Dr. Alan D. Steljes explains the bodily processes that can make sleeping and travel difficult, and he offers some solutions to help sleep better at night so you can get the most out of your vacation time.
 by Alan D. Steljes, MD, FACC, FRCPC
by Alan D. Steljes, MD, FACC, FRCPC
Imagine this: You have been planning for a much needed vacation. Your trip will take you to Europe for a week. You have packed the schedule with an ambitious program in your enthusiasm to “see all the sights.“ You are aware of the time change, so you booked an overnight flight, reasoning that you can sleep on the plane and be ready for adventures on arrival.
En route from Chicago to London, you managed to eke out about four hours of sleep on the 8 hour flight. All is going according to plan.
On arrival, it is 10 a.m. local time, and you are excited to see your first destination, the Tower of London. After standing in line for four hours, you are understandably tired. You enjoy a nice dinner, then look forward to going to bed at 10 p.m. local time. This is great, you think. I will be on local time within the first day. Easy!
Much to your chagrin, you lie awake for hours, unable to sleep. You get only about 4 hours of sleep that first night, before you have to get up in the morning for a scheduled tour. You feel excessively tired during the day and feel like you may nod off at any time. The second night is only a little better. Your normally robust appetite is now poor despite some enticing food options. You’ve had some bowel issues. You find yourself dragging to keep up with your busy schedule. You do feel significantly better after about a week (just as you are getting ready to return to the US.)
Obviously, this is jet lag. This syndrome is associated with complaints of insomnia or excessive daytime sleepiness accompanied by a reduction in total sleep time. There is impairment of daytime function and general malaise. Somatic complaints are common after the first or second day (poor appetite, inappropriate timing of defecation, excessive urination.)
The degree of dysfunction depends on various factors including the number of time zones crossed, the direction of travel (westward travel is better tolerated), sleep loss during travel, availability of daylight at the destination, and one’s ability to tolerate circadian misalignment.
What is the problem? Your internal clock is out of synch with the local time. We say that your internal circadian rhythms are phase delayed with respect to the local time zone. The 10 p.m. bedtime in London is only 4 p.m. for you. Your brain is not at all prepared to sleep.
In EASTWARD TRAVEL, people have difficulty falling asleep and staying asleep because they are trying to sleep at a time when the circadian alerting signal is high. Adaptation requires a phase advance i.e. falling asleep at an earlier time with respect to your internal clock. London is 6 hours ahead of Chicago. You need to phase advance your bedtime by 6 hours. Your body will eventually adapt to the new time zone, without any change in routine. However, it typically adjusts by only half an hour a day when traveling eastward.
The process should start at home, beginning 3 days prior to your flight. Try to go to bed one hour earlier each night and get up earlier each day. Exposure to bright light in the morning is helpful to consolidate your shift in bedtime. Adding melatonin 0.5 mg or 3 mg prior to the usual bedtime may have additional benefit.
Consider scheduling travel to arrive at your destination at least 2 days before any important events, (for example a speech or a wedding) to give your body some time to adjust.
An overnight flight is helpful, by matching the flight time to your normal sleep schedule. Optimize your sleep time as much as possible. Noise cancelling headphones or eyeshades may help. Your physician may prescribe a sleeping pill. Regardless, you will still lose sleep time on a typical 6-8 hour long transatlantic flight.
After arrival, we can speed up the adaptation process, but we will have to use our knowledge of those circadian processes which induce sleepiness at bedtime and promote alertness during the day. Melatonin secretion and core body temperature are the most relevant for bedtime sleepiness. We fall asleep with rising melatonin blood levels and falling core body temperature.
The timing of these processes are governed by our internal clock, our master pacemaker, which is the suprachiasmatic nucleus (SCN) located in the anterior hypothalamus. The SCN has cells which cycle independently with a time period which is close to 24 hours. The SCN must be “entrained” to local time by external clues, the most powerful of which is exposure to daylight.
We can shift the timing of our internal clock by the strategic use of light and melatonin. The rule is that melatonin “pulls” while light “pushes.” This is best visualized by referring to Figure 1.
