by Melissa Mugno, OMT, RDH, and Tara Erson, DMD
Frenum Release Methods
Frenum release may be performed with a scalpel, scissors, electrocautery or lasers. Procedure performed with a scalpel or scissors can result in significant bleeding, obscuring the surgical field and making it difficult to ensure if the restriction has been completely removed. Due to the contact nature of conventional procedure, there is a certain potential for infection; in addition, higher levels of postoperative pain and discomfort have been reported.1,2
Electrocautery and a hot glass tip of dental diodes may leave a fairly substantial zone of thermal tissue necrosis,3 leading to delayed healing, significant post-operative pain4 and scarring. Erbium lasers produce excellent incisions, but are not sufficient for hemostasis and coagulation.3 The 10,600-nm CO2 laser has been shown to accurately incise soft tissue, with simultaneous efficient hemostasis and coagulation. The photo-thermal coagulation depth of this wavelength closely matches the diameters of small oral soft tissue blood and lymphatic vasculature.1,3 This helps maintain a clear surgical site and reduces the risk of postoperative edema.
Frenuloplasty and Role of OMT
Improperly formed orofacial structures and aberrant deglutition, mastication, speech, and breathing habits may develop due to deviant oral posture and oral restrictions. The authors, therefore, believe that in order to achieve optimal orofacial function in older children and adults, oral restrictions should be surgically removed (via frenectomy or frenuloplasty), and this must be combined with consistent pre- and post- surgical orofacial myofunctional therapy (OMT).1,5 Lingual frenuloplasty is the division of restrictive frenum, that involves closing the mucosa rather than leaving the surgical wound heal by second intention.6,7
It is hard to overstate the significance of OMT. The goal of OMT is to strengthen the tongue and orofacial musculature and establish proper functioning of the tongue, lips, and mandible. OMT utilizes the association between nature’s muscular and behavioral forces and the normalizing bioadaptability of soft and hard orofacial tissues. It helps re-educate the tongue and orofacial muscles, to create new neuromuscular patterns for proper oral function, including mastication, deglutition, speech, and breathing.8,9 Camacho et al.10 showed the reduction of apnea-hypopnea index in children and adults following myofunctional therapy. Without such re-education therapy, deviant oral and breathing habits may persist, eventually resulting in the recurrence of airway and sleep issues that existed prior to the release of oral restrictions.1,8
Functional Laser Frenuloplasty

The frenum release in adults is often more extensive than in infants or young children; and along with the mandatory pre- and post-frenectomy myofunctional therapy, it often involves bodywork and/or speech therapy, etc., if necessary, based on the individual needs of a particular patient. For example, muscular compensations can cause muscle tension and tightness that need to be addressed prior to frenuloplasty, i.e., patient may require pre-release care to help start loosening and aligning the joints affected by oral restrictions. Such collaboration between the frenuloplasty provider and bodyworker may help resolving chronic pain, headaches, airway obstruction, and digestive issues). The authors’ technique for the adult Functional Laser Frenuloplasty, involves the following key components:
- Mandatory regular pre-frenuloplasty OMT exercises to prepare and re-pattern tongue function (in order to facilitate the frenum release as well as the postoperative OMT);
- CO2 laser frenum release (frenuloplasty) and placing sutures, under local anesthesia, combined with tongue mobility assessment to assure effective removal of restrictions for optimal oral function;
- Mandatory post-surgical OMT program to attain long-lasting functional results.
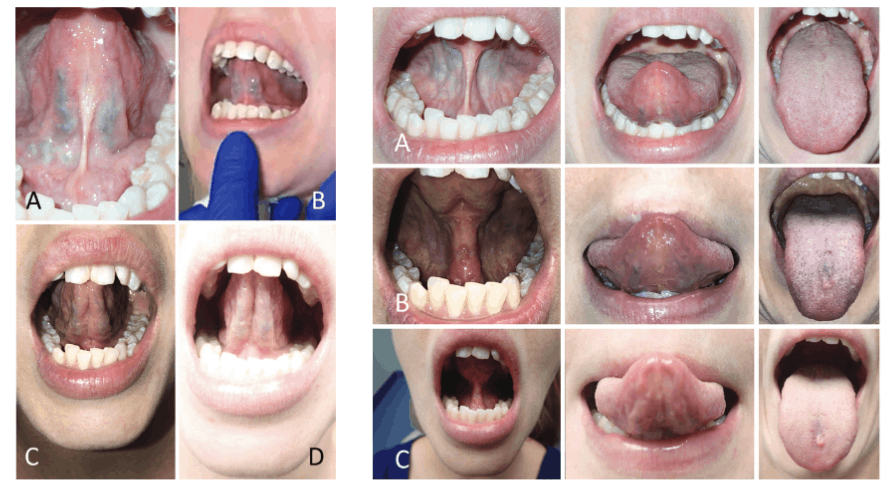
The Functional Laser Frenuloplasty is illustrated by the case study below. Note both the immediate and the long-term improved mobility and lift of the tongue. The well controlled hemorrhage, sealed lymphatics and significantly reduced zone of thermal impact result in less postoperative edema and discomfort to the patient, than the release performed with an electrosurge or diode. Magnification is encouraged during frenuloplasty due to the close proximity of the surgical site to large blood vessels and lingual nerve.
