Dr. Paulo Soares talks about the integration of dentistry, orthodontics, and myofunctional therapy to help children with sleep-breathing disorders and craniofacial development.
 by Paulo Soares, DDS, MSD (Orthodontics and Dentofacial Orthopedics)
by Paulo Soares, DDS, MSD (Orthodontics and Dentofacial Orthopedics)
Introduction
It is hard to turn a corner these days without hearing about mouth breathing and its effects on overall health. Aided by an increased exposure in pop culture and practitioner knowledge, patient awareness and demand for treatment continues to grow at a rapid pace. In response to this demand, practitioners have concluded that early treatment and prevention is best, but they continue to search for the best ways to help their patients.
While physicians have traditionally treated breathing disorders, dentists and orthodontists are increasingly being called upon to assist in these efforts. Given the close relationship between the upper airway and the oral cavity, dentists play a crucial role in the treatment of breathing disorders,1 which have also been associated with dental conditions, such as caries and periodontal disease.2

Historical Background
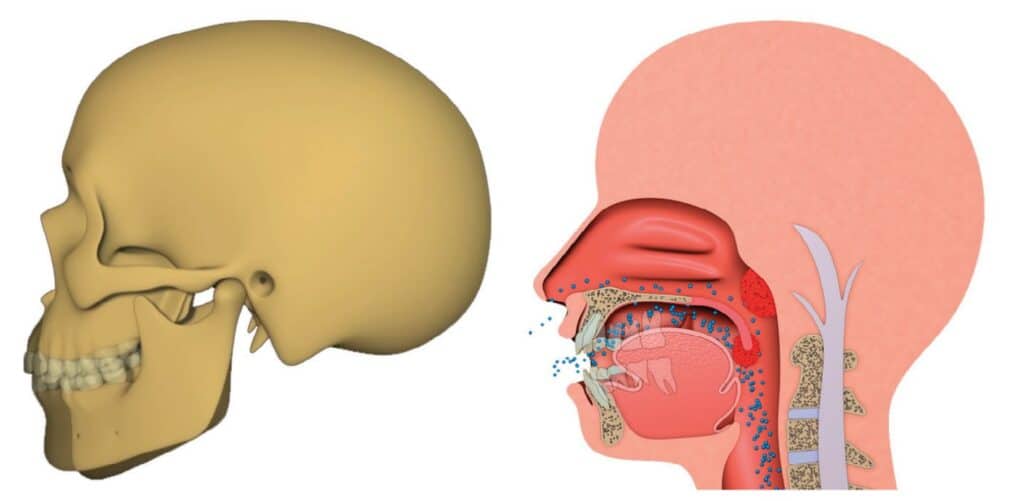
Optimum breathing patterns involve the mouth being closed, lips sealed, tongue resting in the palate and gentle nasal breathing. In his 1907 textbook, the father of orthodontics Dr. Edward Angle stated, “Of all the various causes of malocclusion, mouth breathing is the most potent, constant and varied in its results.”3 Angle understood that mouth breathing changed the function of the oral muscles (collectively known as myofunctional disorders), which changed the forces imparted on the teeth and jaws, leading to malocclusion.
In response to this idea, one of Angle’s students, Dr. Alfred Rogers, began implementing a series of oral exercises in the 1930’s to correct this phenomenon, which was the birth of myofunctional therapy in orthodontics.4 As orthodontics became more focused on mechanics over biology, new bracket technology and better ways of straightening teeth dominated the discourse over the 20th century.5
Discovery of Sleep Disordered Breathing in Children
Thanks to a series of discoveries in sleep medicine which occurred in the latter half of the 20th century, scientists began to understand that it is not just adults who suffer from Obstructive Sleep Apnea (OSA), but a new spectrum of breathing disorders called Sleep Disordered Breathing (SDB) became understood to affect children as well.
