by Dr. Derek Mahony and Dr. Kevin Williams
Table of Contents
Abstract
This article reviews upper airway obstruction caused by hypertrophied adenoids and the possibilities of a subsequent malocclusion. Early diagnosis and treatment of pathological conditions that can lead to the obstruction of the upper airways is essential to anticipate and prevent alterations in dental arches, facial bones, and muscle function.
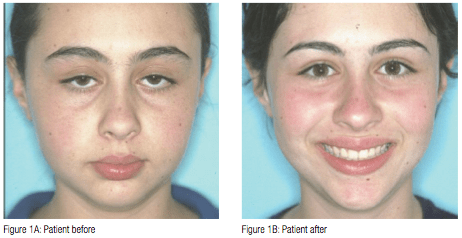
Correct nasal breathing facilitates normal growth and development of the craniofacial complex (Figures 1A and 1B). Important motor functions such as chewing and swallowing depend largely on normal craniofacial development. Any restriction to the upper airway passages can cause nasal obstruction possibly resulting in various dentofacial and skeletal alterations.1 Upper respiratory obstruction often leads to mouth breathing (Figure 2). Habitual mouth breathing may result in muscular and postural anomalies, which may in turn cause dentoskeletal malocclusions2 (Figure 3). Hypertrophy of the adenoids, and palatine tonsils, are one of the most frequent causes of upper respiratory obstruction (Figure 4). Philosophies regarding the treatment of adenoid hypertrophy range from dietary control and environmental modifications to dentofacial orthopaedics, change of breathing exercises, and surgical procedures.
Introduction
The methodology used in this literature analysis consists of a thorough review of narrowly tailored research and journal articles. The paradigm explored in each article involves upper airway obstruction, adenoid hypertrophy, and malocclusion. The results and conclusions stemming from these articles generally fall into three categories:
- That hypertrophied adenoids have a definitive effect resulting in skeletal malocclusion.3
- That hypertrophied adenoids, coupled with other factors, may aid in the development of skeletal anomalies.4
- That adenoid hypertrophy has no effect on airway obstruction and malocclusion.
The research in this area is expansive, but largely inconsistent. Thus, the cause-and-effect relationship of adenoid hypertrophy and malocclusion must be carefully examined on a case-by-case basis.5 Regardless of the various researchers’ conclusions, one theory remains common — that airway obstruction caused by adenoid hypertrophy and malocclusion are related. The degree of that relationship and what it affects is still under debate. This paper attempts only to highlight the positive existence of this relationship and its possible effects regarding dentofacial growth and development.
Basic facial growth and development
Developments in the understanding of human craniofacial growth have stemmed from histological and embryologic studies, radiographic cephalometry, correlation of growth and facial anomalies analysis of surgical interventions, animal research, and other science fields.6 Despite these studies, we are still waiting for a definite consensus regarding the controlling mechanism of craniofacial tissue.
Postnatal facial growth is influenced by genetic and environmental factors.2 Most facial growth and development occurs during the two childhood growth peaks. The first growth peak occurs during the change from primary to permanent dentition (between 5 and 10 years of age) and the second growth peak occurs between 10 and 15 years of age.2 The study of the early years of life shows that by the age of four, 60% of the craniofacial skeleton has reached its adult size. By the age of 12, 90% of facial growth has already occurred.7 By age seven, the majority of the growth and development of the maxilla is complete and by age nine, the majority of the growth and development of the mandible is complete. Proper facial growth is affected either positively or negatively, early in life, by the sequential occurrences of four major factors:
- The cranial base must develop properly.
- The naso-maxillary complex must grow down and forward from the cranial base.
- The maxilla must develop in a linear and lateral fashion.
- A patent airway must develop properly.