Once the initial frenal restriction is removed, the clinician or the myofunctional therapist should re-access the function. The clinician/myofunctinal therapist must consider the range of motion of the mandible, the flexibility of the mouth floor, along with the patient’s ability to elevate, extend, and lateralize the tongue. This will assist in determining that a full released was achieved. Therefore, the clinician should proceed slowly and cautiously in the middle of the site (taking care to avoid large blood vasculature and lingual nerve) and to release tension to attain full movement of the tongue.
After laser frenuloplasty, the patient typically returns for post-op evaluation at varying intervals (starting 72 hours post-op, to see the myofunctional therapist, resume OMT and obtain bodywork, if necessary, and 7 days post-op to see the frenectomy provider). This is important for assessing the mobility of the tongue, the tone and function changes of the lingual muscles and healing of the surgical site.
Case Study
A 32-year-old Caucasian female presented with TMJ issues, headaches/migraines, neck and shoulder pain, and restricted tongue (Figure 1A).
The patient had a long face with low muscle tone, and showed mid-face and low-face deficiency (Figure 1A).
The patient had breathing issues: her tonsils were enlarged; her nighttime breathing habits included mouth breathing in her sleep and snoring; and she experienced fatigue and sleepiness during the day; she reported bruxing at night. Her lips were apart, when at rest.
She had developed neck muscle compensations which were apparent when she put the tongue into the “suction-cup” position (Figure 2F). She had slight facial asymmetry. The patient had incorrect swallowing patterns with tongue thrust, and both mentalis and buccinator activity.
She had a slightly forward head posture, as can be seen in Figure 1A. In the past, she had a tongue piercing which exacerbated improper (low) resting tongue posture (tongue resting on the teeth), which does not allow for normal resting relationship between teeth and jaws.11
Intraoral examination revealed narrow, flattened dental arches and posterior overjet (Figure 2A-D). Teeth crowding was present in both jaws, along with a midline discrepancy (Figure 2A-D). The tongue appeared wide, with scalloped edges (see the right image in Figure 5A). A thick, very tight, restrictive lingual frenal attachment was noted (Figure 2D and 2E).
The following measurements were taken: the initial basic range of motion (ROM) was 41 mm, and the ROM with tongue tip to incisive papilla (TROM) was 32 mm. The functional ROM, therefore, was 78%. The premolar to premolar distance was 31 mm.
Planned Treatment

The patient treatment (with pre-frenum release OMT, mandibular and maxillary expansion (maxillary – with a removable 3-way sagittal appliance and mandibular – with a removable biobloc), CO2 laser frenectomy, and post-frenum release OMT) was estimated at 12-14 months and the patient is currently in month 7.
By the day of frenum release, the patient had already undergone 12 weeks of OMT (both in-office and at home) and expansion (Figure 1B). Expansion was intended to create the necessary additional space for the tongue, as well as to gain some forwarded facial growth and better occlusion to help with the patient’s ability to chew. 6 weeks prior to frenum release, the myofunctional therapist introduced the patient to Buteyko breathing techniques to strengthen the tongue and improve nasal breathing; most Buteyko exercises were done when the patient’s palatal expander was first delivered.
After several weeks of myofunctional therapy, the patient plateaued and could not progress further with her exercises, due to restrictive lingual frenum. At this point, the dentist decided to perform frenum release with a CO2 laser.
Prior to the frenum release procedure, in addition to OMT and expansion, the patient worked twice with a licensed massage therapist (LMT) – another member of our multidisciplinary team – to address her neck and shoulder tension and to obtain a myofascial release. The LMT performed another treatment after the frenectomy procedure.
Day of Laser Frenuloplasty
The day of frenuloplasty, the patient’s facial muscle tone was visibly improved (Figure 1B). Her jaw line was more defined and nasolabial folds appeared less pronounced (Figure 1A and 1B). Her neck appeared longer due to improved head posture. Both the dentist and myofunctional therapist examined the patient prior to the laser procedure to confirm the patient was ready for frenuloplasty.
Laser Frenuloplasty

After a mixture of Lidocaine 2% with 1:100,000 epinephrine was administered by local infiltration, the LightScalpel laser frenuloplasty was performed to release both the maxillary labial and lingual restrictions. LightScalpel® CO2 laser (LightScalpel, LLC, Bothell, WA) with 0.25 mm focal spot size laser handpiece was utilized, delivering 2 watts repeat, non-SuperPulse laser beam gated at 50% duty cycle at 20 Hz (average power to the tissue was 1 watt). For efficient incision, in order to create tension and ensure that the larger vasculature is pushed away from the surgical site, the patient was asked to put her tongue in the “suction-cup” position (Figure 3A). (OMT prior to a functional frenum release is necessary in order to tone the lingual muscles and ensure the patient’s ability to create and maintain tongue suction.) The dentist applied gentle traction with her fingers, while performing the release (Figure 3B). When performed with scissors, this technique requires the use of a hemostat to clamp smaller blood vessels prior to sharp dissection. With the CO2 laser no hemostat is typically necessary, because smaller vasculature (under 0.5 mm) is efficiently coagulated by the 10,600 nm laser wavelength.
