Glidewell is dedicated to improving patient access to quality care in dental sleep medicine.
How to fit sleep therapy into a general dental practice
by Randy Clare
If all 150,000 dentists in the United States screened 100% of their patients for SDB as suggested by the ADA, the way we understand the condition would be transformed. Key to the discussion, however, is that dental office procedures are not designed to identify patients who do not receive treatment.
Historically, dentists screen, diagnose, and treat. When it comes to sleep, it’s unclear if they can or how they should do any of these three. So, in most cases, they don’t. And do you know who suffers? It isn’t just the drowsy propane truck driver. It’s the family in the car in the next lane.
In a recent position paper by the American Academy of Dental Sleep Medicine (AADSM) governing the ordering and administration of home sleep testing equipment in their practices, it was noted that there are potentially 43 million American adults with undiagnosed obstructive sleep apnea (OSA).1
In 2017, the ADA clarified the role that dentists should take in screening their patients for OSA as part of their comprehensive medical and dental history during annual recall appointments.2 As a community health effort, this represents a vital opportunity since over 50% of adults see their dentist twice a year.
Once these patients are identified, they are to be referred to a physician for diagnosis and, I would postulate, medical management. The position paper is vague on this aspect of treating these patients. It seems likely that patients who suffer from undiagnosed OSA will also suffer from a wide variety of other medical conditions that will require medical oversight.
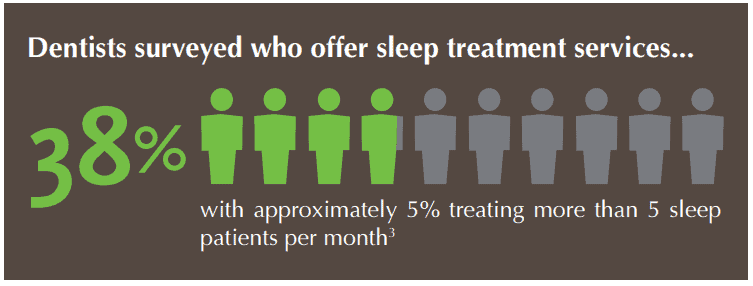
I was very excited about the ADA policy when it was released in 2017. The real impact so far has quelled some of my initial enthusiasm. An Inside Dentistry survey found that only 38% of dentists surveyed offer sleep treatment.3 The more alarming number was that only 5% of respondents treated more than five sleep patients per month.
Let’s rely on the clarity of simple math to connect some dots and underscore this reality. If we can agree that there are 140,000 dentists in the country, and 38% (53,000) have an interest in dental sleep therapy, then only 2,660 make five appliances or more.
This may be a bigger issue than the oft-reported shortage of board-certified sleep physicians, estimated to be only 5,700 throughout the country.
Glidewell has been identified by Frost and Sullivan as the nation’s largest sleep therapy dental lab, producing about 30% of the sleep therapy appliances that are delivered in the U.S. every year.
Our internal records show that some 90% of the dental practices involved in dental sleep treat three or fewer patients per year. This seems to confirm, on a larger scale, the findings of the Inside Dentistry survey regarding the current state of oral appliance therapy treatment.
30% of the population believes treatment is worse than sleep apnea itself.
On a side note, it is striking that often the first patient has the same last name of the dentist who prescribed the appliance. On average, the second appliance comes in many months later. This may not be just a screening issue. Perhaps the treatment of sleep apnea in the dental office, as currently envisioned, is just too complicated, particularly in a post-COVID world.
I completely agree with Dr. David Schwartz’s comment in Dental Sleep Practice that the last paragraph of the AADSM position paper on HST is central to the whole discussion about the role of dentistry in sleep care.4 That paragraph reads, “As health care providers who live by the ethical code ‘do no harm’ and understand the harmful consequences of OSA, we owe it to the public to implement models of care that reduce barriers to diagnosis and treatment, ensure that sleep apnea is diagnosed, and treatment efficacy is verified by physicians and maximizes the training and skills of qualified dentists.”
