Myofunctional practitioner, Sharon Moore, begins her series on the link between sleep and airway, and ways that dentists can help screen patients.
by Sharon Moore
In this multi-part series, author, speech pathologist, and myofunctional practitioner Sharon Moore shares the ramifications of poor sleep on mental, emotional, and physical wellbeing, along with screening techniques to help dental teams identify the common red flags of disrupted sleep. In subsequent issues, she will introduce myofunctional therapy as a method to optimize growth, development and maintenance of healthy facial and upper airway structures to counteract sleep disorders like sleep disordered breathing and upper airway resistance syndrome.
In Part 1, Sharon outlines the importance of sleep for adults and children, as well as highlighting the link between sleep problems and upper airway issues. She also shares how dentists are perfectly positioned to screen problems early and collaborate with other health professionals on intervention.
In America, 70% of adults report experiencing insufficient sleep at least one night a month, and 11% report insufficient sleep every night.1 Meanwhile, a British study showed 77% of British adults do not wake refreshed,2,3 and an Australian study reported inadequate sleep, of either duration or quality, affecting 33-45% of Australian adults.4
In children, up to 40% of 4 -10 year-olds have sleep problems – that’s a lot of children!5 Furthermore, since 80% of kids’ sleep problems are missed, dismissed or misdiagnosed, there are gaps that must be bridged in screening, education and clinical solutions for sleep problems. This is partly attributable to lack of education across community and professional groups, but also because sleep problems can masquerade as behavior and learning problems.6 Regardless, it’s a very big problem.
The Consequences of Poor Sleep in Adults
There is not one body system nor one domain of health, social, or workplace functioning that is not impacted by poor sleep, yet many adults remain unaware of the importance of sleep. In fact, the cost to governments for untreated sleep problems is in the billions.7
Furthermore, we know that sleeping only 6 hours per night can decrease immunity by 70%, notwithstanding the other possible consequences of poor sleep: chronic inflammation, tumor growth, stress and impacts on endothelial, endocrinological, metabolic, cardiovascular, and integumentary systems.8
The Consequences of Poor Sleep in Children
The same goes for children. There is not one system nor domain of childhood development not affected by poor sleep; physical, mental, emotional or social no matter the cause or the severity.9,10,11 The impacts may have ripple effects throughout childhood, adolescence, and beyond when untreated; including the very education and safety of our children by way of the neuro-behavioural and cognitive deficits associated with poor sleep.12

So, What is Good Sleep?
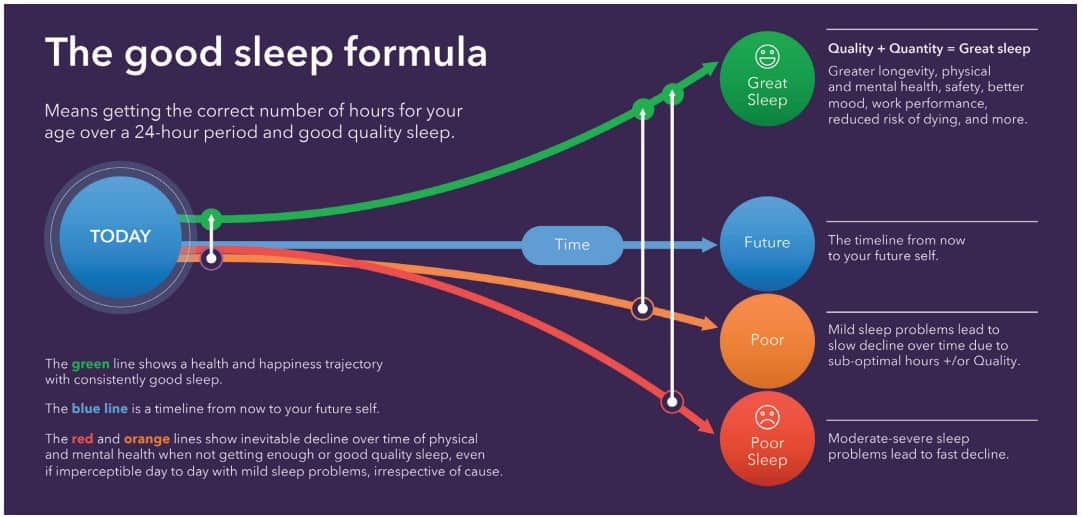
It’s quite simple: good sleep = correct quantity + good quality. The results of good sleep are waking refreshed and managing natural energy peaks and troughs throughout the day.16
Bad sleep, in contrast, is any version of insufficient quantity and/or poor-quality sleep, which can impact our physical, mental, and emotional health. Bad sleep can also have a deleterious effect on performance, safety, and productivity.17
 Where Does Upper Airway Fit in this Picture?
