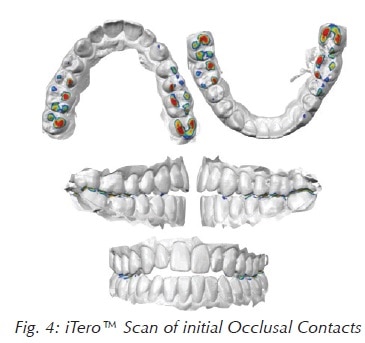
Women speak in code and men are in denial – I guess that John Gray explains that better in his bestselling book, Men are from Mars, Women are from Venus. So the next time a woman comes in complaining of clicking, painful temporomandibular joints, headaches, jaw, back and neck pain – you need to dig deeper. For instance, cues from the medical history, such as reflux, fatigue, difficulty concentrating and insomnia, are indicative of a sleep disorder. Cone-beam (CBCT) imagery (Fig. 1) will show patient and doctor the airway in 3 dimensions and help evaluate the role of the nose, tongue and soft palate as well as the tonsils and adenoids. Sleep testing provides a definitive diagnosis and is the current gold standard. By now, many of us understand the connection between temporomandibular disorders and sleep apnea. Plenty of peer-reviewed articles have shown this connection. 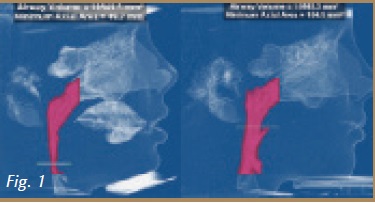 However, there is a still a major informational gap and patients are not aware of this connection. Often times, patients come to us after they have attempted to resolve their headaches with multiple physicians, medications and even other dentists, to no avail. With the cases presented in this article, Dr. Gelb and Dr. Ataii plan to show you the correlation of the symptoms reported by patients and how proper identification and treatment of a sleep disorder stabilized the patient.
However, there is a still a major informational gap and patients are not aware of this connection. Often times, patients come to us after they have attempted to resolve their headaches with multiple physicians, medications and even other dentists, to no avail. With the cases presented in this article, Dr. Gelb and Dr. Ataii plan to show you the correlation of the symptoms reported by patients and how proper identification and treatment of a sleep disorder stabilized the patient.
 Patient Bryan by Dr. Ataii
Patient Bryan by Dr. Ataii
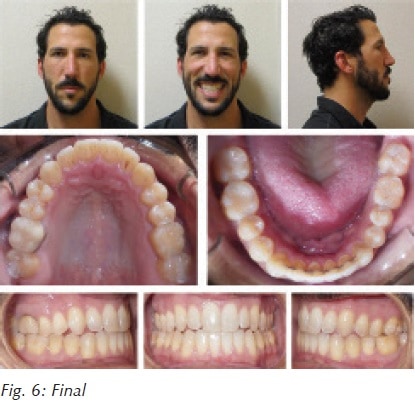
Patient Bryan (Fig. 2) was seen after having a long history of TMJ pain and multiple doctors refusing treatment due to the discrepancy of dental arch, open bite, and possible need for a surgical approach of Class III malocclusion and soft tissue pharyngeal involvement. Upon comprehensive examination, patient stated he did not want to have any wire bracket treatment, and had been on upper and lower expanders and myofunctional treatments from childhood. However, the patient did want to have a cosmetic solution for the anterior open bite and to have a better smile line.
 Treatment options included splint therapy combined with Invisalign® Clear Aligner treatment. Given his various signs and symptoms, he was judged to be high-risk for obstructive sleep apnea; an evaluation of the airway and a sleep study were recommended.
Treatment options included splint therapy combined with Invisalign® Clear Aligner treatment. Given his various signs and symptoms, he was judged to be high-risk for obstructive sleep apnea; an evaluation of the airway and a sleep study were recommended.
 Treatment
Treatment
Phase 1 addressed patient’s immediate pain with a CR (centric relation) splint therapy for six to eight weeks. In the interim, patient was screened and prescribed a sleep study thru Ez Sleep Home Testing System™ due to reported symptoms of fatigue, spouse complaining of snoring, and gasping for air during sleep, as well as visible indications of a large tongue and Class IV Mallampati. Sleep testing results indicated patient with mild obstructive sleep apnea (OSA) (Fig. 3), however, patient’s bite needed to also be put in proper occlusion, since patient only had 4-6 contact point of occlusion (Fig. 4). Due to patient refusal of bracket and wires, clear aligner treatment was suggested using the Invisalign® treatment system. Patient’s physician was also contacted and the patient’s sleep study results were shared with his primary care provider. An FDA-cleared oral sleep appliance known as the ASA (aligner sleep appliance™) (Fig. 5A) was chosen to be worn at night during sleep while still in treatment with Invisalign.

