Dr. Tom Colquitt identifies the four types of tonsils and their contribution to our health.
by Tom Colquitt, DDS
Here’s a fact I’ll bet, unless you are a parent of young kids, you haven’t thought much about as a dentist. Lots of kids, even after they have their adenoids removed, continue to have Recurrent Otitis Media (ROM), ineffectively treated with antibiotics and tubes inserted through the tympanic membrane, exposing the middle ear to the outside world. After draining off a pool of pus, the piercing becomes a source of more infection. Often these kids now have problems with their Tubal Tonsils, which hypertrophy and remain infected along with the middle ear.
Everything needed to sustain life comes to us through our nose and mouth. All these structures need to have the correct “Place in Space in the Face” and the airway behind it (thanks to Sandra Kahn for that term). Each has specific functions with shared plumbing, which requires exquisite cooperation between the air conditioning structures and the food processing structures. This functional symbiosis is run by the tongue.
The tongue is the conductor of the business of living and needs to construct its own Linguatorium (my term) in which to run the show, beginning at or before birth.
There is a ring of tonsillar tissue (Waldeyer’s Ring) surrounding the air-gathering pharyngeal structures at the back of the throat. These are essential bits of lymphatic tissue necessary for a properly functioning immune system. The driver is functional nasodiaphragmatic breathing (NDB) and a proper swallow after efficient mastication. All of which is led by coordinated tongue movement within the Linguatorium which it helped create and maintain.
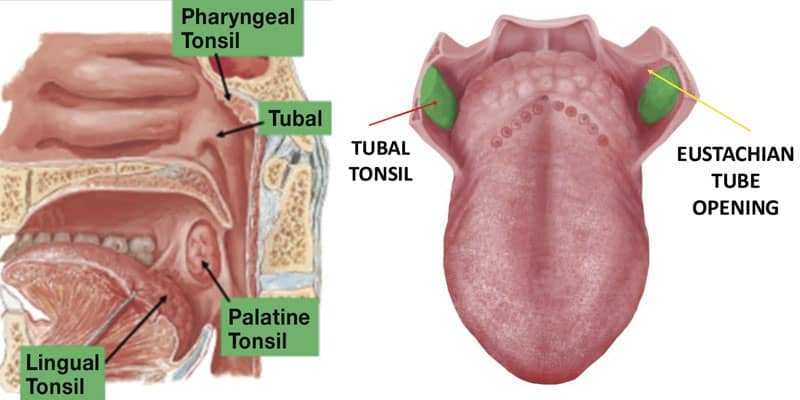
There are bilateral sets of four tonsils surrounding the airway (Figure 1). We can see some of them. Some we can’t. They, along with the nose, are our bodies’ Maginot Line against would-be pathogenic invaders. In 1939, Germany went right around the Maginot Line to invade and occupy France. Airborne pathogens can do the same thing if we have structural, functional, and behavioral breathing problems that permit this to happen. And it happens so much as to be pandemic.
From Top to Bottom
Pharyngeal Tonsils, or Adenoids.
First lymphatic responder in nasal breathing to pathogens and particulates missed by the cilia of the nasal epithelium and the antimicrobial effects of Nitrous Oxide (NO) secreted in the paranasal sinuses. NO is secreted at 200 times the level needed for killing inhaled pathogens, according to Dr. Emet Schneiderman of Texas A&M College of Dentistry.
As such, the nose is our natural first responder, and we as homo sapiens are hardwired for naso-diaphragmatic breathing. The released NO also potentiates the activity of the cilia in the airway epithelium to expel inhaled noxious particulate matter.
In addition to killing microbes, nasal inhalation warms, moisturizes and filters incoming air before it can reach the Adenoids and other tonsils.
Nasal breathing to and from the diaphragm utilizes all the lung volume, whereas shallow mouth breathing uses the intercostal muscles and only the top third of the lungs. The diaphragm is the pump for the immune system.
You can see that the Pharyngeal Tonsils (Adenoids) are part of the back of the throat. Since they have no capsule like the Palatine Tonsils, it is virtually impossible to completely remove them surgically without damaging this part of the pharyngeal wall. Let’s continue our tonsillar tour.
Next Drainage Stop: The Tubal Tonsils
They are located at the pharyngeal opening of the Eustachian Tubes (Figure 2) to keep bad stuff from crawling up the ET and causing a middle ear infection. Tongue movement and proper swallow mechanics opens the ET, equalizing pressure, unless overgrown tubal tonsils squeeze it closed.

Last Drainage Stops: The Palatine and Lingual Tonsils
The Palatine Tonsils are the big boys we can see. Can’t see the Lingual Tonsils as they are embedded in the dorsum of the tongue. Figure 3 shows something very wrong with the Palatine Tonsils. Picture of the Kissing Tonsils shows something very wrong with the airway and is the reason the Pediatric guidelines for childhood Obstructive Sleep Apnea recommend Tonsillectomy as the FIRST line of defense.
This despite these lymphatic structures being essential for a lifetime of immune system function.
This despite multiple studies showing the airflow improvement is only temporary unless the child learns proper breathing behavior.
This despite multiple studies showing kids who had T&A surgery frequently grow up to be sicker adults than those who didn’t.
Ear infections are the most common reason for pediatric visits in this country, with 30 million doctor visits per year. Half of all pediatric antibiotics prescribed are for Otitis Media. The annual cost of treatment estimated at more than Two Billion Dollars. This is a pandemic plagued by ineffective symptomatic treatment that does not address the CAUSE.
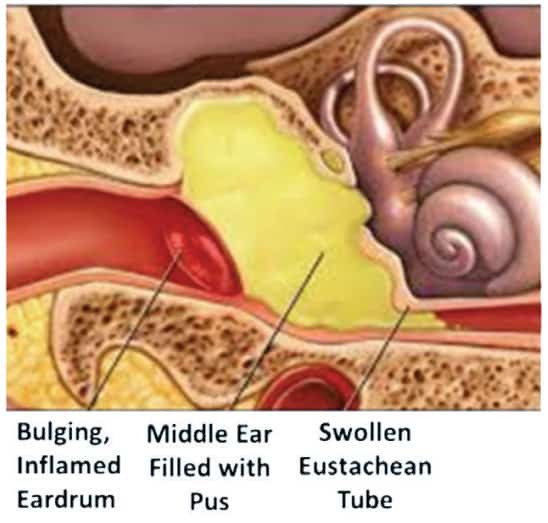
The middle ear is connected to the upper respiratory tract by a tiny channel known as the Eustachian Tube (ET). Germs growing in the nose or sinus can climb up the ET and enter the middle ear to start growing (Figure 4). This is more common in children than adults because these tubes are shorter and straighter than in adults.
Why do these structures get infected so often in so many modern humans? What could contribute to this being such a hugely prevalent and expensive public health issue? The reason for overprescribed antibiotics and tissue mutilation? Could it be related to dysfunctional breathing involving problems with structure, function, and behavior, beginning at or before birth?
Could it have something to do with a cascade of events caused by improper development of the Cranio Facial Respiratory Complex?
You may be like me, having forgotten about Tubal Tonsils. We had no way to connect middle ear infections to mouth breathing, much less breastfeeding and early childhood nutrition. You may be curious what dentists can do about this problem. I’d love to tell you, but I’m out of space in this essay. Stay tuned…
Adenoids and tonsils play a role in basic facial growth and development. Read about their connection to malocclusion here: https://dentalsleeppractice.com/effects-enlarged-adenoids-developing-malocclusion/.



