Editor’s intro: Implementing digital workflows for oral appliance therapy helps clinicians to grow their practices, enjoy their work more, and has made niches, such as dental sleep medicine, more accessible to the dental consumer.
by Tarun Agarwal, DDS, PA
You may have heard that the ‘golden age’ of dentistry has passed us by. With the strengthening economic clout of dental benefit companies, competitive pressures of well-funded ‘corporate’ dental practices, and the financial handcuffs of student and practice debt – it is easy to fall into the trap of believing this thought. I’m here to say that dentistry has never held more promise. Technology has transformed our personal lives for the better and actually gives the solo dental practice more than a fighting chance. Never before have general dentists been able to expand their scope of care than what our profession has witnessed in the past decade. Today, we enjoy the convenience of digital impressions and single visit chairside restorative dentistry, digital 3D radiology and its diagnostic capabilities, digitizing implant dentistry leading to fewer visits and better outcomes, and the virtual planning and execution of orthodontic treatment with clear aligners.
 When I graduated dental school in 1999, I never believed that I would be able to accomplish the scope of care and predictability we are now achieving. Each innovation has allowed me to grow my practice, enjoy dentistry more, and more importantly, has made these procedures more accessible to the dental consumer. To say it boldly, I wouldn’t be doing these procedures without the help of technology.
When I graduated dental school in 1999, I never believed that I would be able to accomplish the scope of care and predictability we are now achieving. Each innovation has allowed me to grow my practice, enjoy dentistry more, and more importantly, has made these procedures more accessible to the dental consumer. To say it boldly, I wouldn’t be doing these procedures without the help of technology.
Table of Contents
So, what does all this have to do with Dental Sleep Medicine?
Largely, dental sleep medicine has been forgotten and left behind when it comes to technological innovations. This has made the practice of obstructive sleep apnea (OSA) therapy more of an ‘art’ than science. Will appliance therapy work? At what position will we achieve the best results? When does one have a follow up sleep study performed? What happens if TMD or bite complications occur? These questions and uncertainties are keeping dental sleep medicine from gaining the national prominence it deserves and patients desperately need! In fact, it’s these concerns that kept me from fully embracing dental sleep medicine in my practice until several years ago.
Luckily for my practice and patients, technology has come around to provide solutions that makes dental sleep medicine more predictable and way more fun!
Technology entering dental sleep medicine is a positive development and will impact oral appliance therapy in the three most important categories – patients, dentists, and team members. For patients, technology will allow dental practices to create awareness by making it easier to have a conversation about OSA and allow patients to better understand their condition through the use of visual aids. For dentists, technology will make appliance therapy more predictable and require fewer visits – making adding OSA therapy less disruptive to the traditional general practice. For team members, technology will make it easier for auxiliaries to better support the doctor and patients in the overall workflow of dental sleep medicine.
A fully digital solution for appliance therapy
Let’s get down to business now. I would like to share with you how today’s technology has transformed how our practice provides therapy for OSA.
I’ll begin by sharing our fundamental workflow and then how technology fits into each of these steps.
- Awareness
- Diagnosis
- Treatment
Awareness.
The saying goes that you can’t treat what your patients don’t see. You must help them become aware of their health problems. For most dentists and team members, it has proven difficult to bring up a conversation about sleep apnea.