HST is an invaluable tool for the titration of oral appliances. John Viviano, DDS, D.ABDSM told me once that “a dentist titrating sleep appliances without an HST is like a nutritionist not owning a scale.” However, some state dental boards do not support dentists dispensing HST.
The critical point in all of this is that we don’t want to create a barrier to meeting the need of the patients or to the dentists who are now required to screen for sleep-disordered breathing (SDB). This screening can easily be accomplished with an Epworth Sleepiness scale or a STOP-BANG questionnaire. These documents can readily be added to standard health history forms.
U.S. Census department estimates there to be 255,369,678 adults in the United States in 2021. Dentists will have conversations with approximately 125 million of them twice this year. We know that 62 million will have some form of sleep disordered breathing (SDB), including the 9% to 38% of the population that suffers from the OSA group that the AADSM is largely focused on.5
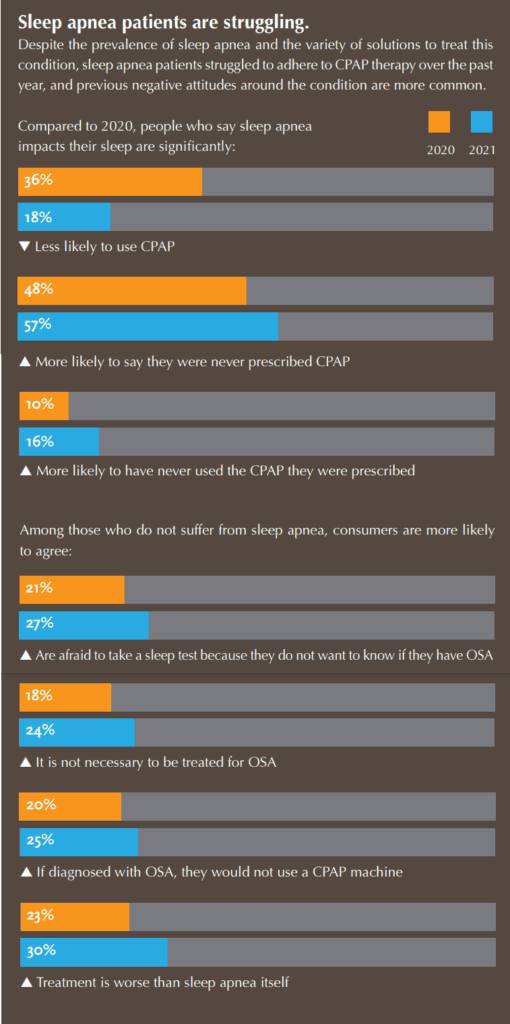
Philips Respironics, one of the worlds largest manufacturers of CPAP and CPAP accessories, published a report on the state of sleep therapy for World Sleep Day. In this report, they highlighted that patients do not seek a diagnosis for SDB because they believe CPAP is the only treatment.
Of the patients surveyed:
- 27% will not take a sleep test because they do not want to know if they have OSA
- 24% of the patients screened do not believe treatment is necessary
- 30% of the population believes treatment is worse than sleep apnea itself.
Of what benefit to patients or dental practices is a screening that requires a multi-step sleep apnea diagnostic process the patient has already decided they do not want?
What most people want, is to alleviate their chief complaint – snoring. It is clear that the dental treatment for snoring is highly effective (so effective Glidewell has a money back guarantee), and not all snorers have OSA, but all OSA patients snore.
The treatment of snoring does not require a physician’s prescription or an objective diagnosis and can be started immediately.
At Glidewell, where the fundamental motivation is to improve patient access to quality care, we believe that patients that present symptoms of snoring should be treated provisionally for that primary complaint. They will be treated with an inexpensive oral appliance (Silent Nite, EMA) using materials and techniques that are found in a general dental practice and pay out of pocket for the care provided.

The appliance should be titrated and managed as is usual and customary. The one caveat is that the patient must sign an informed consent document attesting to the fact that they have been advised about OSA and the importance of seeing a physician for medical management and sleep diagnostics if required.