The laser nozzle was held 1-2 mm away from the target tissue (Figure 3B) and moved in a steady hand speed for controlled depth of incision motion. The myofunctional therapist was present throughout the entire procedure. In the course of the procedure, the dentist stopped several times, while the therapist assessed the remaining tension and the tongue mobility. First, after the dentist removed the most apparent, superficial fascial restriction, the myofunctional therapist measured the basic range of motion (ROM), palpated the tongue, using gentle experienced touch and trying to locate the presence of tightness or restriction. The patient was asked to lift, extend the tongue, and put it in the “suction-cup” position.
The patient was already able to protrude and elevate her tongue better, but there was still tension and the dentist proceeded with a deeper release. At this point, no cutting was done; instead, blunt dissection was used to divide deep fascia – this technique helps the natural release, almost “melting”, of fascia. After that, the patient reported the sensation of the front neck tension alleviation. By the end of the procedure, the myofunctional therapist felt release of the tension in the mid portion of the tongue, where a big knot had been detected during preoperative examination. Finally, the last bit of tension detected by the myofunctional therapist was addressed by extending the incision vertically, upward, with the laser (Figure 3E).
The dentist pointed out that if she decided to not suture the surgical site, she would have ablated mucosa laterally (and created more of a diamond shape, as she does in infants and toddlers). For this patient, however, the frenum release was more linear (vertical) (Figures 3D and 3F) and sutures have been placed to facilitate healing without the need to worry about postoperative wound management to prevent return of ankyloglossia and begin OMT 72 hours postoperatively (Figure 3H).
Aftercare and OMT Following Laser Frenuloplasty
Our office typically recommends 400-800 mg of Ibuprofen every 6-8 hours for adult patients, depending on the patient’s pain level, for 48 hours after the frenum release. During this time, the patient is advised to maintain a soft, bland diet and to abstain from hot, spicy or astringent food or drinks.
The dentist saw the patient one week after the laser release. Under supervision of the myofunctional therapist, the patient resumed her OMT exercises, 72 hours after frenectomy. Two bottom sutures snapped during exercise, but this did not affect healing or the patient’s ability to proceed with OMT. The patient was able to elevate the middle and posterior portions of the tongue to the palate, and more easily go through myofunctional exercises that she had previously found challenging.
Three weeks after her frenum release, the patient’s teeth clenching decreased by 75%. Five weeks following frenuloplasty and routine OMT, the patient reported feeling significantly better. Tightness in neck and back were almost completely gone and she noted the decrease in chest tightness. Although the patient’s basic range of motion has remained 41 mm, her tongue-to spot range of motion (TROM) has increased from 32 mm to 40 mm (i.e., 25% increase).
In addition to her OMT routine, the patient regularly attends a chiropractor, 2-4 times a month. She will continue with her expansion for another 8-12 weeks, as she relapsed a bit due to being sick and unable to wear the expander at night. Her maxilla has expanded from 31mm to 39 mm (from premolar to premolar). Although the patient has already seen significant improvements in her symptoms, she intends to continue her OMT, working on maintaining proper orofacial habits and further improving and maintaining better posture.
Summary
In adults, optimal orofacial function can be attained through the deep functional release1 of restrictive frenal attachments and re-education of orofacial soft tissues. The functional laser frenuloplasty consists of the following three equally important parts: 1) methodical pre-frenuloplasty OMT; 2) CO2 laser release of tethered oral attachments performed with the frequent assessment of the tongue mobility and the presence of tension (to achieve the maximum ROM and ensure that there are no anatomical obstacles in the way of the patient’s myofunctional therapy); and 3) methodical post–frenuloplasty OMT. The authors strongly feel that the ability to provide extensive OMT, bodywork and deep lingual frenum release within the same practice ensures that the patient receives the most comprehensive treatment in a familiar environment, and without the need to travel to multiple providers. Importantly, all the team members are well familiar with the patient’s treatment plan and closely follow the patient’s progress.
The authors find that the minimal thermal tissue change, less traumatic surgery, predictable incision depth, and ability to achieve hemostasis, make the 10,600 nm CO2 laser an excellent surgical alternative to scissors or diode hot tip devices.
Acknowledgments
Authors greatly appreciate the help and contribution from Anna (Anya) Glazkova, PhD, and Peter Vitruk, PhD, in preparing this material for publication.
To read more about functional laser frenuloplasty, read CO2 laser functional frenectomy here.