The relationship between the naso-maxillary complex anud the cranial base is significant for esthetic reasons and proper facial bone, muscle, and soft tissue support. To allow proper downward and forward rotation of the mandible, the maxilla must be adequately developed, in width, for acceptance of the mandible. Any limitation on mandibular rotation may affect the relationship of the condyle to the glennoid fossae (in the temporal bone) resulting in multiple TMJ problems. An improper airway will affect the global individual growth.8 The simultaneous growth of these factors is not nearly as significant as how these factors interrelate during facial growth and development. For example, the basic design of the face is established by a series of interrelated factorial developments. The naso-maxillary complex is associated with the anterior cranial fossae. The posterior boundary of the maxilla determines the posterior limits of the midface. This structural plane is significant to facial and cranium development. The basic structural format of facial growth and development is dependent on, and governed by, the interrelation of multiple functional matrices. These functional matrices include a phenomenon of bone displacement and growth at the TMJ with the maxillary forward and downward movement equaling mandibular growth
upward and downward. The displacement and growth phenomenon is responsible for the spatial relationship necessary for functional joint movement resulting in the final result of facial growth.9 Additionally, muscle adaptions affect dentoskeletal development. The integration of the musculoskeletal system affects respiration, mastication, deglutition, and speech.2
This basic understanding of facial growth and development is relevant as adenoidal tissue enlargement coincides with major facial growth; that is, they occur simultaneously. Facial growth may be restricted by abnormal development of adenoidal tissue resulting in abnormal swallowing and breathing patterns (Figure 5).
Adenoidal growth and development
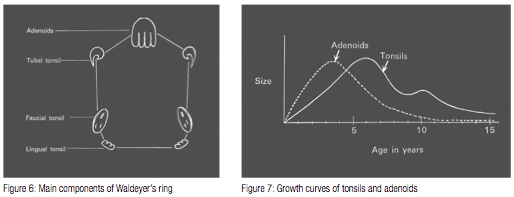
Lymphoid tissue is normally present as part of the Waldeyer’s tonsillar ring in the form of a nasopharyngeal tonsil (Linder-Aronson 1970). The Waldeyer’s ring is the system of lymphoid tissue that surrounds the pharynx. This system of tissue includes adenoids and pharyngreal tonsils, lateral pharyngeal tonsils, lateral pharyngeal bands, palatine tonsils, and lingual tonsils (Figure 6). Tonsils and adenoids have disparate embryonic origins and cytology even though they are both part of Waldeyer’s ring.10 Bacteria may play a role in adenoid hyperplasia. Specifically, different pathogens, such as Haemophilus influenza and Staphylococcus aureus, have been associated with lymphoid tissue hyperplasia. The adenoid lymphoid structures are lined with ciliated respiratory-type epithelium, which is normally distributed throughout the upper and posterior nasopharynx walls. During the presence of disease, the distribution of the dendritic cells (antigen presenting cells) is altered. The result is that there is an increase in dendritic cells in the crypts, and extrafollicular areas, and a decrease in surface epithelium dendritic cells.
 Lymphoid tissue is normally not apparent in the early infant stage of life. Marked symptoms of adenoid development are most common in the childhood age range of 2–12. During adolescence, a decrease in adenoid size is noted as current with the growth of the nasopharynx. Rarely is adenoid tissue present in adults, and when it is noted, it is usually in an atrophic condition. The cause of the involution of the Waldeyer’s ring is still under investigation.12 The imbalance in the relationship between the enlargement of the nasopharynx/nasopharyngeal airway and the concomitant growth of adenoid tissue can result in reduced patent nasopharyngeal airway and increased nasopharyngeal obstruction.10
