Table of Contents
Background
The importance of incorporating vertical dimension (VDO) into jaw positioning for treatment of OSA with oral appliances has been largely overlooked in the Dental Sleep Medicine community. Although some commercial bite registration products include a vertical component, there is little critical evidence to support their use. Additionally, early work by Peter Cistulli and his group showed that adding VDO did not improve outcomes with oral appliances. In that study the patients’ existing dorsal fin appliances were opened from a starting 4mm of inter-incisal distance to 14mm.1
More recent clinical evidence from our group, however, has demonstrated that selected patients may benefit from increasing VDO when adding smaller, calculated amounts.Based on clinical experience using this approach, we have had considerable success improving patient comfort and outcomes. I have been asked to share our experiences along these lines with the readers of Dental Sleep Practice magazine.
In our practice we routinely deploy a calculated amount of vertical and protrusive positioning with each case using the Apnea Guard® system. This system is easy to use and was developed based on our work with OA titration and follow-up using Home Sleep Testing. The Apnea Guard trial oral appliance was designed to primarily serve three functions: 1) Provide determination of the correct jaw position for any design of custom oral appliance 2) Enable the dentist or sleep laboratory to provide immediate treatment for patients 3) Reduce the time and the number of appointments necessary to reach adequate treatment.
 Based on our clinical trial demonstrating equivalency between AG and custom appliances2, some of our sleep labs have begun fitting and using the AG to assess a patient’s response to OAT during their overnight PSG. The sleep labs are then able to offer their patients more treatment options going forward, and perhaps even better is that the patient has immediate treatment for their OSA by using the AG out the door, and while waiting for their custom appliance! Other labs that do more home sleep testing are also helping dentists to identify good candidates for OAT prior to the purchase of a custom device. Besides this being good medical practice, insurance carriers in our region are very interested in this approach since it saves healthcare dollars by identifying responders to OAT ahead of making larger expeditures.
Based on our clinical trial demonstrating equivalency between AG and custom appliances2, some of our sleep labs have begun fitting and using the AG to assess a patient’s response to OAT during their overnight PSG. The sleep labs are then able to offer their patients more treatment options going forward, and perhaps even better is that the patient has immediate treatment for their OSA by using the AG out the door, and while waiting for their custom appliance! Other labs that do more home sleep testing are also helping dentists to identify good candidates for OAT prior to the purchase of a custom device. Besides this being good medical practice, insurance carriers in our region are very interested in this approach since it saves healthcare dollars by identifying responders to OAT ahead of making larger expeditures.
Our Approach
After the patient has been consulted and examined, several design options of the custom oral appliances are demonstrated. We invite the patient to be involved in this process and ask questions. Based on clinical judgment, the sleep study data, and the patient’s oral presentation or preferences, a design is chosen. Following the usual impressions the Apnea Guard protocols are implemented, requiring approximately 10 minutes to complete.
Vertical tray height selection will depend on gender and tongue size (figure 1). Females start with less VDO (a low size tray) and Males start with a medium tray height. Then the tray height is increased by one size depending on whether obvious tongue scalloping is present (figure 2). Three simple steps are followed to center the patient’s teeth into the AG expanding trays that are filled with the recommended PVS putty.
Protrusive positioning is calculated to 70% using the AG slider (figure 3) and these settings are provided to the dental laboratory for custom appliance fabrication.
 Protrusive is reduced by 1mm for patients leaving with the AG as immediate treatment and they are given instruction to advance forward that same one millimeter before their next appointment. (The complete AG technique can be viewed at http://www.advancedbrain monitoring.com/apnea-guard/).
Protrusive is reduced by 1mm for patients leaving with the AG as immediate treatment and they are given instruction to advance forward that same one millimeter before their next appointment. (The complete AG technique can be viewed at http://www.advancedbrain monitoring.com/apnea-guard/).The patients often return with their jaws adequately conditioned and adapted to advancement, and are very happy to move to their custom appliance! For for those who will be tested by PSG or HST, the AG is left at 70% for that night of testing. Sleep technologists are instructed to titrate the patient forward on the night of PSG based on another protocol when response is not adequate. So far, we have rarely had to decrease protrusion when the AG protocol is followed, although before AG’s arrival I had plenty of concern about advancing patient immediately to the full predicted protrusion.