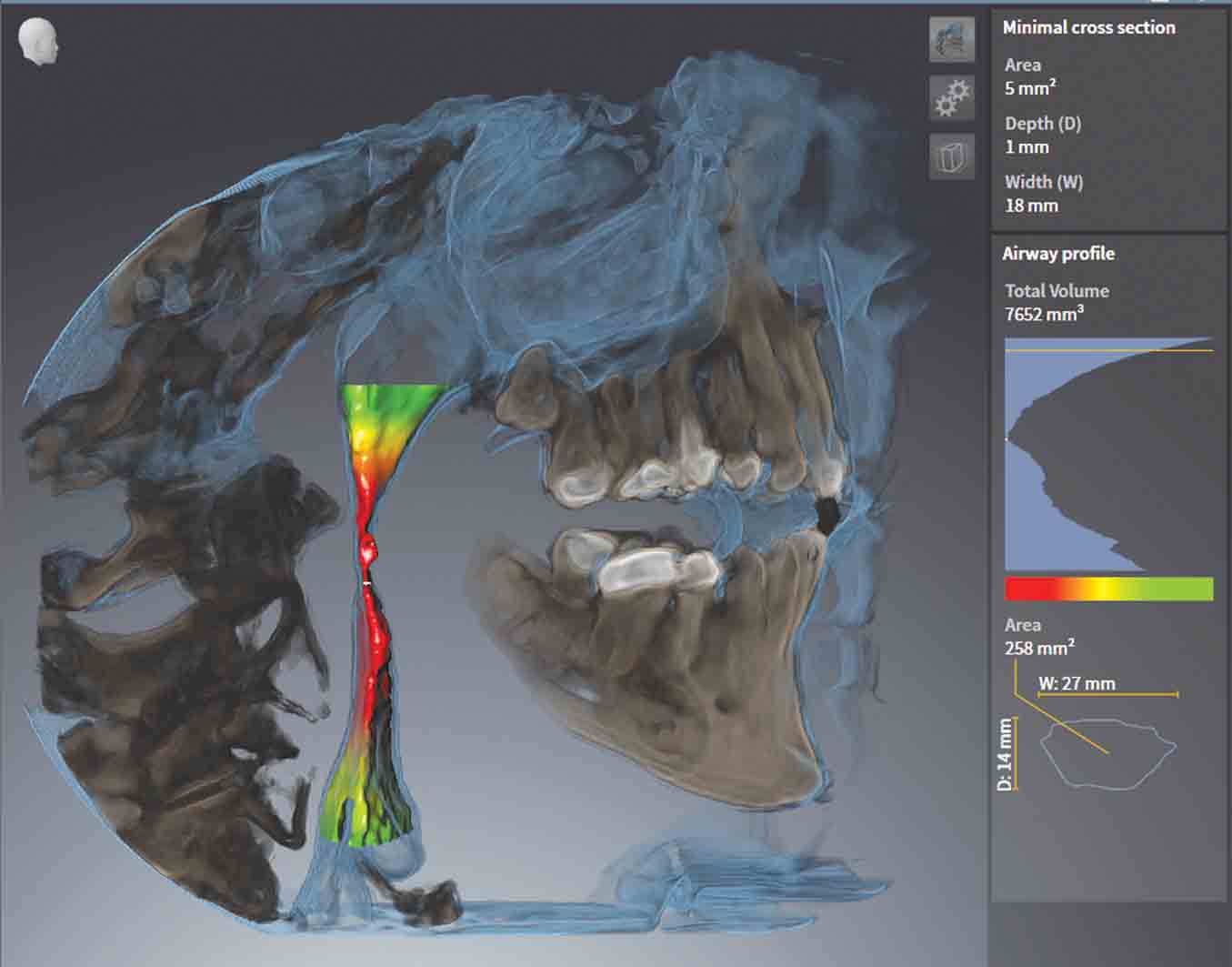
When we started using CBCT airway segmentation as a non-diagnostic tool to show patients what their airway looked like, and presented the link between medical conditions and sleep apnea, something very interesting happened. Patients actually started asking us questions and leading the conversations.
It is my opinion that best practice would be to provide each patient – not just those who we think have sleep apnea – with a 3D colored airway segmentation. The reason being is that it is often the spouse of a patient who has symptoms of sleep apnea. Our goal should be to raise overall awareness of the gravity of OSA.
Diagnosis.
Once you have created awareness and conversation the next step is to encourage the patient to take a test to ‘rule out’ the presence of OSA. This testing can be done using a PSG (polysomnogram) at a sleep lab or at home using an HSAT (Home Sleep Apnea Test).
It is important for me to remind readers that the diagnosis of sleep apnea CANNOT be done by a dentist and that I believe it is best practice to have every HSAT scored by a sleep tech and read by a board-certified sleep physician. Circumventing the physician community is not in the best interest of the patient.
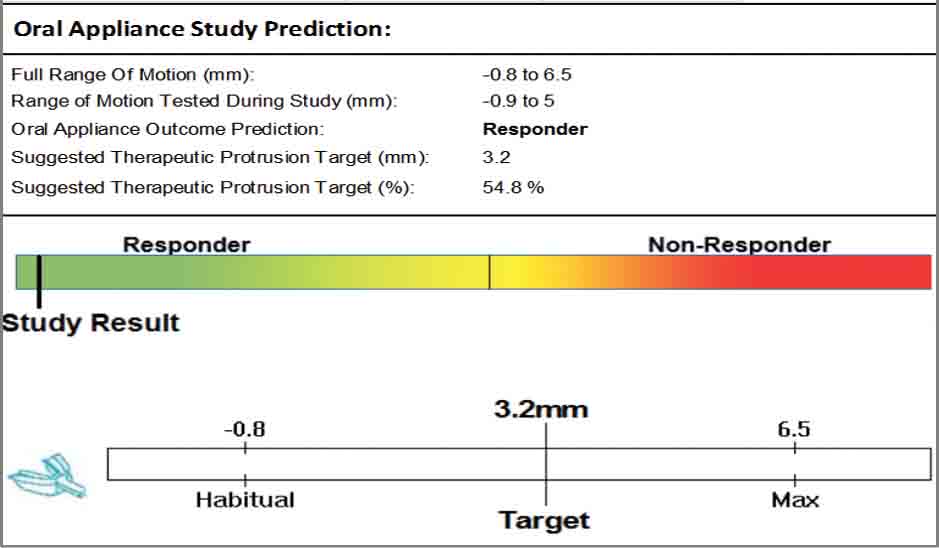
While the HSAT is not a new technology, what is different is the ability for a device (MATRx plus, Zephyr Sleep Technologies Calgary, Canada) to be able to assist in the diagnosis and predict whether or not the patient is a candidate for oral appliance therapy. It takes a step further by determining at what protrusive position the patient will achieve maximum results.