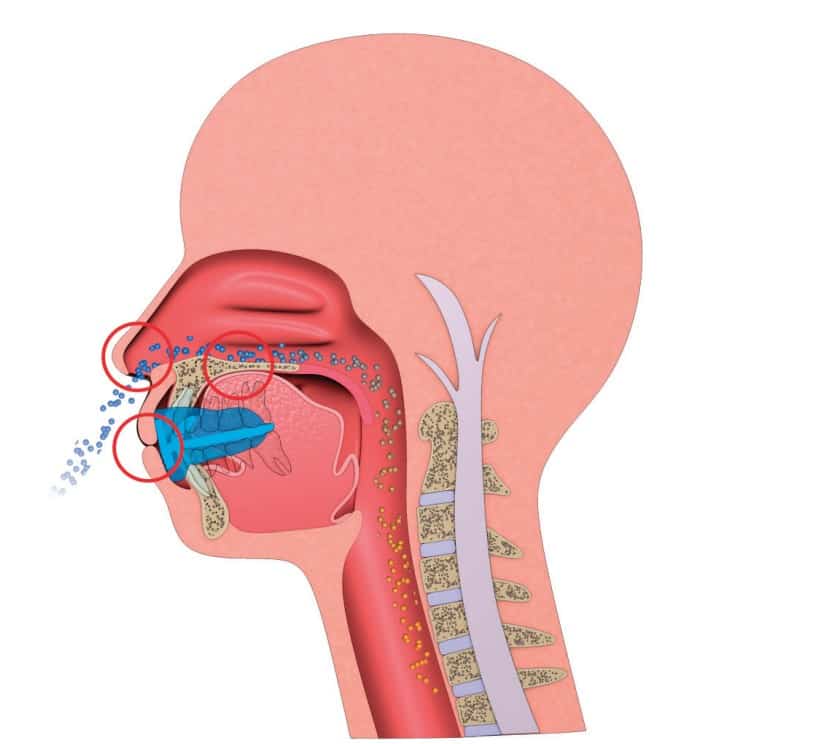
SDB includes (in order of severity) mouth breathing, snoring, Upper Airway Resistance Syndrome (UARS) and OSA6 and can affect patients from the first days of life. SDB is known to be linked to numerous mental and physical conditions in both children and adults. As with most medical conditions, prevention is better than cure, and this is what the father of sleep medicine Dr. Christian Guilleminault suggested when he advocated for early treatment and stated, “the only valid treatment goal is restoration of nasal breathing.”7
If we reflect on the cascade of events that cause these issues, we understand that mouth breathing precipitates poor oral habits, which alter the patient’s growth and development and finally result in malocclusion.
Integration of Dentistry, Orthodontics, and Myofunctional Therapy
The research has led us to understand that there is an interplay of nasal obstructions or restrictions (e.g., allergic rhinitis or adenotonsillar hypertrophy), poor craniofacial development and myofunctional disorders in the development of SDB, especially in non-obese patients. We also understand the cumulative damage imparted by SDB, which means the issue must be treated as soon as it is detected.8
The role of poor craniofacial development and myofunctional disorders in the development of SDB has led to the inclusion of dentistry, orthodontics, and myofunctional therapy in the treatment of breathing disorders (in cooperation with otolaryngology). In fact, the World Dental Federation (FDI) published a policy statement in 2018 urging dentists to be actively involved in treatment, more specifically “prevention of late-onset forms” of SDB.9
Challenges in Current Treatments
Unfortunately, the treatments proposed to address these breathing disorders and the restoration of nasal breathing have caused dissipation of enthusiasm among practitioners and patients. Positive Airway Pressure (PAP) therapy can be used, but it has been found to have adverse effects on facial development, potentially worsening breathing disorders in the long term.10
Orthodontic techniques have also been proposed, but their outcomes are unpredictable, unstable and they may exacerbate myofunctional disorders.11 Surgical interventions are often a last resort due to their complexity, cost, and potential side effects, while research clearly shows that surgery is not the only answer.12,13 Parents and practitioners alike are also hesitant to explore surgical options unless absolutely necessary.
Resurgence of Myofunctional Therapy
In recent years, myofunctional therapy has experienced a resurgence as a non-invasive approach to correcting myofunctional disorders, improving SDB and promoting healthy craniofacial growth and development in patients. While the concept is sound, traditional myofunctional therapy suffers from issues of unpredictability, complexity, and lengthy treatment duration. This was the reason it originally fell out of favour, and unfortunately the resurgence has done very little in the way of redesign or updates to this excellent intervention.
Poor patient compliance combined with the lack of a globally recognized and standardized program have hindered its widespread success. To address these challenges, a structured, simple, and cost-effective rehabilitation protocol is necessary to meet the growing demand for treatment. Since our understanding of early treatment has improved, the need to apply this intervention to very young children means that the need to correct these deficiencies is even greater. Even if the treatment is not applicable to 100% of patients, even a modest reduction in the disease burden would still be worthwhile.
The simplicity and child-friendly approach of the protocols make it enjoyable for children to participate in habit correction.

breathing and myofunctional disorders.
The Myofunctional Orthodontic Appliance Protocol
One potential solution that shows promise is the implementation of a myofunctional orthodontic appliance protocol. This approach involves the use of prefabricated myofunctional appliances as part of a simple and structured treatment plan. These appliances serve multiple functions, including promoting nasal breathing, developing dental arches, establishing correct habits, and aligning teeth. By combining non-invasive and cost-effective treatment methods, these appliances provide a way to correct poor habits associated with mouth breathing while improving orthodontic outcomes. Collaboration with medical practitioners is also integrated into the treatment protocols when necessary. Published studies have shown some potential for this technique, and as the openness of the profession to this novel approach improves, more high-quality studies are expected to arise.14
Sequential Stages of Treatment
The myofunctional orthodontic appliance protocol typically consists of administering 3-4 appliances sequentially to progressively rehabilitate the patient. If we reflect on the cascade of events that cause these issues, we understand that mouth breathing precipitates poor oral habits, which alter the patient’s growth and development and finally result in malocclusion.
In response, myofunctional orthodontic appliances address the problem in the order in which it occurs. The initial stage concentrates on correcting breathing and myofunctional disorders, as these habits form the basis of treatment. The second stage focuses on developing dental arches while continuing to address breathing and myofunctional issues. The final stages aim to retain the arch form, align teeth, and assess the stability of habit correction. Each stage corrects a certain problem and sets the foundation for the next condition to be corrected in the cascade.
