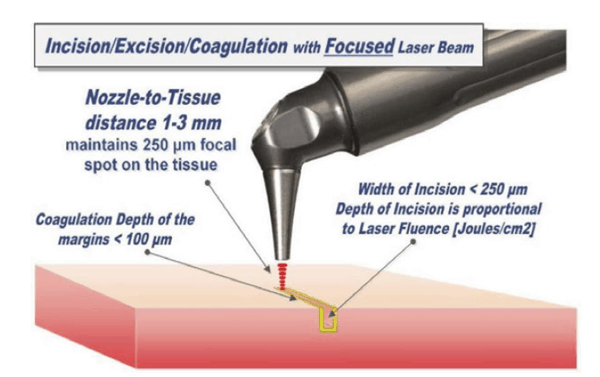
- Not all lasers are equally efficient at both tissue vaporization (i.e., ablation or cutting) and coagulation. The difference is illustrated in the absorption spectra for main soft tissue chromophores21-23 in Figure 4. The advantages of CO2 lasers in oral soft tissue surgeries include:
- Combination of the CO2 laser wavelength and SuperPulse settings, which allows for a char-free and bloodless surgery. It allows, as seen in Figure 4, for approximately 1,000 times more cutting efficiency than dental diodes, and for approximately 10 times more coagulating efficiency than erbium lasers;
- Controlled, repeatable and reproducible speed of tissue removal;
- Coagulation depth of SuperPulse CO2 laser closely matching the blood capillary diameters20,22,24 as illustrated in Figure 4. It allows, unlike with erbium lasers, for an instant hemostasis during high speed ablation/cutting. It affords the clinician improved visibility of the surgical field and therefore allows for more precise and accurate tissue removal;22-24
- Highly controllable depth of incision with dynamic range from micrometers to millimeters. It is proportional to laser power and inversely proportional to laser beam spot size and the surgeon’s hand speed;23,25
- Laser beam focal spot diameter determines the quality of the laser cut. For cutting, the LightScalpel SuperPulse CO2 laser handpiece is maintained 1-3 mm away from the tissue and is moved at a hand speed of a few millimeters per second as illustrated in Figure 5. For a rapid switch from cutting to just photo-coagulation, the laser beam can be defocused by simply moving the handpiece away from the tissue (by approximately 5-10 mm for LightScalpel tipless laser handpieces from Figure 5), and “painting” (sweeping/scanning/”painting” motion) the “bleeder” for enhanced hemostasis;
- Minimal post-operative swelling and edema due to the intraoperative closure of lymphatic vessels on the margins of the CO2 laser incision;25,26
- Reduced post-operative pain and discomfort, as reported with the CO2 laser surgery; 25,26
- Significantly reduced post-surgery production of myofibroblasts, diminished wound contraction and scarring.25,26 As observed in our surgeries, healing with the CO2 laser is markedly different from the other surgical modalities; it is uncomplicated and predictable.
Summary
In order to rebuild the necessary orofacial function in children and adult patients, an extensive Tongue-Tie FUNCTIONAL RELEASE includes the mandatory pre- and post- frenectomy myofunctional therapy and the SuperPulse CO2 Laser frenectomy, preferably under topical anesthesia and combined with Tongue Movement Assessment for Ideal Release to achieve optimal function.
The choice for the CO2 laser wavelength and pulsing settings is based upon its unique absorption coefficient by the water-rich soft-tissue. Decreased wound contraction combined with minimal lateral tissue damage, less traumatic surgery, precise control over the depth of incision, and excellent hemostatic ability make the SuperPulse CO2 laser a safe and efficient alternative to scalpel, electrosurgery, electrocautery, diodes and erbium lasers.