The MATRx plus accomplishes this by fitting the patient with a sliding dental tray that is controlled by a micromotor. This motor and attached tray adjust throughout the night in reaction to the measured oxygen response by the associated HSAT device. A patient is designated a responder if their oxygen desaturation index (ODI ) is below 10.
The included Type 3 HSAT enables diagnosis by a physician. Adding the jaw positioning element introduces a new level of technology: Theragnostics. This reflects a combination of diagnosis with immediate determination of potential therapy.
Implementing theragnostics into our sleep apnea workflow has given me, the prescribing physician, and the patient confidence that oral appliance therapy is a good decision. We now know what our optimal end point is and can adjust our starting point to achieve treatment in less time. Because we know what the target position is, we avoid over-protrusion, minimizing disruption to the jaw joint and jaw muscles. Another benefit from this new piece of technology is that it has reduced our chair time and number of patient visits.

Treatment.
So far, we have a patient who has OSA (with proper supporting medical physician diagnosis), the MATRx plus testing has determined that the patient is a responder for oral appliance therapy and at what protrusive position to achieve optimal results.
To fabricate an appliance we need upper and lower impressions and a treatment bite. Traditionally this has been accomplished via PVS impressions. Today all of this is accomplished digitally. In our office the models are captured using CEREC Omnicam (Dentsply Sirona) and the MATRx plus theragnostic bite is captured via 3D CBCT imaging. 3D CBCT imaging allows the clinician to evaluate the joints and the upper airway (nasal septum, nasal turbinates, and sinuses), any of which can impact overall effectiveness of oral appliances.


So, what is the benefit of fabricating the appliance digitally?

To fully appreciate the benefits of the digital workflow it is best to realize the inherent flaws of the analog workflow as it relates to the impression and bite.
Capturing full arch impressions for appliances is not easy, yet critical. Most of us are using stock trays that don’t always extend far enough distally – leading to an inaccurate capture of the distal tooth. Another common result found on stone models in the lab are pulls on the linguals – which are then ‘guestimate’ corrected at the lab by scraping the model. These points are important because it is the impression that determines the fit of the appliance. Digital impressions allow you to completely and accurately capture all surfaces without distortions.
The bite is also a culprit in the analog method. It is easy for the patient to deviate when capturing the protrusive bite record. This is often overlooked in the practice while the patient is still present and not noticed until mounted by the laboratory. Appliances made with deviated bites and/or improper mountings can be causes of tooth shifting, bite changes, and/or TMD issues. Correction at this point means the patient has to be brought back into the practice. Capturing the bite digitally allows immediate visualization and verification. The digital workflow outlined here greatly simplifies the task of proper 3D bite registration.
You can see there are significant benefits to having a fully digital workflow. But we aren’t done yet! There are also benefits to having a digitally fabricated appliance (OPTISLEEP – SICAT). In my experience, there are two main complaints from patients about oral appliances – bulk and bacteria. Both of these are directly related to the analog fabrication method.
Analog sleep appliances are typically made using powder/liquid acrylic. These are inherently weaker and require greater bulk and/or metal reinforcement for strength. These analog appliances are also more porous and attract more bacteria – leading to early discoloration and a bad odor. Digitally fabricated appliances are slimmer and more comfortable to wear, they are stronger and last longer for the patients, and are healthier due to the significant decrease in bacteria accumulation.
I am hopeful and confident that you can see that a digital workflow for oral appliance therapy is a positive and gigantic leap forward for the field of dental sleep medicine. It will give more dentists the confidence to step into this growing field and provide quality treatment. Dentistry’s contribution to a population health problem will stand out and more people will seek therapy.