Lymphoid tissue is normally not apparent in the early infant stage of life. Marked symptoms of adenoid development are most common in the childhood age range of 2–12. During adolescence, a decrease in adenoid size is noted as current with the growth of the nasopharynx. Rarely is adenoid tissue present in adults, and when it is noted, it is usually in an atrophic condition. The cause of the involution of the Waldeyer’s ring is still under investigation.12 The imbalance in the relationship between the enlargement of the nasopharynx/nasopharyngeal airway and the concomitant growth of adenoid tissue can result in reduced patent nasopharyngeal airway and increased nasopharyngeal obstruction.10
The growth of adenoidal tissue as demonstrated by a bell curve, peaks at or near age six and also begins involution at or near this age as well (Figure 7). Facial growth is coupled with adenoidal growth. As the cranial base forms the roof of the nasopharynx, a close examination of the growth and development of the craniofacial complex becomes significant for evaluation of the size and configuration of the nasopharyngeal airway. Any abnormal development regarding this craniofacial complex may affect the nasopharyngeal airway. Abnormal adenoidal growth that occurs during childhood may consume the nasopharnx and extend through the posterior choanae in the nose.13 This excessive adenoidal growth usually interferes with normal facial growth and can result in abnormal breathing patterns, congestion, snoring, mouth breathing, sleep apnea,4 eustachian tube dysfunction/otitis media, rhinosinusitis, facial growth abnormalities, swallowing problems, reduced ability to smell and taste, and speech problems.12 Theoretically, many clinicians believe the blockage should be removed as soon as possible through a surgical procedure called adenoidectomy. However, according to a study conducted by Havas and Lowinger, one-third of child study patients, with traditional adenoidectomies, were ineffective with intranasal extensions of the adenoids obstructing the posterior choanoe. For this segment of the study population the “powdered-shaver adenoidectomy” was effective in the complete removal of the obstructive adenoid tissue ensuring postural patency.13
Upper airway obstruction and mouth breathing
During normal nasal respiration, the nose filters, warms, and humidifies the air in preparation for its entry into the body’s lungs and bronchi. This nasal airway also provides a degree of nasal resistance in order to assist the movements of the diaphragm and intercostals muscles by creating a negative intrathoracic pressure. This intrathoracic pressure promotes airflow into the alveoli.7,15
Correct normal resistance is 2 to 3.5 cm H2O/L/Sec and results in high tracheobronchial airflow which enhances the oxygenation of the most peripheral pulmonary alveoli. In contrast, mouth breathing causes a lower velocity of incoming air and eliminates nasal resistance. Low pulmonary compliance results.7 According to blood gas studies, mouth breathers have 20% higher partial pressure of carbon dioxide and 20% lower partial pressures of oxygen in the blood, linked to their lower pulmonary compliance and reduced velocity.7,16
Contributing factors in the obstruction of upper airways include: anatomical airway constriction, developmental anomalies, macroglossia, enlarged tonsils and adenoids, nasal polyps, and allergic rhinitis.5 However, for purposes of this paper, the focus shall be on enlarged adenoids as the major contributing factor. There are numerous studies that link adenoid hypertrophy with nasopharyngeal airway obstruction to the development of skeletal and dental abnormalities.14
Airway obstruction, resulting from nasal cavity or pharynx blockage, leads to mouth breathing, which results in postural modifications such as open lips, lowered tongue position, anterior and posteroinferior rotation of the mandible, and a change in head posture. These modifications take place in an effort to stabilize the airway. As previously discussed, facial structures are modified by postural alterations in soft tissue that produce changes in the equilibrium of pressure exerted on teeth and the facial bones (Figure 8). Additionally, during mouth breathing, muscle alterations affect mastication, deglutition, and phonation because other muscles are relied upon.2
Malocclusion — the issue still in debate
Is there a cause-and-effect relationship between adenoids, nasal obstruction, and malocclusion?