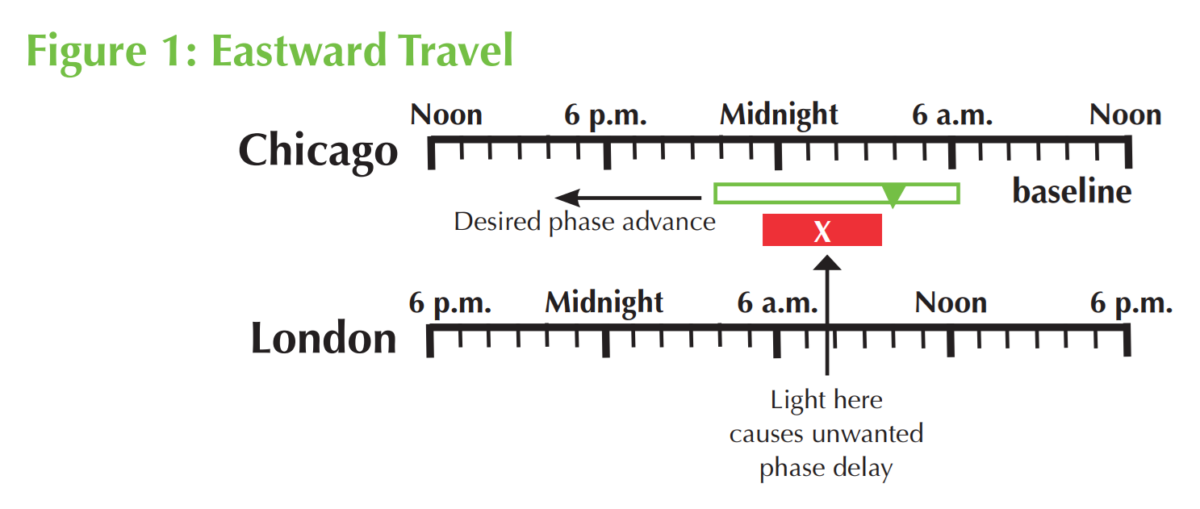
The evening rise in melatonin secretion and the minimum core body temperature (CBTmin) are two useful markers of the position of an individual’s circadian rhythm with respect to the local time of day. The CBTmin occurs 2 to 3 hours before our natural awakening.
After your arrival in London, you should have avoided exposure to light before 10 a.m., by wearing sunglasses or staying indoors. Exposure to light prior to CBTmin, will reset your clock in the wrong direction.
We can shift the timing of our internal clock by the strategic use of light and melatonin. The rule is that melatonin “pulls” while light “pushes.”
Ideally, you want to expose yourself to sunlight between 11 a.m. to 2 p.m. Light exposure after the CBTmin will “push” the CBTmin in the desired direction. Avoid evening light as you are approaching your new bedtime.
Melatonin at your new bedtime is an option to “pull” the CBTmin earlier i.e. phase advance.
In WESTWARD TRAVEL, people may experience sleepiness prior to bedtime which may make falling asleep easier, but they may have difficulty maintaining sleep for as long as desired since the internal circadian alerting signal will be rising during the sleep period. Adaptation requires a phase delay. That is the individual will go to bed later than customary. Westward travel is typically better tolerated, since it is easier to stay up later at night than to get up earlier in the morning. Adaptation to western travel is also quicker i.e. about one hour a day.
Pre-flight adjustment may not be necessary. However, phase delaying could be tried before travel begins (go to bed later, get up later) using evening bright light for 1 to 3 hours. Daytime flights are preferred.
Light should be avoided in the morning in the new destination (if it occurs soon after CBTmin) to prevent phase advance. Exposure to light in the evening (if before CBTmin) may be helpful (phase delay). See Figure 2.
