
by Brian Sung, MD
More than half of Americans are overweight and roughly 12 million Americans have severe obesity (defined as being 100 pounds or more overweight). Obesity, categorized as a body mass index (BMI) of 30 or more, is linked to more than 40 diseases including type 2 diabetes, heart disease, stroke, and obstructive sleep apnea (OSA). Obstructive sleep apnea is a common condition in the general population with increasing prevalence in the obese and morbidly obese populations. Obesity is the most common risk factor for OSA, with over 50% of OSA cases attributable to excess weight¹ and overall incidence that is 12 to 30 fold higher in the bariatric population². As such, OSA commonly coexists with obesity and may exacerbate other obesity-related complications such as type 2 diabetes and hypertension.
Weight loss by any method is a well documented treatment for OSA. Studies have shown that bariatric surgery (also known as weight loss surgery) is an effective tool for treating obesity, and for preventing, treating and even resolving sleep apnea. In general, many patients after bariatric surgery will develop clinical improvement or resolution of symptoms of OSA, regardless of whether a normal BMI is ever achieved, as even a modest weight loss of 10-20% has been associated with improvement of symptoms and greater than 26% reduction in apnea hypopnea index (AHI).³
Data in the literature demonstrates subjective improvement in symptoms of OSA after bariatric surgery which include: improvement in self-reported postoperative sleep quality, reduction in daytime sleepiness, improvement in validated quality of life scores, and improvement in Epworth Sleepiness Scores. And objective parameters regarding severity of OSA have been shown to improve after bariatric procedures including respiratory disturbance index (RDI), AHI, oxygen saturation, and both sleep efficiency and REM sleep on polysomnography testing.
More than two decades ago, the National Institutes of Health (NIH) recognized bariatric surgery as the only effective treatment to combat severe obesity and maintain weight loss in the long term. Based on the NIH consensus, bariatric surgery candidates are patients with a BMI between 35 and 39.9 with at least one obesity related comorbidity or a BMI ≥40. Nearly two thirds of obese patients with severe OSA are good candidates for bariatric surgery.
 Bariatric Procedures
Bariatric Procedures
The most common forms of bariatric surgery are Roux-en-Y gastric bypass, adjustable gastric banding and sleeve gastrectomy. More than 95 percent of all procedures performed are performed using minimally invasive (laparoscopic) techniques. Minimally invasive surgery means faster operations, less anesthesia, much smaller incisions and less scarring, all of which contribute tofaster healing and recovery.
Laparoscopic Roux-en-Y Gastric Bypass
This procedure involves creating a small stomach pouch, so less food can be consumed. The intestine is connected to the pouch and rerouted. Food bypasses the lower stomach, the first segment of the small intestine (duodenum) and part of the second segment (jejunum). A direct connection is created from the small stomach pouch to the lower segment of the small intestine. Patients generally can return to work within three to four weeks.
 Laparoscopic Adjustable Gastric Banding (LAGB)
Laparoscopic Adjustable Gastric Banding (LAGB)
The laparoscopic adjustable gastric banding procedure involves placing an adjustable, inflatable silicone band around the upper part of the stomach. The technique restricts the amount of food that can be eaten and, when properly adjusted, controls hunger. Patients generally can return to work after two weeks. The inner balloon of the band can be incrementally inflated after surgery to increase the feeling of fullness after eating and improve hunger control.
Patients generally recover quickly and return to work within one to two weeks.
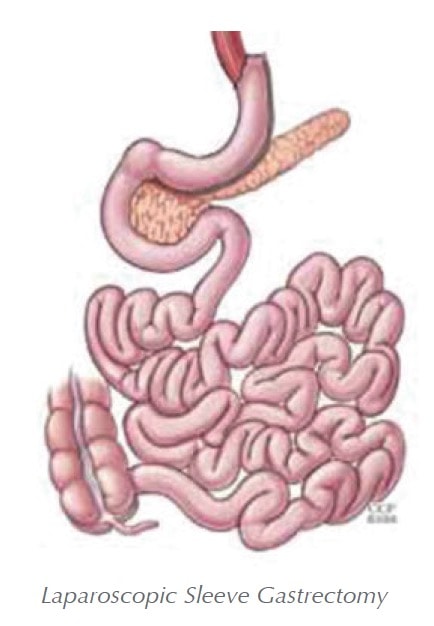 Laparoscopic Sleeve Gastrectomy
Laparoscopic Sleeve Gastrectomy
Laparoscopic Sleeve Gastrectomy (LSG) is a restrictive procedure that reduces the size of the stomach and limits food intake. This procedure may be used as part of a staged approach to surgical weight loss.
Patients who have a very high BMI, who are at risk for undergoing anesthesia or who have a heart or lung problem and should not undergo a long surgical procedure may benefit from this staged approach.
As a stand alone procedure, there is significant evidence that sleeve gastrectomy is comparable in safety and efficacy to gastric banding. Unlike gastric banding, there is no silicone band and no return visits for adjustments are required. Patients generally can return to work within three to four weeks.
Overall, the risks are similar to those seen with the laparoscopic adjustable band, but lower than the risks associated with gastric bypass.
Conclusion
Bariatric surgeries result in long-term weight loss success. Most studies demonstrate that more than 90 percent of individual previously affected by severe obesity are successful in maintaining 50 percent or more of their excess weight loss following bariatric surgery. Several large population studies have found improved longevity in individuals affected by severe obesity who have bariatric surgery with a lower risk of death than those individuals affected by obesity who do not have surgery. In addition to mortality reduction, bariatric surgery also decreases morbidity with improvement or resolution of obesity related comorbidities including hypertension, sleep apnea, asthma, gastroesophageal reflux disease, fatty liver disease, lipid abnormalities, infertility, and more. In addition to improvement in health and longevity, surgical weight loss improves overall quality of life including measures of improved mobility, self esteem, and profession and social interactions. And given that the mortality rate for bariatric surgery (3 out of 1000) is similar to that of a gallbladder removal and less than that of a hip replacement, the benefits of surgery far exceed the surgical risks.
Regardless of which bariatric surgery procedure a patient and their surgeon
decide on, it is important to remember that bariatric surgery is a “tool.” Weight loss
success depends on many important factors such as nutrition, exercise, behavior modification and more. When combined with a comprehensive treatment plan and program, bariatric surgery is an effective tool to provide patients with long term weight loss and overall improvement in their health and quality of life.
Stay Relevant With Dental Sleep Practice
Join our email list for CE courses and webinars, articles and more..