 Patient Nancy
Patient Nancy
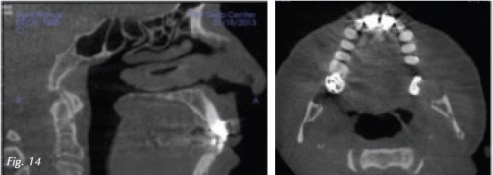
Patient Nancy (Fig. 7) wakes up with a headache every morning possibly related to taking out her partial at night. She also has numbness in her face and head as well as her gums, teeth and skull. Shoulder pain radiates into the occipital region. Cervical and masticatory muscles were exquisitely tender to palpation. There was pain in both posterior joint spaces when compressed through the external auditory meatus. On joint auscultation, we found coarse crepitus on terminal closure. The mandible was displaced by 1 mm to the right. Interincisal opening was normal at 42.5 mm. Initial cues pointed to a TMJ and musculoskeletal diagnosis. CBCT (Fig. 8) shows reduced joint space bilaterally, moderate to severe osteoarthritic changes in the left mandibular condyle with an anterior osteophyte. Airway space is somewhat decreased in axial and sagittal views (Figs. 9 and 10). A lower modified Gelb mandibular repositioning appliance was inserted for daytime wear (Fig. 11) and a Farrar anti retrusion appliance was inserted for use during sleep. Symptoms slowly subsided and 4 years later follow up photos and CBCT were taken (Fig. 12). The new intercuspal position was still maintained by an appliance due to limited finances, living in Virginia and the ill health of her husband. Pre and post condyle images (Fig. 13) and sagittal and axial airway images (Fig. 14) give us insight into how and why the eyes, skin and face look more vital and glowing. Sleep testing is standard practice in my protocol with an efficacy study at maximum medical improvement 3-6 months later. Physiological testing such as heart rate variability can also be used to assess autonomic and cardiovascular health. Endothelial dysfunction is also a physiologic metric and a major risk factor for cardiovascular disease.






 15 years ago dentists were claiming seemingly incredible results from repositioning therapy which can now be attributed to increasing oxygen saturation and decreasing intermittent hypoxia with follow up sleep testing. Sleep fragmentation or disturbed sleep is also improved as the patient spends more time in stage 3 restorative and REM sleep. This is verified by either overnight sleep study (PSG) or unattended home sleep study.
15 years ago dentists were claiming seemingly incredible results from repositioning therapy which can now be attributed to increasing oxygen saturation and decreasing intermittent hypoxia with follow up sleep testing. Sleep fragmentation or disturbed sleep is also improved as the patient spends more time in stage 3 restorative and REM sleep. This is verified by either overnight sleep study (PSG) or unattended home sleep study.
An even more dramatic example of AirwayCentric® TMJ protocol is seen in Ellen’s case. She is a 56 year old woman who presented with left TMJ locking, clicking and popping (Fig. 15). Left jaw pain radiates into the left ear and maxillary sinus. A severe aching headache starts in the left eye, ear and sinus and radiates into the jaw and mental nerve region. Nausea, vomiting, phono- and photo-fobia are denied. Clicking had occurred for 15 years, exacerbated in the last 3 years. Clinical exam revealed exquisite left cervical and masticatory pain as well as severe pain and compression in the left lateral TMJ capsule and the posterior joint space.
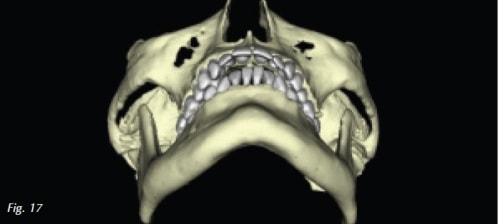
 Joint auscultation produced a late closing click in the left temporomandibular joint. The mandible is displaced to the left by 1.5 mm with interincisal opening of 48.5 mm.Past medical history includes depression, insomnia, sinus infections/congestion, reflux and fatigue.Tongue is level 2, Mallampati is class IV, with an elongated uvula. CBCT reveals mild osteoarthritic changes in the left mandibular condyle with decreased joint space bilaterally (Fig. 16). Overjet and mandibular retrognathia were extreme although the airway was not compromised (Fig 17).
Joint auscultation produced a late closing click in the left temporomandibular joint. The mandible is displaced to the left by 1.5 mm with interincisal opening of 48.5 mm.Past medical history includes depression, insomnia, sinus infections/congestion, reflux and fatigue.Tongue is level 2, Mallampati is class IV, with an elongated uvula. CBCT reveals mild osteoarthritic changes in the left mandibular condyle with decreased joint space bilaterally (Fig. 16). Overjet and mandibular retrognathia were extreme although the airway was not compromised (Fig 17).
Upper and lower repositioning appliances were inserted (Fig. 18). The ramp on the Farrar appliance was modified to prevent the mandible from retruding in the supine position (Fig. 19). Today an unattended sleep study would be performed to diagnose a breathing related sleep disorder and repeated once symptoms were improved.

Facial photos show us changes that are only possible with a profound decrease in systemic inflammation, reduced intermittent hypoxia and improved sleep architecture (Figs. 20-23). An AirwayCentric® orthodontist in NYC treated this case non surgically with unique orthodontic therapy. Orthognathic surgery is an alternative treatment plan.
Diagnostic cues from the medical history, facial analysis, and CBCT often indicate sleep studies should be included in the diagnostic process.

Conclusion
Next time you have a patient complaining of headaches or any sign and symptom of TMD/TMJ, prescribe a sleep study using the Ez Sleep System™ confirming sleep apnea. Note that it is not uncommon for patients to be unaware of the sleep condition they might be suffering from. And, given the high prevalence of TMD in patients who suffer from sleep apnea, addressing the compromised airway will generally lead to happier and more stable patients.
Many dentists believe orthodontic techniques are effective methods to expand the maxilla and mandible to increase intraoral volume, make room for the tongue, and reduce sleep disordered breathing. To achieve the best results with temporomandibular disorders consider maintaining the mandible in a neutral or protrusive position at night to decompress the temporomandibular joints, and increase oxygen saturation while improving restorative and rem sleep.
Best practices require a follow-up sleep test with the recommended oral appliance to ensure control of sleep related breathing events (Fig 5B).