by Samuel J. Higdon, DDS

This is the fourth article in a series that has addressed the issues of Temporomandibular Disorders (TMDs) as they relate to providing Oral Appliance Treatment (OAT) for Sleep Disordered Breathing (SDB) such as Obstructive Sleep Apnea (OSA). In previous articles I have discussed the risks of developing a TMD in response to OAT (Winter 2016), what the Sleep Dentist needs to know about TMDs (Spring 2017), and what is involved in screening your SDB patients for potential TMDs (Fall 2017), even if there are no overt signs and symptoms of such problems. For those who find this information valuable, I recommend reviewing these previous articles prior to reading this fourth article, as I will reference several things I have mentioned previously.
In this fourth article, I will discuss some aspects of the anatomy of the temporomandibular joints as it relates to potential TMD issues associated with OAT. The limitations of space prevent an in depth discussion of TMJ anatomy. However, a free ebook, Illustrated Anatomy of the Temporomandibular Joint in Function / Dysfunction with text and illustrations by this author, is available for download at http://tmjoregon.com/downloads/TMJ_Anatomy_eBook.pdf/. This will provide a foundation for understanding many aspects of TMJ anatomy.
In a recent issue of the Journal of Dental Sleep Medicine1 (JDSM), a panel of experts appointed by the American Academy of Dental Sleep Medicine discusses in some depth several potential side effects of OAT. It addresses four categories of side effects – I will be discussing only those related to the anatomy of the temporomandibular joint.
First, some context. It is important to appreciate that structural changes within the temporomandibular joints are common, as represented by a quite high prevalence of joint sounds, clicking and popping of the joints, caused primarily by displacement of the articular disc. Many studies have demonstrated that this occurs more frequently in females than in males. As just one indication of this high prevalence, Nebbe and Major2 found that in pre-orthodontic adolescents who presented for orthodontic treatment, MRI of the TM joints demonstrated disc displacement of 50% in males and up to 75% in females. Not only is the prevalence of disc displacement extremely common, the disc can displace in a number of directions (Fig. 1).3 This variability of disc displacement challenges some assumptions that have existed since disc displacements were first described by William Farrar in 1971.4
Most dentists are aware of how common joint sounds are but tend not to give them much consideration. As discussed in previous issues, the prevalence of joints sounds in a potential OAT patient should NOT be treated with complacency. An understanding of TMJ anatomy, in general, and its implications for OAT is essential knowledge for the Sleep Dentist. In all potential OAT patients, a clear understanding of the condition of the patient’s TM joints is a must. Therefore, a screening TMJ exam, (as previously described), must be done to minimize the potential for a problem of the temporomandibular joints developing in response to OAT.