Benefits of Myofunctional Orthodontic Treatment
The myofunctional orthodontic treatment protocol offers several advantages. The prefabricated nature of the appliances and their advanced features make treatment easy to learn and implement for practitioners. This allows for wider dissemination of the treatment to meet the demand for early intervention and prevention of mouth breathing and myofunctional disorders. Moreover, the simplicity and child-friendly approach of the protocols make it enjoyable for children to participate in habit correction. Accompanying digital and print resources further enhance the effectiveness of the treatment and improve compliance. Treatment delivery is a key part of the myofunctional orthodontic approach. Overall, the myofunctional orthodontic treatment protocol represents an exciting development in the fields of orthodontics, myofunctional therapy, and dental sleep medicine.
Conclusion
In conclusion, the treatment of pediatric sleep breathing disorders requires a comprehensive and proactive approach. The integration of dentistry, orthodontics, and myofunctional therapy has emerged as a vital part of addressing these issues. The myofunctional orthodontic appliance protocol offers a structured, simple, and cost-effective rehabilitation strategy that can be implemented on a large scale to meet the increasing demand for treatment. By focusing on early intervention and prevention, this protocol aims to restore nasal breathing, correct poor habits, and improve orthodontic outcomes in pediatric patients. While further research and refinement are needed, the myofunctional orthodontic approach holds great promise in bridging the gap in pediatric sleep breathing treatments and ensuring the long-term oral and overall health of children.
For more information on Myofunctional Orthodontics, visit www.myoresearch.com and start with the free online courses.
- Leibovitz et al. Pediatric sleep-disordered breathing: Role of the dentist. Quintessence Int. 2018;48(8): 639-645.
- Ballikaya et al. Oral health status of children with mouth breathing due to adenotonsillar hypertrophy. Int J Pediatr Otorhinolaryngol. 2018 Oct;113:11-15.
- Angle E.H. (1907) Treatment of malocclusion of the teeth: Angle’s System. S.S. White Manufacturing Co., Philadelphia.
- Rogers A. Evolution, development, and application of myofunctional therapy in orthodontics. Am J Orthod Oral Surg. 1939 Jan;25(1): 1-19.
- Ackerman J. Was the destiny of orthodontics written in the stars. Am J Orthod Dentofacial Orthop. 2015;147:290-2.
- Bonuck et al. Sleep-Disordered Breathing in a Population-Based Cohort: Behavioral Outcomes at 4 and 7 Years. Pediatrics. 2012 Apr; 129(4): e857–e865.
- Guilleminault et al. Sleep-Disordered Breathing, Orofacial Growth, and Prevention of Obstructive Sleep Apnea. Sleep Med Clin. 2019 Mar;14(1):13-20.
- Alison et al. Recent advances in paediatric sleep disordered breathing. Breathe 2022 18: 220151.
- World Dental Federation 2018. Dentistry and Sleep-Related Breathing Disorders. Viewed 14 June 2023. <https://www.fdiworlddental.org/dentistry-and-sleep-related-breathing-disorders>
- Roberts et al. Midfacial and Dental Changes Associated with Nasal Positive Airway Pressure in Children with Obstructive Sleep Apnea and Craniofacial Conditions. J Clin Sleep Med. 2016 Apr 15; 12(4): 469–475.
- Barbosa et al. Rapid maxillary expansion in pediatric patients with obstructive sleep apnea: an umbrella review. Braz. J. Otorhinolaryngol. 2023 Jun;89 (3): 494-502.
- Huang et al. Treatment Outcomes of Adenotonsillectomy for Children with Obstructive Sleep Apnea: A Prospective Longitudinal Study. Sleep. 2014 Jan 37: 71-76.
- Guilleminault et al. A prospective study on the surgical outcomes of children with sleep-disordered breathing. Sleep. 2004 Feb 1;27(1):95-100.
- Ferreira FG. Novel Approaches for Class II Malocclusion Treatment using Myofunctional Orthodontics Therapy: A Systematic Review. Int J Dentistry Oral Sci. 2017. 4(7), 503-507.


 Paulo Soares, DDS, MSD, is an orthodontist in Brazil. Dr. Soares graduated with his dental degree from the Universidade Federal de Sergipe, Brazil. He is a specialist in Orthodontics and Facial Orthopaedics with more than 15 years of experience in Myofunctional and Airway Orthodontics. Dr. Soares is a Myobrace Certified Provider and Educator. He is also a member of the Brazilian Dental Sleep Medicine Association (ABROS).
Paulo Soares, DDS, MSD, is an orthodontist in Brazil. Dr. Soares graduated with his dental degree from the Universidade Federal de Sergipe, Brazil. He is a specialist in Orthodontics and Facial Orthopaedics with more than 15 years of experience in Myofunctional and Airway Orthodontics. Dr. Soares is a Myobrace Certified Provider and Educator. He is also a member of the Brazilian Dental Sleep Medicine Association (ABROS).