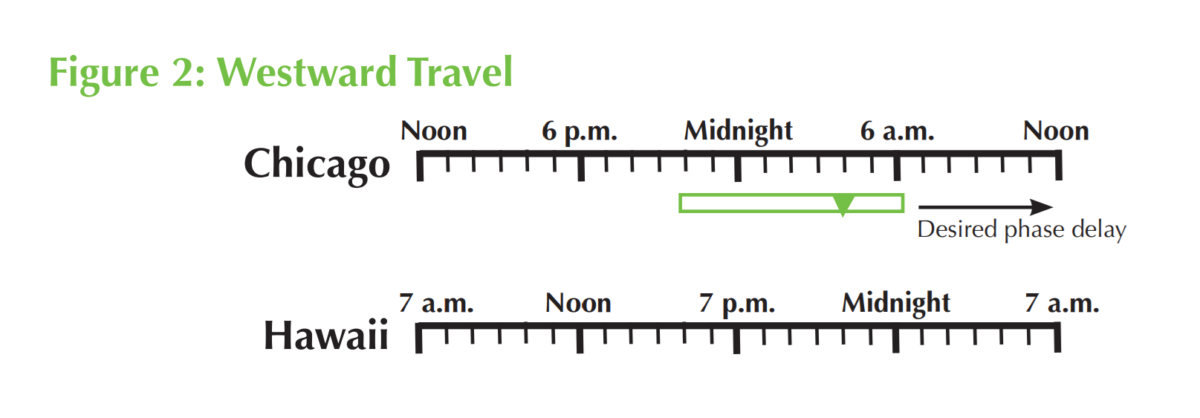
Melatonin use for westward travel can be counterproductive if not timed carefully. For example, melatonin at bedtime in the destination, if taken before CBTmin, induces phase shift in the wrong direction (phase advance). Taking melatonin on awakening is the correct time for phase delay but may make the individual sleepy during the day.
If melatonin is used, it is recommended that a small dose (to avoid prolonged sleepiness) be taken during the last half of the night.
Crossing More Than Eight Time Zones
After eastward flights, very early light (inappropriate phase delay) should be avoided.
On westward flights, light at dusk (inappropriate phase advance) should be avoided for 2 to 3 days. Thereafter, light at the usual times may help with adaptation.
Some physicians recommend attempts at phase delay even if the direction of travel is eastward when more than eight time zones are crossed.
It does get complicated. There are websites which will customize a schedule for you including wake times, bed times, caffeine, and melatonin.
Finally, these common-sense steps will help you adjust and avoid jet lag symptoms.
- You should follow the sleep and waking routines of your destination when you arrive.
- Hypnotic sleeping pills at bedtime may help with sleep but do not necessarily help with alertness the next Even if you get adequate sleep, decreased circadian alertness will occur at the time of CBTmin
- Take meals on the local schedule. Eat small meals to avoid stomach aches or other problems.
- Avoid alcohol as it disrupts sleep.
- Use caffeine and exercise strategically; these may help you stay alert throughout the day, but you should avoid these after noon.
- Drink plenty of water.
- If you are sleepy during the day, take short naps, no more than 15-20 minutes, to help you feel better during the day, yet still sleep at night.
Good luck on your travels.
Sleeping and travel are complicated enough — but whether you are away or at home, nosebreathing is fundamental. Read more about helping your patients breathe correctly in “Healthy Cells, Healthy Brain: Nose Breathing is Fundamental”: https://dentalsleeppractice.com/healthy-cells-healthy-brain-nose-breathing-is-fundamental/.

 Alan D. Steljes, MD, FACC, FRCPC was trained as an interventional cardiologist. Since fellowship, he has obtained additional certification in nuclear cardiology, echocardiography, CT coronary angiography and finally sleep medicine. In 2010, he opened a two bed sleep lab, recognizing the heart-sleep apnea interaction. The initial 2 beds have been scaled up to 12 beds since associating with the Nevada Heart & Vascular Center. He has since retired from the cardiology practice but continues to oversee the sleep program. He remains passionate about spreading the word about sleep disordered breathing and the heart. He currently shares his time between Las Vegas, NV and Mount Pleasant, SC.
Alan D. Steljes, MD, FACC, FRCPC was trained as an interventional cardiologist. Since fellowship, he has obtained additional certification in nuclear cardiology, echocardiography, CT coronary angiography and finally sleep medicine. In 2010, he opened a two bed sleep lab, recognizing the heart-sleep apnea interaction. The initial 2 beds have been scaled up to 12 beds since associating with the Nevada Heart & Vascular Center. He has since retired from the cardiology practice but continues to oversee the sleep program. He remains passionate about spreading the word about sleep disordered breathing and the heart. He currently shares his time between Las Vegas, NV and Mount Pleasant, SC.