Where Does Upper Airway Fit in this Picture?
Poor sleep is a global epidemic – ‘perhaps one of the greatest challenges of the 21st Century.’18 Insomnia is the biggest problem and sleep disordered breathing (SDB) ranks second. SDB hinges directly on upper airway health and function, with conditions including obstructive sleep apnea (OSA), snoring, upper airway resistance syndrome, respiratory effort related arousals and mouth breathing.
Currently, the apnea-hypopnea index (AHI) that measures OSA does not capture the full spectrum of narrowing and collapse of the upper airway that occurs in SDB, leading to varying degrees of poor-quality sleep. The outcome is disruption of breathing and sleep architecture.
With 40% of cranio-facial growth being complete by age 4 and 90% complete by age 11-12, there is a critical window of opportunity to develop the healthiest possible airway.
 What Does that Mean in a Dental Practice?
What Does that Mean in a Dental Practice?
The ADA states “All dentists should screen for SDB/OSA.” 19,20 Dental teams are face-to-face with patients every single day, on the frontline for identifying sleep and upper airway issues.
Here are the top three things dental teams can do:
- Screening: Use sleep questionnaires and screen for upper airway issues impacting sleep, including anatomy, tissue, and neuromuscular function.
- Education: Promote sleep and healthy upper airway along with dental hygiene to your whole team as well as your patients.
- Clinical solutions: If you have adequate knowledge of dental sleep medicine, be part of the multidisciplinary team treating SDB/OSA patients.
 It Takes a Team
It Takes a Team
Approximately 30% of sleep problems can be solved by developing healthy sleep habits.21 The rest require expert help from medical, dental, and allied health professionals.
Dental teams truly are on the frontline to help patients and their families discover the life-changing magic of great sleep.22 However, to provide complete solutions for patients’ airway and breathing issues, it’s essential to work alongside other medical and allied health professionals whose expertise is required for developing and maintaining healthy breathing during sleep. These include sleep specialists, ENTs, oro-maxillofacial surgeons, allergists, and myofunctional therapists, among others.
Sleep and Health in the 21st Century
While poor sleep has far-reaching negative consequences, the converse is true for good sleep. Good sleep leads to optimal emotional, physical and mental development in children, optimal work and academic performance, road and occupational safety, robust mental and emotional health for adolescents and adults.
It is mission critical for everyone to get the sleep they need every night to be healthy and happy. In order to achieve this, over the following three installments I will expound upon how to screen for disordered sleep and recognize the common red flags that represent when sleep is less than optimal. I will also introduce myofunctional therapy as a tool to address upper airway issues, including giving an overview of key oral functions that assist in the development of the airway, and sharing some of my go-to exercises for patients presenting with SDB and other issues of the upper airway.
Finally, I will take an in-depth look at Upper Airway Resistance Syndrome, including its impact on sleep and development, the challenges of identifying the disorder, and how dental teams can contribute to screening for and treating this disorder.
By engaging with this series, you can help create the face(s) of our future and solve one of the greatest health challenges of the 21st Century.
Sharon Moore further discusses the link between sleep and airway in children, in her book Sleep Wreched Kids. Read more about it here: https://dentalsleeppractice.com/industry-news/putting-childrens-sleep-problems-to-bed/.
- Centers for Disease Control and Prevention. Perceived Insufficient Rest or Sleep Among Adults—United States, 2008. Morbidity and Mortality Weekly Report 58:1179
- Sealy UK & Loughborough University Clinical Sleep Research Unit. (2016) The world’s largest-ever online ‘sleep census’ reveals a sleep-deprived planet. [Online] Available from: http://www.lboro.ac.uk/media-centre/press-releases/2016/november/the-worlds-largest-ever-online-sleep-census-reveals-a-sleep-deprived-planet.html
- Institute of Medicine, ‘Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem’, (Washington, DC: National Academic Press, 2006), https://doi.org/10.17226/11617.
- Adams, Robert J., Sarah L. Appleton, Anne W. Taylor, et al. “Sleep Health of Australian Adults in 2016: Results of the 2016 Sleep Health Foundation National Survey.” Sleep Health3, no. 1 (2017): 35-42. doi:10.1016/j.sleh.2016.11.005.
- Owens & Chervin, ‘Behavioral Sleep Problems in Children’, https://www.uptodate.com/contents/behavioral-sleep-problems-in-children
- David L. Rabiner, Jennifer Godwin and Kenneth A. Dodge, ‘Predicting Academic Achievement and Attainment: The Contribution of Early Academic Skills, Attention Difficulties, and Social Competence’, School Psychology Review 45, no. 2 (2016): 250–67, https://doi.org/10.17105/spr45-2.250-267.