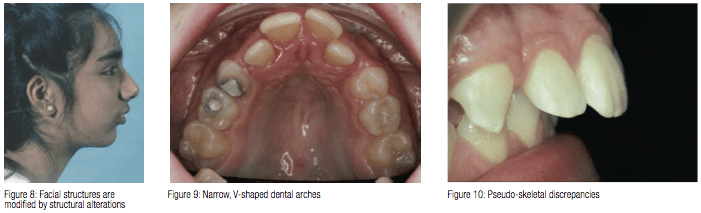
Dentofacial changes associated with nasal airway blockage have been described by CV Tomes in 1872 as adenoid facies. Tomes coined this term based on his belief that enlarged adenoids were the principle cause of airway obstruction and resulted in noticeable dentofacial changes.7 Tomes reported that children, who were mouth breathers, often exhibited narrow V-shaped dental arches10 (Figure 9). This narrow jaw is a result of mouth breathers keeping their lips apart and their tongue position low. The imbalance between the tongue pressure and the muscles in the cheek, result in cheek muscles compressing the alveolar process in the premolar region. Simultaneously, the lower jaw postures back (Figure 10). These simultaneous actions have been termed the compressor theory.11
Tomes’ views were supported in the 1930s by numerous leading orthodontists. These supporting clinicians reported airway obstruction as an important etiologic agent in malocclusion. Rubin advocated that in order for these patients to fully be assessed they must be thoroughly evaluated by both a rhinologist and orthodontist.7 Malocclusion is the departure from the normal relation of the teeth in the same dental arch or to teeth in the opposing arch.3
Airway obstruction, coupled with loss of lingual and palatal pressure of the tongue, produces alterations in the maxilla. The positioning of the tongue also plays an important role in mandibular development. The tongue displaced downward can lead to a retrognathic mandible, and an interposed tongue can lead to anterior occlusal anomalies.
Additionally, maxillary changes can be viewed in the transverse direction, producing a narrow face and palate often linked with cross bite; in the anteroposterior direction, producing maxillary retrusion; and in the vertical direction, causing an increase in palatal inclination as related to the cranial base and excessive increases of the lower anterior face height. The most commonly found occlusal alterations are cross bite (posterior and/or anterior), open bite, increased overjet, and retroclination of the maxillary and mandibular incisors.2 Mahony and Linder-Aronson’s findings were in agreement with the significant correlation between changed mode of breathing and diminished mandibular/palatal plane angle (ML/NL) found in adenodectomized children.22
Several authors have taken the position that alleged faces are not consistently found to be associated with adenoids, mouth breathing, nor a particular type of malocclusion; and that there is no cause-and-effect relationship between adenoids, nasal obstruction/mouth breathing, and malocclusion.
Proponents of this position believe that the V-shaped palate was inherited and not acquired through mouth breathing (Hartsooh 1946). A review of literature related to mouth breathing concluded that mouth breathing is not a primary etiological factor in malocclusion. Additionally, Whitaker (1911) found that in a study of 800 children, who underwent adenoidectomy or tonsillectomy, only 30% had dental anomalies that needed orthodontic intervention. There is some suggestion that adenoids and hypertrophic tonsils are a consequence of a thyroid hormone deficiency. This hormone deficiency acts as a catalyst for activating the organism’s defense mechanisms which include hypertrophy of lymphoid tissue.11 Another orthodontic clinician, Vig, took the position that without documented total nasal obstruction, any surgery or other treatment to improve nasal respiration is empirical and difficult to justify from an orthodontic point of view.7,17
Nasal respiratory evaluation
The relationship of airway obstruction and dentofacial structures/malocclusion is still the subject of investigation and controversy among orthodontists. The correlation between functional problems and morphologic characteristics is yet to be solidified. Regardless of varied opinion in this area, practitioners should observe each patient carefully.
Here is the suggested protocol:
- As the patient enters the room, facial and head posture should be noted to see if the lips are closed during respiration.
- Signs of allergic rhinitis should be noted, as well as histories of frequent colds or sinusitis.
- Assessment of family history for allergies is important.
- Sleep history should be evaluated: sleep apnea, loud snoring, open-mouth posture while asleep.
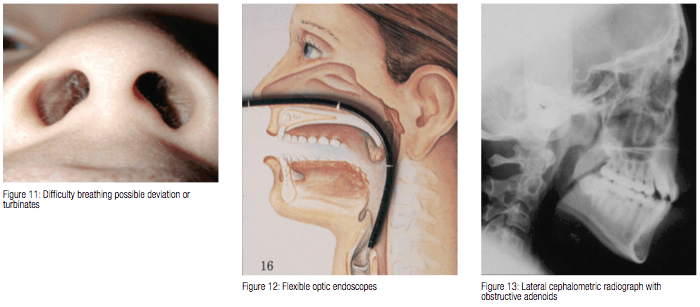
- Patient is asked to seal his/her lips — difficulty breathing through nose should be noted. One nostril can be occluded and the response noted — same procedure on the other side (Figure 11).
