by Patrick Tessier, MBA
Appliance selection is one of the most important decisions a clinician makes when treating a patient with Sleep Disordered Breathing (SDB). Breaking down the academic, clinical, and financial benefits of the two major advancement categories can provide clarity on the overall effectiveness of appliances.
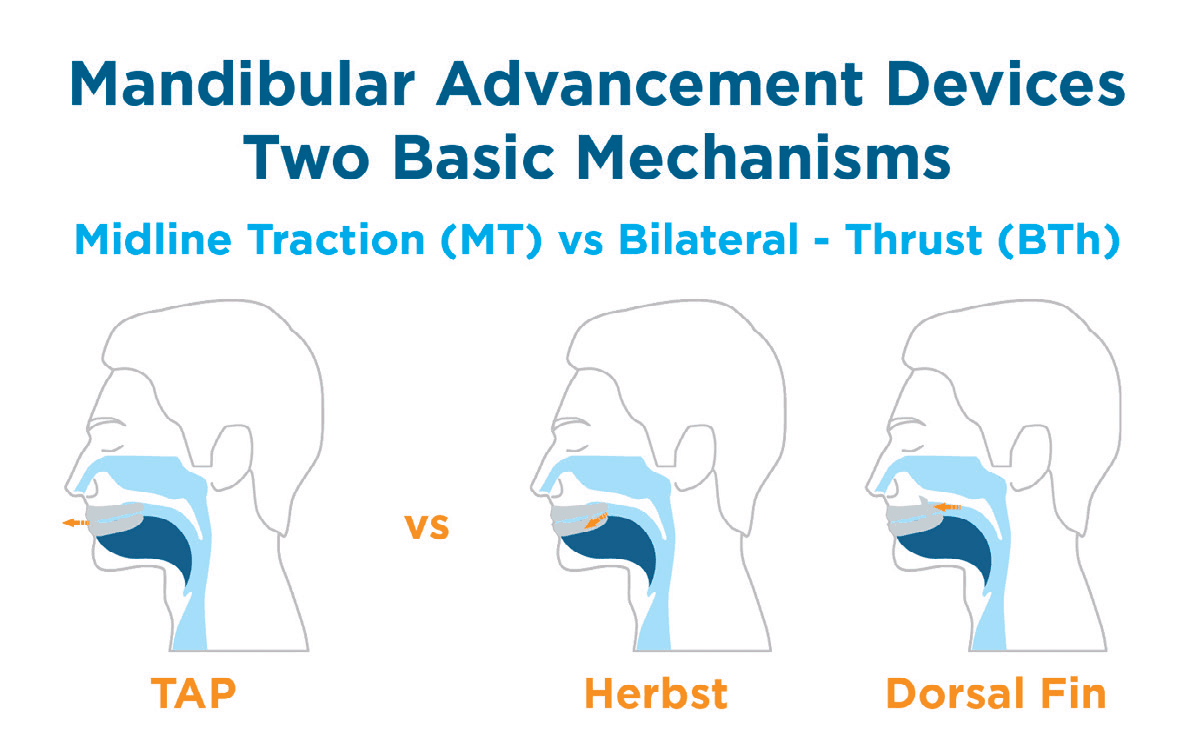
Mandibular Advancement Devices (MAD) are generally segmented into two advancement mechanism categories, midline traction (MT) and bilateral thrust (BTh).
- MT devices have a single point of midline adjustment in the anterior of the device. The most popular and recognizable midline device is the TAP Custom Appliance.
- BTh devices have two points of adjustment; one on each side of the arch. The two most common devices in that category are the Herbst and Dorsal Fin appliance.
The easiest way to differentiate between the two categories is “push vs. pull”. The midline device pulls the mandible forward while bilateral devices push the mandible forward.
Academic
In 2015, the American Academy of Sleep Medicine (AASM), updated their clinical guidelines to include a literature review comparing the effectiveness of various devices against CPAP and Oral Appliance criteria. The literature review found that:
Midline devices
- 100% met the Oral Appliance criteria
- 50% met the CPAP criteria
Bilateral devices
- 20% met the Oral Appliance criteria
- 0% met the CPAP criteria
Based on these peer reviewed studies, data supports the efficacy of midline traction devices.

mechanisms. Image courtesy of Airway Management, Inc.
Clinical
Both comfort and compliance are key to clinical success. Concerns about comfort are the most common reason cited for CPAP noncompliance. An effective treatment modality must also be comfortable for the patient to use which usually equates to higher levels of treatment compliance.
Comfort: While anecdotal and not the experience of every patient, let me share my first experience with a bilateral device.
After the appliance was delivered, I instantly stopped snoring. My wife loved it. However, after just a few nights, I started to notice jaw pain in the morning. After a week, I could barely open my mouth in the morning. Finally, I called the dentist to complain. He asked if it hurt on one side or both sides. It was just on one side. He said that the midline was off and had me move the screw on one side to compensate.
Bilateral devices require two independent adjustment mechanisms requiring modification. This can lead to an issue whose origin can be found when the initial protrusive bite is taken. If the patient inadvertently bites to one side, even slightly, the device can be manufactured with an offset midline. This causes the device to stretch the muscles and ligaments on one side and induces pain. With midline devices this problem does not exist as there is only a single point adjustment that allows for lateral movement.

Compliance: If patients don’t wear their devices, their SDB will remain untreated. One of the most effective methods clinicians can use to increase compliance is patient engagement. When a patient is engaged and takes some measure of ownership, they are much more likely to feel empowered in their treatment and overcome short-term obstacles to wearing the device.
Single point adjustment is so simple, the patient can be involved in the titration process. By giving them an adjustment key with a titration schedule, it becomes “their treatment”. Bilateral devices are generally more complicated as patients may inadvertently turn one of the screws the wrong way and cause additional pain.
The literature is also quite clear that if the mandible falls open, soft tissue is more likely to obstruct the airway. With bilateral devices, many clinicians address this issue by adding clasps and orthodontic rubber bands. This increases the complexity of the treatment and reduces compliance. With single point midline adjustment, the advancement mechanism does this by design. The hook in the anterior prevents the jaw from dropping down and eliminates the need for clasps or bands.
Financial Implications
Medicare is the most restrictive payor and allows reimbursement for only TAP, Herbst, and Snorehook oral appliances. Dorsal fin devices and all others are not covered by Medicare. Private insurance companies, seeking to reduce their liability, are beginning to restrict approved appliances to only those that are PDAC approved. The conservative approach, advocated by many third-party billers, is to use a PDAC approved device to avoid potential reimbursement issues.
The profitability of a DSM procedure is largely determined by the chair time required to complete the treatment. If the patient returns several times for adjustment or advancement, the profit margin for that procedure decreases.
This is where the simple adjustment mechanism of the single point device shines. The patient advances the device on their own; following the titration schedule limiting the amount of advancement per day. Cases that are treated with single point mechanisms are more likely to be profitable than those cases requiring chair time for every 0.5mm advancement.
Conclusion
Whether evaluating academic, clinical or financial implications, midline adjustment devices are the extremely effective. More than 500,000 TAP appliances have been delivered. These MT devices are PDAC approved and a litany of research has demonstrated their effectiveness for the normalization of AHI.