 SomnoMed’s Medical Initiative Brings Dental Sleep Medicine Solutions to Prescribing Physicians to Treat More OSA Patients, More Effectively
SomnoMed’s Medical Initiative Brings Dental Sleep Medicine Solutions to Prescribing Physicians to Treat More OSA Patients, More Effectively
by Matthew Conlon, EVP of Sales & Marketing, SomnoMed North America
SomSummit ’22 co-chairs, Colleen Lance, MD, and David Rapoport, MD, insightfully noted: “Never before has the specialty of sleep medicine been at such a turning point, poised with innovation in several key arenas. As a field, we are redefining what sleep apnea is and how to better measure and treat it.”
SomnoMed North America recently held our second annual SomSummit ’22, in Scottsdale, AZ. We showed, by example, the power of physician-dentist collaborations as our Medical Initiative is intended to facilitate. We also highlighted the enormous opportunity to successfully treat more OSA patients in light of the astonishing statistics we see of undiagnosed, untreated OSA sufferers, and the growing recognition of PAP treatment shortcomings in effectiveness – and now, access.

SomSummit ’22 presented an opportunity to go even further. The focus wasn’t on Oral Appliance Therapy (OAT), and it wasn’t about SomnoMed products. Rather, it focused on vetting the value of all therapies, and the fundamental research that supports them in improving, and even defining, OSA treatment “success.” Topics included:
- The potentially waning value of AHI and myriad prospective future approaches to better define and measure successful treatment
- When and why to STOP likely-to-fail therapies based on “big data” statistics
- Patient endotyping and phenotyping as a means to predict the most successful treatments outcomes
- The potential to quickly triage patients from one failed or failing therapy to the next, and starting with patient choice as a likely factor in treatment success
- And of course, all too familiar reminders of the stubborn and startling OSA prevalence and treatment statistics that unify sleep health professionals of wildly diverse interests and expertise around a “North Star” urgency to Treat More OSA Patients, More Effectively.
It’s truly humbling to gain a fuller perspective of the entire universe of solutions in sleep disordered breathing. It’s also daunting to contemplate the work needed to make an impact, to move the needle, to address the gaps, and to ease the frictions that stand in the way of broader and more effective treatment of the persistently underestimated condition of OSA. The goal – the mission – for SomnoMed, however, is simple: to bring OAT and the Dental Sleep Medicine (DSM) experts who provide it into the primary OSA treatment ecosystem as a prominent, clinically accepted, and accessible therapy for OSA sufferers…among other therapies.

Over the past year, SomnoMed assembled Clinical Advisory Boards, composed of both sleep dentists and physicians, in each of our global regions. This year, we were delighted to follow the lead of our Clinical Advisory Board members and SomSummit ’22 co-chairs, Colleen Lance, MD, and David Rapoport, MD. In contrast to last year’s Summit, while DSM was expertly and prominently represented, DSM and OAT was but one specialty, one topic, interspersed and in relation to ALL current and future potential therapies and approaches to Treating More OSA Patients, More Effectively. The theme of SomSummit ’22 was “The Right Therapy for the Right Patient, at the Right Time.” As humbling – and daunting – as the challenge may be, the level and diversity of expertise, and the professional interest, courtesy, and admiration across all specialties, points toward an incredibly promising future for the field of DSM.

Sleep dentistry was superbly represented and fully engaged in the sleep ecosystem during SomSummit ’22, which was comprised of top key opinion leaders (KOLs) and practitioners in sleep medicine. A barometer of SomnoMed’s Medical Initiative, this confirms for us, the DSM community, that OAT has earned a respected position within that primary ecosystem. Now, we must continue to translate this strong position with the goal of enabling OAT as a standard of care.

The Sleep Ecosystem
The growth of DSM and OAT to where it stands today as a clinically viable option for the treatment of OSA is a credit, almost exclusively, to the profession itself: both top-down, through formal organization of advocacy, education, and credentialing, and bottom-up, dentist-by-dentist treating patient-by-patient. One-by-one, expert DSM providers have cultivated rare, trusted relationships with local prescribers where only two or three strong local referral relationships has built many robust DSM practices. This, combined with lower-friction pathways for diagnosing via home sleep testing, the leveraging of rapidly growing telemedicine opportunities, and greater adoption of direct-to-patient marketing and treatment pathways, has contributed to the significant growth of SomnoMed’s – and our dental customers’ – treatment impact. Yet, in relation to the enormous number of undiagnosed, untreated, or unsuccessfully treated OSA sufferers, it’s clear that the field of DSM has been lying outside of the primary sleep ecosystem where millions of patients are seen and treated, successfully or otherwise.