Figure 1: Directions of Disc Displacement
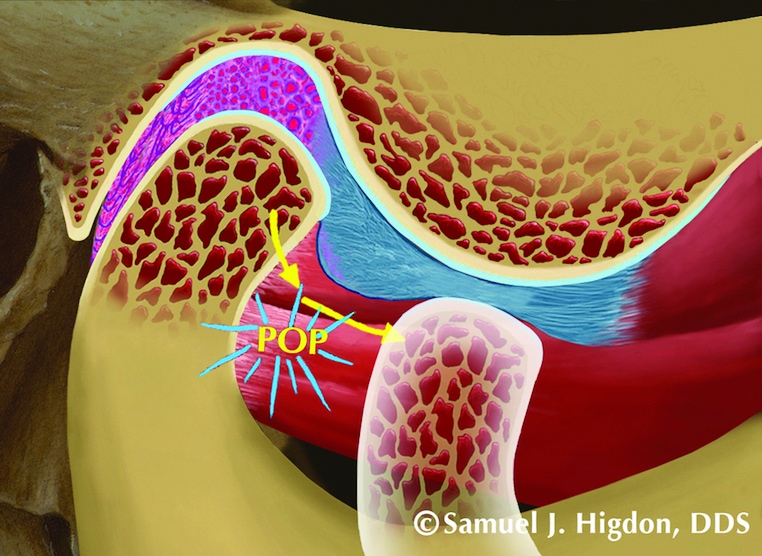
Figure.2: Articular Disc Displacement with Reduction (Click/pop)
The authors of the JDSM side effects article list four sub-categories; 1) Transient morning jaw pain, 2) Persistent temporomandibular joint pain, 3) Tenderness in muscles of mastication, and 4) Joint sounds. A screening TMJ exam will reveal the likelihood of any of these to develop, providing the basis for an informed consent discussion with the patient prior to beginning OAT.
I will describe three possible scenarios that might be encountered with OAT as related to the anatomy of the TM joints:
Joint Clicking/Popping With or Without TMJ Pain
Clicking and popping of jaw joints is common (Fig. 2). In a patient in which it occurs easily, with no indication of catching or locking, it will be important to evaluate for pain from the TM joints. Use palpation through the ear canal to the distal of the joint, as well as provocational joint loading. If there is no increase in pain in response to this testing, the potential for any untoward side effects from OAT are minimal. Your joint exam ruled out pain arising from intracapsular structures.
Even when clicking/popping of the TMJs occurs easily, if pain is found from this type of joint examination, positioning the mandible forward for several hours is likely to unload the retrodiscal tissues and thereby relieve the intracapsular pain. This can be beneficial. However, after removing the Mandibular Advancement Device (MAD), the mandible would be expected to return to the original position within the fossa, allowing normal intercuspal position (ICP) of the teeth, but would allow loading the retrodiscal tissues again. If the patient had previously not been particularly aware of pain subjectively, from the joint(s), the re-loading of the retrodiscal tissues may produce joint pain that the patient will then notice, resulting in blame being assigned to OAT. They might discontinue using the MAD, seek other treatment, or create complications for ongoing OAT. It would be far better to have discovered the joint pain, prior to initiating OAT, and discussed it with the patient.
Joint “Reluctance” to Return to ICP Upon Removal of the MAD
As discussed in a previous issue, it is considered standard protocol when doing OAT, to provide the patient with an “AM repositioner” that encourages the condyles to resume their original joint position in the fossae, thereby allowing the dental occlusion to return to ICP.
However, cases have been reported in which, after the condyles have been maintained in an “on disc” protrusive position for several hours, there has clearly been a “reluctance” of the condyles to resume their original position within the fossae, even with the use of the “AM repositioner”. The author has personally had this occur with his own jaw. The cause of this “reluctance” is not known with certainty but it is presumed that, once the condyle is able to assume an “on disc” position, the morphology of the disc, primarily the shape of the posterior band of the disc, is such that it is somewhat difficult for the condyle to once again move off the disc. When this occurs, the result will be a change in the dental occlusion, usually with a posterior open bite, most notable on the side of the affected condyle. There may also be a slight shift of the mandible away from the affected side as a result of a slightly more anterior condylar position on that side.
It is difficult to anticipate when this may occur. It seems less likely to occur when clicking/popping of the joint, prior to OAT treatment, has been mild, indicating that the condyle is easily moving on and off the disc. When the tendency to maintain an “on disc” position does occur, the question then arises as to whether this new condylar position should be maintained, possibly requiring treatment of the resulting occlusal change, or whether the condyle should be allowed to return to its previous position, probably off the disc, and usually suggesting that OAT treatment is no longer a viable option for treatment of OSA. The considerations will vary, based on differing findings. But a decision to maintain the “on disc” position and to treat the resulting occlusal change is a challenging treatment option, requiring quite a lot of clinical experience. It definitely does not represent a conventional case of treatment of malocclusion and will often require a combination of treatment options.
Joint Pain Resulting From OAT
Joints that are most likely to become painful with OAT are joints that have either locked (disc displacement without reduction) or joints that have undergone degenerative changes (osteoarthrosis). In a joint that has locked (Fig. 3), certain clinical findings will be seen with a fairly high degree of consistency. With recently locked joints, opening range of motion will be limited and typically, with opening, the mandible will deflect toward the locked side. Similarly, there will often be a protrusive deflection toward the affected side and lateral condylar movement on the affected side will typically be less than on the non-affected side. However, in joints that have been locked for some time, these clinical findings will be less apparent. Perhaps the most important finding that may suggest whether OAT is appropriate would be pain from the affected joint with any of the movements mentioned above.

Figure 3: Disc Displacement without Reduction (Locked)
With a joint that is locked, the disc has been displaced and the condyle does not move on to the disc. The condyle, during any translatory movement, simply encounters the folded posterior band of the disc and, with protrusion, pushes on the disc. This can produce intracapsular pain. If, with the screening exam, joint pain occurs with joint movement, it may be possible to test the possibility for OAT with the use of a temporary trial appliance. The author has used several for this purpose. One possible temporary appliance would be the ZQuiet, which is available in several configurations from 0 mm to 6mm of protrusion.
In joints that have undergone degenerative changes (osteoarthrosis), frequently these will be pain-free on examination, even when course crepitation can be heard with auscultation. If, in such joints, range of motion is near normal and no pain is produced with such movements, the patient may tolerate a MAD. However, caution will be the watchword and a temporary trial appliance may be a good starting point. There will be the possibility of joint pain developing in degenerative joints and change in the dental occlusion may be seen. Again, these are considerations that should be discussed with the patient prior to initiating OAT.
Clearly, not all patients with mild to moderate OSA are candidates for OAT. When a patient does not seem to be an OAT candidate, there are other options. One that the author has used effectively is a tongue stabilizing device (aveoTSD), which, by utilizing suction on the tongue, brings the tongue forward to open the airway without having any effect on the position of the jaw.
All Sleep Dentists are encouraged to become knowledgeable regarding the normal and dysfunctional anatomy of the temporomandibular joints. The ebook offered earlier in this article is a very good place to begin.