The evaluation of nasal airway patency is complicated, especially when the possibility exists that airways may clinically appear inadequate but be quite functional physiologically. Lip separating or an open-mouth habit is not an infallible indicator of mouth breathing. Often complete nasal respiration is coupled with dental conditions that cause open-mouth posture.10
Adenoid evaluation
Nasopharyngeal space and the size of adenoids have been evaluated using different methods of assessment:
- Determination of the roentgenographic adenoid/nasopharyngeal ratio (a lateral cephalometric X-ray)
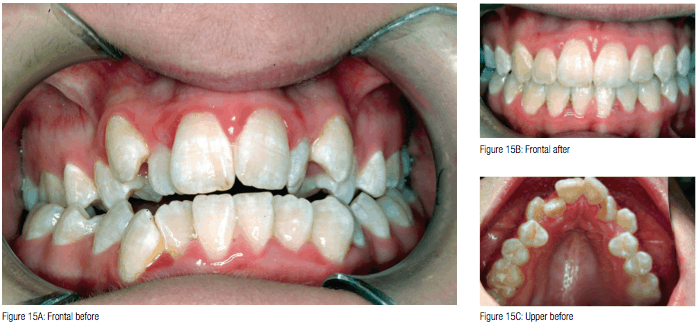
- Flexible optic endoscopes (Figure 12)
- Acoustic rhinometry
- Direct measurements during surgery
Direct measurements are considered to be the most accurate because space can be assessed in three directions.12 A lateral cephalometic radiograph is an added valuable diagnostic tool for the orthodontist in the evaluation of children with upper airway obstructions14 (Figure 13).
 Treatment of nasal obstruction
Treatment of nasal obstruction
- Adenoidectomy with or without tonsillectomy is indicated if hypertrophied adenoids (and tonsils) are the cause of upper airway obstruction.7Powered-shaver adenoidectomy — adenoidectomy coupled with endoscopic visualization will assist in achieving adequate removal of adenoids particularly high in the nasopharnx. Use of the powered-shaver technique allows for better clearance of obstructive adenoids. The end result is more reliable restoration of nasal patency.13
- Septal surgery (rarely indicated in the child) but may be considered in the presence of a marked nasal septal deflection with impaction. Conservative septal surgery in growing patients will not have an adverse effect in dentofacial growth.7,18,19,20
- Maxillary expansion (RME or SAME) — an orthodontic procedure that widens the nasal vault7,18 (Figure 14).
- Cryosurgery or electrosurgery — this is a viable option for patients with vasomotor rhinitis.7
- Bipolar radiofrequency ablation (allergic rhinitis) — performed under local anesthetic.
- Inferior turbinectomy — using powered instrumentation.
- Use of nasal sprays.
Conclusion
The effect of adenoids on facial expression, malocclusion, and mode of breathing has been a topic of debate and investigation by practitioners in the field for the last 100 years. A review of the literature exposes several theories.
A healthcare provider, with a practice philosophy based on prevention of malocclusion development, cannot ignore the early years of the patient’s growth cycle. By age 12, 90% of facial growth has already occurred. This is the age when many practitioners begin orthodontic treatment.7 This is the age when 80%-90% of craniofacial growth is complete, so most formation and/or deformation has occurred.21 To wait until 90% of the abnormality has occurred, before beginning treatment, is not consistent with a preventive philosophy. Interceptive measures must be initiated sooner. Early intervention requires an acceptance of a multidisciplinary approach to total patient health. An integrated approach to patient evaluation, diagnosis and treatment is most effective. Primary care physicians, dentists, allergists, otorhinolaryngologists, and orthodontists must all work together for early prevention and management of young patients with increased nasal airway resistance.
After diagnosis, a comprehensive risk benefit analysis regarding early intervention must be considered. Although hereditary and environmental factors must be considered, the universal goal is the promotion of proper nasal respiration throughout a child’s early years of facial growth.
