
As the subspecialty of dental sleep medicine has evolved and matured, reasonable concerns have been voiced regarding potential undesirable results from doing mandibular advancement during sleep as a long-term treatment for sleep disordered breathing (SDB). Several studies have been done on long-term changes that may occur, including not just TMD-related effects, but also skeletal changes and changes in the dental occlusion.1 Skeletal and dentoalveolar changes have been reported.2
From a long-term perspective, the risk for developing TMD signs and symptoms because of treatment with a mandibular advancement device (MAD) seems to be low. Apparently, the masticatory system has a good capacity for adaptation if MAD use continues, with an overall reduction in TMD symptoms as well as a slight increase in range of motion.3 However, in the short term (up to 6 months), risks remain.
The sleep dentist should be aware of these studies and be prepared to discuss them with patients being considered for treatment using a MAD. However, long-term problems are not the focus of the present article. Identifying the potential for short-term development of a temporomandibular disorder (TMD) prior to undertaking MAD treatment will lessen the need to explain to the patient what has occurred and what may happen if treatment with the MAD is to continue and whether the TMD symptoms may persist even if MAD treatment is terminated. After-the-fact explanations are best avoided, if possible.
In the previous article (DSP Spring 2017) I made the argument that most dentists primarily think of temporomandibular disorders (TMDs) as pain problems. The risk associated with this limited perspective is the assumption that if the patient isn’t complaining, there currently isn’t, and that there won’t be, a problem. The potential for TMD problems often can be detected in an incipient state, based on certain clinical signs that can be present before there is any pain and before the patient is otherwise aware of a problem. The need for a careful evaluation of the patient for potential TMD problems is of particular importance when MAD treatment is being considered.
As discussed in the previous article, several dental organizations, including the ADA4,5,6,7,8 have for years advocated that ALL dentists screen ALL of their patients for TMDs, yet it appears that few dentists do so routinely. One reason for this may be that most dentists may not know what it means to screen their patients for TMDs nor how to incorporate a screening protocol into their practice. A protocol for introducing a routine screening procedure for TMD into any dental practice will be described (see Fig. 1).
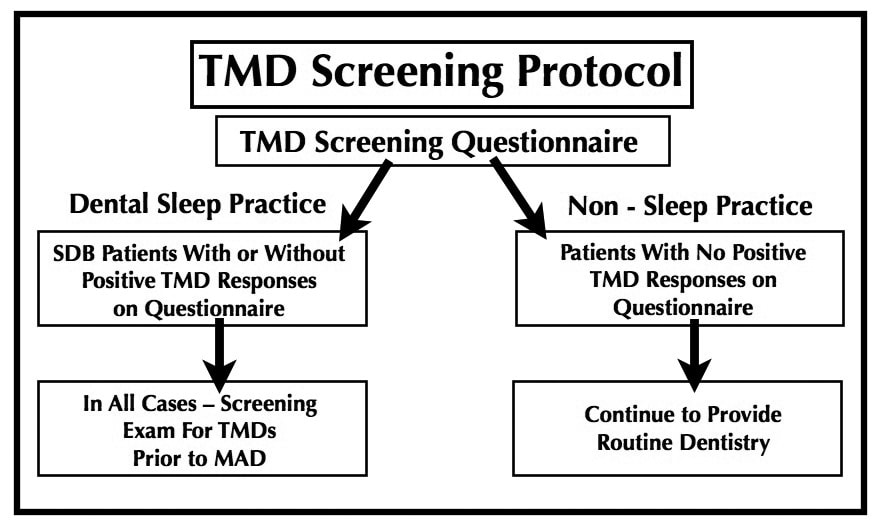
In a conventional dental practice, screening of patients for TMDs would initially require only the routine use of a screening questionnaire. If given to each new patient, and again at regular recall visits with all patients, significant changes that may develop over time will be identified at the earliest possible time while continuing to provide routine dental care.
If there are positive findings, or indications of progression over time on the screening questionnaire, the next step would be a TMD screening exam.
All SDB patients should not only complete the screening questionnaire but also have a TMD screening exam, for indications of possible incipient TMD problems, prior to consideration of possible use of a MAD. Certain findings on a screening exam may suggest that the use of a MAD may be contraindicated, at least until the TMD issues have been adequately addressed.
It is worth mentioning, in this context, that a dental hygienist can be trained to do a screening TMD exam, the results of which can then be conveyed to the dentist for consideration.
The Screening Forms
Because the Screening Questionnaire (download at https://dentalsleeppractice.com/forms-higdon/) can be administered by front office staff, it can easily become a part of routine office procedure for all patients without requiring any additional time on the part of office staff, including the dentist.