A downloadable copy of an informed consent document is available on the Silent Nite page on Glidewell’s website.6 Any approved appliance will suffice for this care. The document was prepared by Dr. Ken Berley, a dentist and attorney with an extensive background in dental sleep medicine. This document has been downloaded several thousand times. The response has been excellent.
The ADA has made the screening of SDB a dental mandate. The AADSM has opened the door for the use of sleep testing for appliance titration. This should give general dentists the confidence that OAT is a service that patients can expect to be available, like tooth whitening, occlusal guards and clear aligners, in any practice from every dentist.
The focus on the medical model, medical reimbursement, pre-treatment diagnostics, and medical referrals can be a barrier to entry. It affects the patient and the dentist and is just too difficult for most practices. This has limited the practice of OAT to a very few practitioners whose practices tend to be limited solely to sleep therapy.
Therefore, OAT should be provided on a provisional basis for a low price in order to introduce OAT to the wider patient population. This will build confidence in the general dentist that the ADA’s screening policy will lead to revenue in the practice. Patients will return to the practice, after their physician consult, and some of them will have a diagnosis of OSA but most of them will be happily snore-free. All of them will tell their friends and family, and that will help the YELP review…and that is a good thing.
Glidewell continues to spread the word about dental sleep medicine at its Dynamic Education Center. Read more about it here: https://dentalsleeppractice.com/industry-news/glidewell-dental-unveils-dynamic-education-center-for-emerging-techniques-in-dental-technology/.
- Schwartz, D., Adame, M., Addy, N., Cantwell, M., & Hogg, J., et al. (2020, October 10). American Academy of Dental Sleep Medicine Position on the Scope of Practice for Dentists Ordering or Administering Home Sleep Apnea Tests. Special Article 1, Issue 7.4 – American Academy of Dental Sleep Medicine. https://aadsm.org/journal/special_article_1_issue_74.php.
- Burger, D. (2017, October 31). Sleep-related breathing disorder treatment outlined in new policy. https://www.ada.org/en/publications/ada-news/2017-archive/october/sleep-related-breathing-disorder-treatment-outlined-in-new-policy.
- Mazda, J. (2019, January). Trends In Dentistry January 2019 Page 16. Inside Dentistry. https://lscpagepro.mydigitalpublication.com/publication/?m=7169&i=551575&p=18&ver=html5.
- Schwartz, D. (2021). How Do Dentists Tackle the 54-million-pound Elephant Called Sleep Apnea? Dental Sleep Practice Spring 2021. https://issuu.com/medmark/docs/dsp_spring2021_issuu/10.
- Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, Hamilton GS, Dharmage SC. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Med Rev. 2017 Aug;34:70-81. doi: 10.1016/j.smrv.2016.07.002. Epub 2016 Jul 18. PMID: 27568340.
- Glidewell Dental Lab. (n.d.). Silent Nite Sleep Appliance. glidewelldental.com. https://glidewelldental.com/solutions/sleep-dentistry/mandibular-advancement-devices/silent-nite- sleep-appliance.

 Randy Clare, Glidewell’s director of business development in dental sleep medicine, brings more than 25 years of experience in the sleep therapy and pulmonary function fields. He has held numerous management positions throughout his career and has demonstrated a unique perspective of alternate care diagnostic and therapy models. Clare is considered by many to be an expert in the use of oral appliances such as the Silent Nite Sleep Appliance to treat snoring and sleep apnea in the dental office. For more information, follow
Randy Clare, Glidewell’s director of business development in dental sleep medicine, brings more than 25 years of experience in the sleep therapy and pulmonary function fields. He has held numerous management positions throughout his career and has demonstrated a unique perspective of alternate care diagnostic and therapy models. Clare is considered by many to be an expert in the use of oral appliances such as the Silent Nite Sleep Appliance to treat snoring and sleep apnea in the dental office. For more information, follow