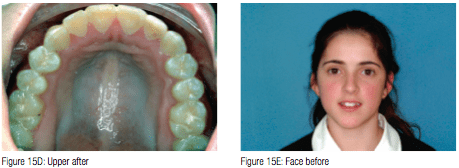

Figures 15A-15F shows the before and after treatment results of a young girl who had her adenoids removed, then underwent maxillary expansion before full-fixed braces. She was treated as a second opinion against the removal of four premolar teeth to relieve dental crowding.
References
- Mattar SE, Anselmo-Lima WT, Valera FC, Matsumoto MA. Skeletal and occlusal characteristics in mouth-breathing pre-school children. J Clin Pediatr Dent. 2004;28(4):315-318.
- Valera FC, Travitzk LV, Mattar SE, Matsumoto MA, Elias AM, Anselmo-Lima WT. Muscular, functional and orthodontic changes in pre-school children with enlarged adenoids and tonsils. Int J Pediatr Otorhinolaryngol. 2003;67(7):761-770.
- Khurana AS, Arora MM, Gajinder S. Relationship between adenoids and malocclusion. J Indian Dental Ass. 1986;58:143-145.
- Pellan P. Naso-respiratory impairment and development of dento-skeletal sequelae: a comprehensive review. Int J Orthod Milwaukee. 2005;16(3):9-12.
- Soxman JA. Upper airway obstruction in the pediatric dental patient. Gen Dent. 2004;52(4):313-316.
- Ranly DM. Craniofacial growth. Dent Clin North Am. 2000;44(3):457-470.
- Rubin RM. Effects of nasal airway obstruction on facial growth. Ear Nose Throat J. 1987;66(5):212-219.
- Pistolas PJ. Growth and development in the pediatric patient. Funct Orthod. 2004-2005;22(1):12-22.
- Enlow DH, Hans MG. Essentials of Facial Growth. New York, NY: W.B. Saunders Co.; 1996: 79-98, 206.
- Diamond O. Tonsils and adenoids: why the dilemma? Am J Orthod. 1980;78(5):495-503.
- Linder-Aronson S. Adenoids. Their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the denition. A biometric, rhino-manometric and cephalometro-radiographic study on children with and without adenoids. Acta Otolaryngol Suppl. 1970;265:1-132.
- Casselbrant ML. What is wrong in chronic adenoiditis/tonsillitis anatomical considerations. Int J Pediatr Otorhinolaryngol. 1999;5;49(suppl 1):S133-5.
- Havas T, Lowinger D. Obstructive adenoid tissue an indication for powered-shaver adenoidectomy. Arch Otolaryngol Head Neck Surg. 2002;128(7):789-791.
- Oulis CJ, Vadiakas GP, Ekonomides J, Dratsa J. The effect of hypertrophic adenoids and tonsils on the development of posterior crossbite and oral habits J Clin Pediatr Dent. 1994;18(3):197-201.
- Adams GL, Boies CR, Papaiella MM. Boies’ Fundamental Oto. Philadelphia, PA: WB Sanders; 1978.
- Ogura JH. Physiologic relationships of the upper and lower airways. Ann Otol Rhinol Laryngol. 1970;79(3):495-498.
- Vig PS, Sarver DM, Hall DJ, Warren DW. Quantitative evaluation of nasal airflow in relation to facial morphology. Am J Orthod. 1981;79(3):263-272.
- Gary LP, Brogan WF. Septal deformity malocclusions and rapid maxillary expansion. Orthodontist. 1972;4(1):2-14.
- Cottle MH. Nasal surgery in children. Eyo, Ear, Nose and Throat Monthly. 1951;30:32-38.
- Jennes JL. Corrective nasal surgery in children. Long term results. Arch Otolaryngol. 1964;79:145-151.
- Mahony D, Page D. The airway, breathing and orthodontics. Ortho Tribune. 8-11.
- Mahony D, Karsten A, Linder-Aronson S. Effects of adenoidectomy and changed mode of breathing on incisor and molar dentoalveolar heights and anterior face heights. Aust Orthod J. 2004;20(2):93-98.

