In this edition, I continue with the discussion of questions posed to me at the American Academy of Dental Sleep Medicine (AADSM) annual meeting last June. I admit that I have struggled with the questions pertaining to “E” codes, so I asked Rose Nierman of Nierman Practice Management to help me write this very important article.
E codes are level II Healthcare Common Procedure Coding System (HCPCS) codes in the medical coding system that are used primarily to identify products, supplies, and services not included in the CPT codes, such as ambulance services and durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS).
The questions: I was asked by Adam with Slumberbump™ about using E-codes to bill medical insurance for positional therapy used as a conservative or adjunctive treatment for snoring and Obstructive Sleep
Apnea (OSA). Additionally, I was asked by Stacy with Go-Go Billing about the usage of E codes to bill medical insurance for lab-fabricated morning repositioners. We will look at both questions in this article.
E-codes for Positional Therapy
When we think about E codes for positional therapy, a number of issues immediately come to mind. Who will be the prescribing physician? Will the patient’s physician prescribe the positional pillows for insurance purposes or will the treating dentist be the prescriber? Legally, the protocol would be easier to defend if the patient’s sleep physician’s signature was on a prescription with a statement of medical necessity.
The positional pillow may well be considered medically necessary for the treatment of OSA. We have an Explanation of Benefits (EOB) from Tricare, as well as from a private carrier, for reimbursement for a positional pillow. Therefore, we know that some carriers are providing coverage. However, can the dentist distribute these? Obviously, what a dentist can or cannot do is determined by the state board of dental examiners in their respective states. So ultimately each state could be different. However, the one state that I am concerned about is Georgia. With the new statute on Dental Sleep Medicine (DSM), positional therapy might not be within the scope of practice for a dentist. The Georgia Statute states:
Depending upon the diagnosis of the type and severity, one possible treatment option for obstructive apnea is the use of oral appliances. The design, fitting and use of oral appliances and the maintenance of oral health related to the appliance falls within the scope of practice of dentistry. The continuing evaluation of a person’s sleep apnea, the effects of the oral appliance on the apnea, and the need for, and type of, alternative treatment do not fall within the scope of dentistry.
Does the dentist need a written order from a physician for a positional pillow? The answer to that depends on the individual policy. Medicare, for example, does not provide reimbursement. On the other hand, some private insurers may reimburse, without a prescription, for the code, E0190; “Positioning cushion/pillow/wedge, any shape or size, includes all components and accessories,” Not all Durable Medical Equipment (DME) requires a prescription or a written order. Also, positional pillows are not on any published list stating that a written order is required. Medicare and some commercial carrier have published lists of DME that require written orders, while some insurers state in their DME policies that ALL DME requires a prescription from a physician.
Morning Repositioners
As a brief history, prior to July of last year, I was using a hard lab-fabricated morning repositioner. My lab cost was approximately $150, and I was charging $400 for this appliance. I was filing medical insurance using HCPCS code S8262 with a letter of explanation/medical necessity. I was relatively successful in getting reimbursement for morning repositioners. In July of last year, CMS removed the S8262 code and we stopped billing medical insurance for these devices. I began using an AM Aligner (non-lab fabricated device) and included that service in the cost of oral appliance therapy (OAT). However, upon request, Rose and I revisited this issue.
Some insurers state that ALL DME requires a prescription from a physician.
To begin this discussion, be aware that some dentists are using code E0485 for the morning repositioner. That code is for a prefabricated device: “Oral device/appliance used to reduce upper airway collapsibility, adjustable or non-adjustable, prefabricated, includes fitting and adjustment.” This description does not adequately describe how a morning repositioner functions, so we do not suggest the use of that code to represent morning repositioners. Additionally, if you are using a simple non-laboratory fabricated AM Aligner, do not file medical insurance for that service. That is just WRONG! Give that to the patient, don’t be greedy.
In our opinion, the best code for a Lab-Fabricated morning repositioner seems to be E1399. E1399 is a code which is billable and sometimes payable for “Miscellaneous DME”. One commercial carrier states that this code is to be used; “For any other devices without a specific code, claims should be filed with the applicable unlisted code.”
As far as whether a morning repositioner requires a prescription, you should know that the Medicare policy manual contains the following statement: “A prescription or physician written order is required within 6 months of the physician Face-to-Face appointment for DME.” Similar language is seen in private insurer’s DME policies and is also referenced in the Affordable Care Act (ACA). The Affordable Care Act addresses this; displayed in the screenshot below:
Notice the Act states “certain types of DME.”