- ‘The Price of Fatigue’, Harvard Medical School, PDF document, December 2010, https://sleep.med.harvard.edu/file_download/100.
- Luciana Besedovsky,1,2 Tanja Lange,1,2 and Jan Born1,2, Sleep and immune function, Pflugers Arch. 2012 Jan; 463(1): 121–137. Published online 2011 Nov 10. doi: 10.1007/s00424-011-1044-0
- Sharon Moore, Sleep-Wrecked Kids: Helping Parents raise happy healthy kids one sleep at a time. (New York: Morgan James publishing 2019).
- Alison L. Miller, Julie C. Lumeng and Monique K. Lebourgeois, ‘Sleep Patterns and Obesity in Childhood’, Current Opinion in Endocrinology & Diabetes and Obesity 22, no. 1 (2015), https://doi.org/10.1097/med.0000000000000125.
- Ann C. Halbower, Mahaveer Degaonkar, Peter B. Barker, Christopher J. Earley, Carole L. Marcus, Philip L. Smith, M. Cristine Prahme and E. Mark Mahone, ‘Childhood Obstructive Sleep Apnea Associates with Neuropsychological Deficits and Neuronal Brain Injury’, PLoS Medicine 3, no. 8 (2006), https://doi.org/10.1371/journal.pmed.0030301.
- Obrien, ‘Neurobehavioral Implications of Habitual Snoring in Children’, Pediatrics 114, no. 1 (2004): 44-49, https://doi.org/10.1542/peds.114.1.44.
- Karen Bonuck, Ronald D. Chervin and Laura D. Howe, ‘Sleep-Disordered Breathing, Sleep Duration, and Childhood Overweight: A Longitudinal Cohort Study’, The Journal of Pediatrics 166, no. 3 (2015), https://doi.org/10.1016/j.jpeds.2014.11.001.
- Karen Bonuck, Ronald D. Chervin and Laura D. Howe, ‘Sleep-Disordered Breathing, Sleep Duration, and Childhood Overweight: A Longitudinal Cohort Study’, The Journal of Pediatrics 166, no. 3 (2015), https://doi.org/10.1016/j.jpeds.2014.11.001.
- David L. Rabiner, Jennifer Godwin and Kenneth A. Dodge, ‘Predicting Academic Achievement and Attainment: The Contribution of Early Academic Skills, Attention Difficulties, and Social Competence
- Sharon Moore, Sleep-Wrecked Kids: Helping Parents raise happy healthy kids one sleep at a time. (New York: Morgan James publishing, November 2019).
- Sharon Moore, Sleep-Wrecked Kids: Helping Parents raise happy healthy kids one sleep at a time. (New York: Morgan James publishing 2019).
- Matthew Walker, Why We Sleep. Penguin Random House, October 2017
- Silvia Gianoni-Capenakas, DDS, MSc, PhD1, Andre Chiconelli Gomes, DDS2, Pedro Mayoral, DDS, MSc, PhD3, Manuel Miguez, DDS, MSc, PhD4,5, Benjamin Pliska, DDS, MSc, PhD6, Manuel Lagravere, DDS, MSc, PhD7, Sleep-Disordered Breathing: The Dentists’ Role – A Systematic Review, Journal of Dental Sleep Medicine, Review Article 1, Issue 7.1, http://dx.doi.org/10.15331/jdsm.7108
- American Association or Orthodontics Whitepaper, (2019) https://www.semanticscholar.org/paper/American-Association-of-Orthodontists-White-Paper-%3A/cbddda450eb7be89dbf 192e87445f3c443764856
- Sarah Blunden, ‘Behavioural Sleep Disorders across the Developmental Age Span: An Overview of Causes, Consequences and Treatment Modalities’, Psychology, 3 (2012): 249–56, https://doi.org/10.4236/psych.2012.33035.
- Sharon Moore, ‘Sleep Disorders are in your face’, in The 2nd AAMS Congress (Chicago, 2017).
 Sharon Moore is an author, speech pathologist and myofunctional practitioner with 4 decades of clinical experience across a range of communication and upper airway disorders. She is on the transdisciplinary team for the Canberra Sleep Clinic and has a special interest in early identification of craniofacial growth anomalies in children, concomitant orofacial dysfunctions and airway obstruction in sleep disorders.
Sharon Moore is an author, speech pathologist and myofunctional practitioner with 4 decades of clinical experience across a range of communication and upper airway disorders. She is on the transdisciplinary team for the Canberra Sleep Clinic and has a special interest in early identification of craniofacial growth anomalies in children, concomitant orofacial dysfunctions and airway obstruction in sleep disorders.