Time Savings in Reaching Optimal Outcomes
When the correct combination of protrusion and vertical dimension is deployed at the outset of treatment we have seen a considerable reduction in the number of follow-up appointments needed for further calibration. In order to determine how much time was saved using AG, we performed a retrospective survey of charts prior to the time we began using the AG system, and looked at the number of appointments needed to reach an endpoint of calibration with acceptable outcome for the AHI. Then prospectively, we made the same observations using the Apnea Guard, comparing the two groups for differences with regard to number of appointments required to reach a treatment endpoint, costs, and outcomes.
Using Apnea Guard protocols we were able to improve our rate of successful outcomes from 79% to 93%. The elapsed time from the start of therapy until a successful outcome is achieved has been reduced from an average of 177 to 33 days. The reduction in office visits/chair time contributed to a savings of $455 per patient which more than covers the $60 cost for the Apnea Guard.
How Does VDO Improve Outcomes?
Theoretically, adding VDO may improve upper airway dynamics by one or two routes: 1) By putting the hyoid sling musculature under additional tension, primarily via the stylohyoid and styloglossus muscles, or 2) By increasing a phenomenal known as tracheal tug. My assumptions are based on the dynamic interaction of the infra and supra hyoid muscles and observation on lateral imaging that demonstrates a “smoothing” of the pharyngeal mucosal outline. Whatever the mechanism, we have found in clinical practice that VDO acts as a surrogate to further protrusion in bringing down the supine AHI.
One surprising effect that we have seen in clinical practice: is that adding VDO consistently makes further protrusion more comfortable for the patient, and often mitigates muscle/joint soreness (I will let the gurus of the TMJ world figure this one out).
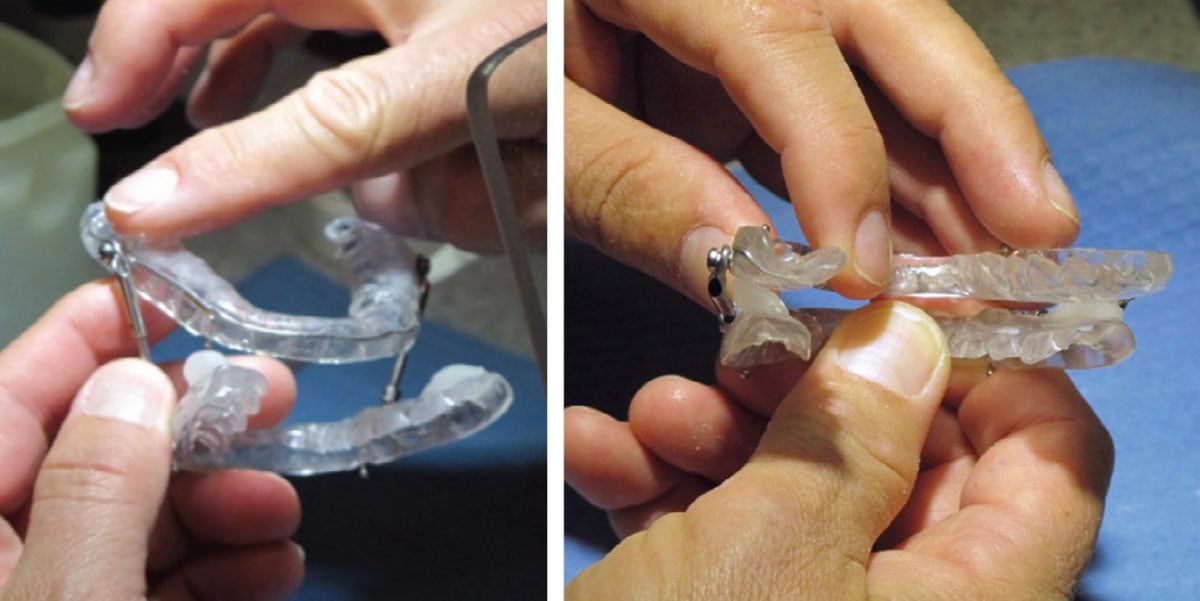
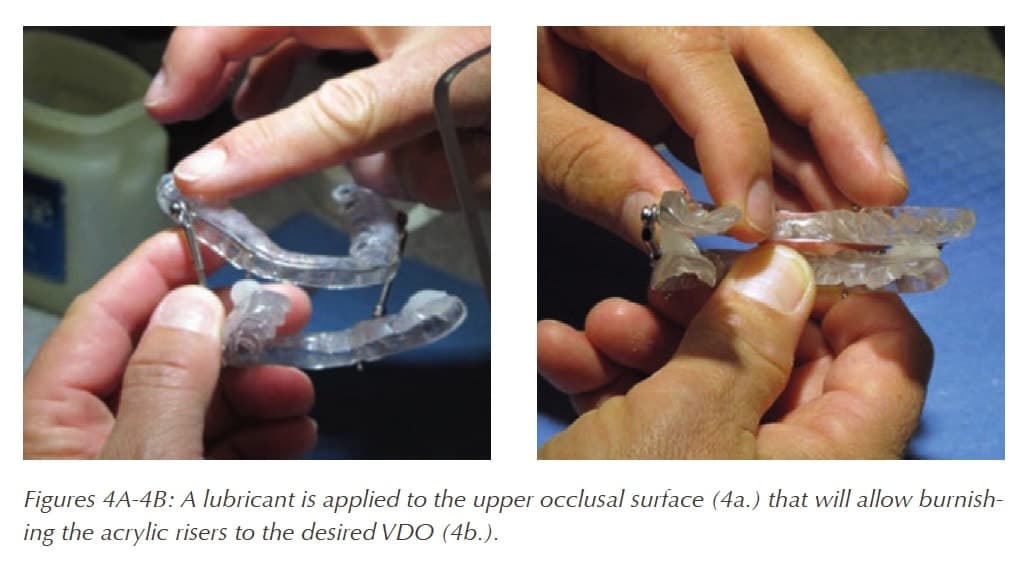
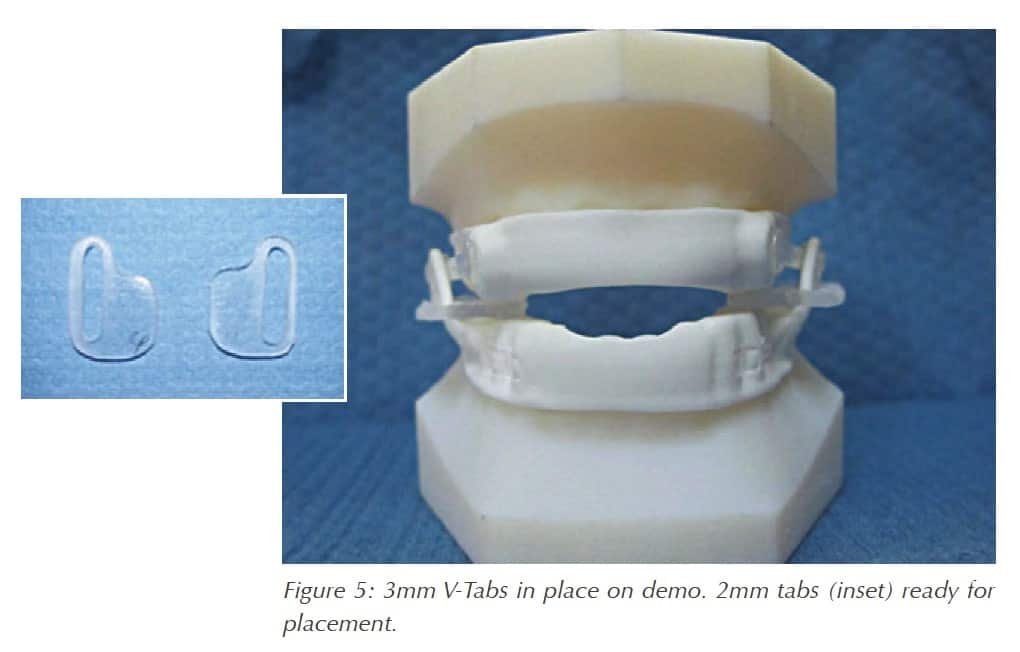
Adding VDO is easily accomplished at the chair with a lab handpiece and cold cure acrylic (figure 4). One exception is the Narval appliance, where VDO cannot be increased without the use of a novel vertical tab (figure 5). These V-tabs come in 1, 2 and 3mm thicknesses and are designed to fit over the fin on the lower component tray. You can contact your Narval lab to obtain the tabs and full application of their use.
I hope that the reader may gain some insight here to the use of VDO in their future cases. I am confident that more scientifically based guidelines for calibration of Oral Appliances will bring greater success and satisfaction among our colleagues and of course, our patients!