In the DSM arena, manufacturers have historically sold features and benefits to dentists. They’ve swapped market share between themselves, adding little real value to the growth of the industry or to their sleep dentistry customers; “just another lab” selling feature, benefit, and price. Few dentists and fewer manufacturers were educating prescribers and investing in and leading clinical research and publication efforts to influence prescribing habits. The resulting frustration of DSM providers is expressed routinely. We’ve commonly heard: “They (sleep physicians) don’t get it. They won’t change.” It’s clear that regardless of enabling technologies, prescribers (treating physicians) must be educated and on board with the value of the therapy and the value of the therapist – the qualified, expert, sleep dentist – before we, as an industry and a profession, “move the needle” to any significant degree.
The Journey to OAT Acceptance and Adoption
In context, the OAT journey to broad-scale prescriber acceptance and adoption…to a standard of care, actually isn’t so different than that of many other medical therapy journeys in the past, including PAP therapies. In fact, it’s been widely reported that it takes an average of seventeen years for evidence-based practices to be incorporated into routine general health care practices.
From the inception of CPAP reimbursement in the mid 1980s, Respiratory DME companies have depended on prescriber referrals. The literature supported CPAP, and the guidelines and reimbursements were aligned with the clinical research, as we have today with OAT. However, this alone didn’t drive treating physicians to alter their treatment routines. DMEs, together with the major manufacturers, needed to bring the literature, the “why?” (clinical proof sources), and the “how?” (the process) to them, office-by-office, physician-by-physician, and patient-by-patient. The DMEs also had armies of sales reps. By the early 90’s, with PAP still in its infancy, there were no fewer than four local DME reps calling on each sleep physician to educate them and ask for patient referrals.
The respiratory DME companies leaned on the leading manufacturers such as Respironics and ResMed to help them win new referral sources with CE programs, explanation of technologies, features, and benefits. Manufacturers were likewise expected to know the literature of PAP to support an evidence-based decision tree. Prescribers needed to know the “why?” It was understood that prescribers don’t drink their morning coffee with journals in front of them; they don’t attend all of the relevant conferences. However, when they hear and see the same “drum beat” from various credible industry sources, and are brought together with their peers that may be a bit ahead of their curve, they gain a comfort level in moving toward newer recommendations and patient care routines. In short, they needed confidence that they were practicing evidence-based medicine. Then, and only then, did they move to the “how?” with the right product(s), patient care services (DME), and patient treatment pathways to support their practice and patient care needs.
The principles of operation of bi-level PAP devices, with flow algorithms and triggering mechanisms, that were being detailed to physicians in 1991 to enable clinical application of Non-Invasive Ventilation only “mattered” to prescribing physicians after several more years of industry advocacy and education, supported by clinical research and publication. Thirty years later, non-invasive ventilation is a standard of care, and CPAP clings to the title of “gold standard” for OSA treatment. SomnoMed’s Medical Initiative is modeled around a similar proven approach to clinical adoption.
As DSM participants of SomSummit ’22 will attest, leading Key Opinion Leaders in the field of Sleep Medicine view OAT as a valid, effective, and important “tool in the tool box,” and are eager to find more trusted and frictionless treatment pathways,and better means of predicting success. They are tremendously excited with the prospect of technologies to finally enable objective, reliable metrics of nightly oral appliance patient compliance and efficacy. DSM has the top-down support of these KOLs and formal guidelines. SomnoMed, with our Medical Initiative, and through strong collaboration with key industry stakeholders whose products and services are integral to frictionless patient and provider treatment journeys, is leading the charge to translate this resounding support into clinical adoption.
Sleep Dentist or DME?
The parallels are clear: the sleep dentist replaces the DME in the CPAP model. What’s missing? AASM guidelines based their robust support of OAT use even as a first-line treatment option and the leading sleep KOLs are on board. So, what barriers remain?
While we can draw strong parallels of OAT to PAP relative to their DME status, there are significant departures, as well:
- DMEs are mostly national and regional, with an additional churn of local providers. Their “armies” can be deployed at scale and with uniformity of patient care and operational efficiencies across state lines. DME providers are also not “sleep medicine” professionals like DSM Providers (dentists), who are held to strict, state-by-state dental practice laws. While ensuring the integrity and quality of their services, these laws may also present barriers to scaled delivery of DSM care.
- DMEs compete ferociously on nuances of service, patient satisfaction, and treatment success. One of their most compelling offerings is providing the prescriber with assurance – through robust, routine communication – that the patients are being treated. Data, by patient and in aggregate, of prescribers’ patient success rates is critical. While DMEs provide objective data via CPAP compliance monitoring technologies, OAT has relied on widely varying, and mostly subjective, reporting of ill-defined OAT treatment success. Future technologies will help to fill the void of objective metrics of nightly compliance and efficacy.
- Dentists are not DME providers. DSM providers walk a tightrope between their role as a commercial DME provider, eager for referrals, and that of a trusted colleague in the field of sleep medicine. Physicians can choose among many CPAP DMEs based on varying service and patient care metrics, but they need and want to know the dentist. Their historical perceptions are often based on poor experience or hearsay of sending the wrong patient to the wrong dentist with wildly exaggerated fees or billing methods, or simply no feedback or follow-up from the dentist at all.
Under SomnoMed’s Medical Initiative structure and process, our team of Business Development Managers, dedicated to calling on prescribing physicians, serve as facilitators of physician-to-dentist relationship building. They introduce only the most highly qualified DSM providers to prescribers, where Dentists are presented as the colleagues and patient care partners they are…not as another DME provider. Business Development Managers explore prescribers’ depth of awareness, understanding, and perceptions of OAT to address the barriers that prevent appropriate consideration of OAT as a means of achieving more successful OSA treatment outcomes.
Barriers to OAT: Real or Perceived?
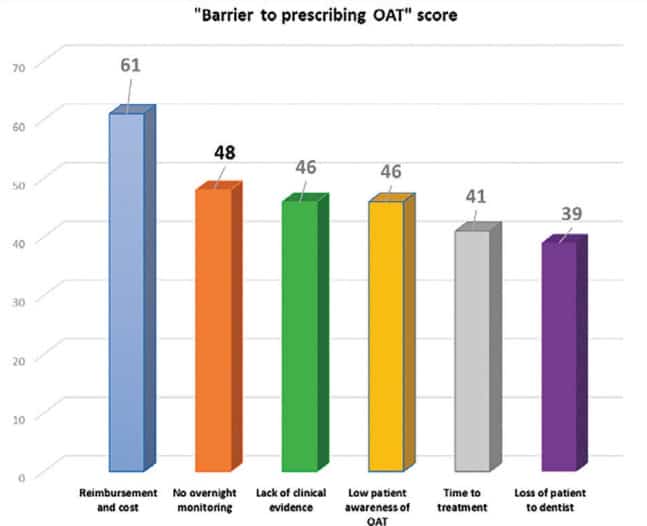
In 2019, SomnoMed surveyed 242 CPAP prescribers to understand the barriers to greater adoption of OAT.
Do these survey results reflect these physicians’ understanding of OAT as a treatment option …or, rather, their perceptions? After all, we know that over a five year span, CPAP patient costs are far greater than those of OAT. How could “lack of clinical evidence” rate so strongly when AASM guidelines are evidence-based? Does “time to treatment” still hold water when CPAP treatment times are now weeks and months in light of the CPAP supply issues stemming from the Philips recall?
While each of these are undoubtedly partial contributors to under-prescription of OAT, there are more significant, overarching barriers. Foremost is the physicians’ level of awareness…and their associated perceptions. Almost all PAP-prescribers are aware of OAT. If they had been merely aware of CPAP in the early 1990s, however, without having been reinforced of its clinical value via a consistent drum beat of supporting clinical publications, podium presentations, and DME reps, would PAP be the dominant therapy it is today? Can DSM address the perceived barriers?
The Road to 100% Effective OSA Treatment
To be effective in representing and advocating for OAT and our expert DSM professionals who provide it, SomnoMed is aware and fully educated in OAT’s potential and value that prescribers are obligated to assess, prioritize, and prescribe for their patients. CPAP is the right therapy for many patients, as are positional devices, surgeries, pharmaceuticals, and OAT. The goal must be one hundred percent treatment success.
DSM is not peripheral, but central to the broader discussions surrounding sleep disordered breathing. SomSummit ’22 helped to further confirm that patients and their physicians need us. Come SomSummit ’23, we’ll look back on progress made and move further ahead with new insight, experience, and perspective toward our common goal of one hundred percent effective OSA treatment.
The most important work to be done is at the local level; physician-by-physician, patient-by-patient. We’ll need a growing army of DSM and medical professionals, industry stakeholders, and key opinion leaders. As we show the successes, identify the failures, and address the real and perceived barriers to broader adoption of OAT as an effective choice, the right choice, for millions of OSA sufferers, the turning point becomes a tipping point.
SomnoMed is involved in finding solutions to dental sleep issues. This CE discusses the many solutions to manage sleep-disordered breathing. Read “Physician-Dentist Collaboration: A Call to Arms for Allied Troops,” and then take the quiz to obtain 2 CE credits! https://dentalsleeppractice.com/ce-articles/physician-dentist-collaboration-a-call-to-arms-for-allied-troops/