When a dentist provides DME, such as an oral appliance, a prescription or Detailed Written Order (DWO) is required from one of the physician categories listed in the screenshot above. The accepted physician categories for the DWO are a licensed MD, DO, nurse practitioner, clinical nurse specialist, or physician’s assistant working within their scope of practice.
While Medicare considers a DDS & DMD to be in the “physician” category for Part B services, that is not the case when we are treating OSA. When we are providing oral appliance therapy (OAT) for Medicare beneficiaries, we are no longer physicians (due to the requirement to enroll as a DME supplier for custom made OSA devices). Therefore we cannot prescribe them under Medicare guidelines. The term “physician” does not include a dentist (DDS or DMD) per the Medicare Local Coverage Determination LCD for Oral Appliance Therapy. Although many carriers do not reference Medicare’s guidelines, in the past year, increasingly more insurance companies now follow Medicare’s guidelines for OAT. Given that, it is my opinion that a Rx should be obtained with a letter of medical necessity for positional therapy from the patient’s sleep physician. This Rx could then be used on an “as needed” basis. This Rx will be in addition to your prescription for the mandibular advancement device. It is my legal opinion, that if we have the Rx from the patient’s sleep physician for the positional therapy, we are certainly within our scope of practice to determine when and if positional therapy should be employed during the OAT titration/calibration process of our patients.
Prescriptions and Detailed Written Orders (DWO)
The big issue is who can prescribe positional pillows? It goes without saying that a physician could order and prescribe positional pillows in conjunction with a custom made oral appliance for OSA (E0486). It also appears that the morning repositioner needs to be part of the sleep physician’s treatment plan and a prescription written for the appliance in addition to the E0486. BCBS’s policy on covered DME states that they may cover other items per the physician’s plan of treatment:
 Another question to answer is whether a morning repositioner could be considered an accessory to a MAD appliance or is it a totally unrelated item for billing purposes. This is from Noridian which addresses accessories:
Another question to answer is whether a morning repositioner could be considered an accessory to a MAD appliance or is it a totally unrelated item for billing purposes. This is from Noridian which addresses accessories:
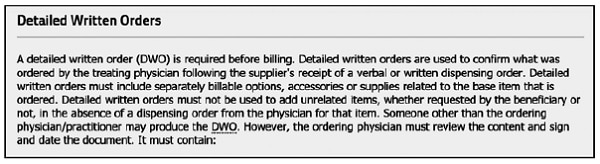 From our research, it appears that DME suppliers have a reputation of adding unnecessary items to physician’s prescriptions. These “add-ons” alter the prescription and make it invalid. So the question is, could a morning repositioner be considered an add-on to a prescription for an E0486, making the Rx invalid? The answer could be yes! Therefore, the prudent approach is to get a separate Rx for the morning repositioner if you’re going to bill for it.
From our research, it appears that DME suppliers have a reputation of adding unnecessary items to physician’s prescriptions. These “add-ons” alter the prescription and make it invalid. So the question is, could a morning repositioner be considered an add-on to a prescription for an E0486, making the Rx invalid? The answer could be yes! Therefore, the prudent approach is to get a separate Rx for the morning repositioner if you’re going to bill for it.
Sadly, morning repositioners are not addressed anywhere in any insurance policy that we are aware of. Therefore we do not know whether a morning repositioner is considered a part of the treatment of OSA with E0486. It possibly could be considered part of the “fitting and adjustment” or it could be considered an accessory of the E0486.
Therefore, since morning repositioning is not addressed in policies, the insurer could say that any payment made for morning repositioning was made in error and ask for recoupment.
In conclusion, I think it is possible to file both positional therapy and morning repositioning to medical insurance using the codes indicated in this article. However, I think it is prudent to obtain a prescription and letter of medical necessity for both items from the patient’s sleep physician. We would suggest that you charge no more than three times the cost of the item in question to prevent a claim of overbilling.
You should understand we are now in uncharted waters and it is certainly possible that an insurance company could ask for all their money back for either item in the future. The act of recoupment is used any time an insurance company pays for an item for a period of time and then changes their mind. At that point, you could be asked to come up with a lot of money. Be aware and forewarned!