The author’s background has involved extensive training in the clinical application of dental occlusal principles. However, in spite of having been well-trained in these concepts, in addition to 30+ years of experience in doing a comprehensive occlusal examination, I have come to recognize that the feedback that the patient can provide regarding how their bite actually feels to them will often add a level of clarity to the occlusal assessment over and above the results of a conventional occlusal examination. For this reason, in my TMD practice, I now ask every patient who has been referred to me to complete the Patient Self-Assessment of Occlusal Condition questionnaire as part of their intake procedure. Responses to these questions have added immeasurably to our otherwise comprehensive TMD history and examination.
It is important that this Patient Self-Assessment of Occlusal Condition (download at https://dentalsleeppractice.com/forms- higdon/) is not seen as a substitute for either the screening questionnaire or the screening exam. It simply adds to what may be found when a proper TMD screening history and exam are done. The Patient Self-Assessment of Occlusal Condition form can provide important information regarding the patient’s perception of their own dental occlusion.
Following forward posturing of the mandible during sleep using a MAD, it is generally expected that the patient’s mandible will be able to return to their previous intercuspal position (ICP) shortly after awakening. Current accepted protocol advocates providing the patient with an “AM repositioner” to aid in this process. If the patient, on the Patient Self-Assessment of Occlusal Condition questionnaire, has in some way indicated that their existing ICP has been uncomfortable (not necessarily painful – perhaps uneven, uncomfortable, strained) to them before MAD treatment, or if there has been an intracapsular problem involving limited range of motion or catching of the joint, such problems may represent a complicating factor when the patient attempts to return to their ICP upon awakening.
Identifying potential issues in advance of MAD treatment can avoid some challenging outcomes that would otherwise be difficult not only to explain to the patient, but also to resolve in a satisfactory manner.
One example: If the pre-existing ICP had been maintaining the mandible in an asymptomatic but retruded jaw (condylar) posture, upon removal of the MAD in the morning, it may become apparent, even with encouragement provided by use of the “AM repositioner”, that the mandible does not easily return to the previous ICP. When properly evaluated, this may indicate that a somewhat more protrusive position is a more physiologic position for the mandible. This is not to suggest that the jaw will maintain the full protruded position that the MAD provides, but only that the mandible may not easily return fully to the pre-existing ICP.
If on the Patient Self-Assessment of their Occlusal Condition, the patient had indicated that their jaw is more relaxed and comfortable in a somewhat forward position, or if they indicate that they have heavier contact on their anterior teeth vs. the posterior teeth, this may also suggest that a potential problem involving joint position may need to be evaluated and addressed as a separate issue. There may not be any joint pain, but if pain is present in combination with a description of this kind, it represents a TMD problem that must be addressed before considering MAD treatment. Because MAD treatment under these circumstances could potentially result in a permanent change in condylar position and a resulting change in the patient’s dental occlusion, it may represent a contraindication for MAD treatment, at least until the joint/bite condition has been adequately addressed. Other means of managing the diagnosed airway problem should be used in the interim.
When findings of this kind are present and the patient is otherwise relatively symptom-free, TMD issues may be less a problem of joint pain and more a problem of joint mechanics and jaw posture. Because of the implications regarding potential related bite changes, there will need to be a discussion of this with the patient, including treatment options. One option would be to address the problem of joint mechanics as a separate issue before undertaking MAD treatment. These circumstances can be rather complex and a decision regarding a path forward to appropriate treatment will be dependent on the circumstances, on good clinical judgement, but particularly on the experience of the dentist in managing non-painful but dysfunctional TMD problems.
Decreasing TMD Symptoms with MADs
It has long been recognized that in some instances intracapsular TM joint pain can be relieved with mandibular advancement. If there are accompanying headaches and other muscular symptoms, these, too, may be relieved with mandibular advancement. A finding of intracapsular pain is commonly indicative of adverse loading of the retrodiscal tissues. Relieving this joint pain by alteration of the load on pain-sensitive tissues with a MAD may also decrease the muscular response to the joint pain, thereby affecting muscle symptoms such as headaches. Even with a decrease in symptoms in response to MAD treatment, it is important for the sleep dentist to recognize that they have not “cured” a TMJ problem. It is more likely that these improvements in symptoms will be transitory and that more definitive treatment of the TMD, to address the underlying source of the pain issues, may be indicated, possibly before undertaking MAD treatment for SDB. To describe this set of circumstances succinctly, TM joint pain may be relieved by the MAD treatment and this may be accompanied by a “reluctance” of the mandible to return to the pre-existing ICP.
Increased TMJ Symptoms with MAD Treatment
Under certain circumstances, mandibular advancement may increase joint pain, particularly if done in the presence of certain intracapsular conditions. As described in the Discussion of the Significance of History Questionnaire and Exam Findings form (download at https://dentalsleeppractice.com/forms-higdon/), the potential for these condition to develop are likely to be identified with a careful TMD screening exam.
Pain-free clicking and popping in TM joints that otherwise move well may be inconsequential. Finding joint sounds on examination, however, is not a reason for complacency. They are always an indication of a loss of normal structural integrity of the joints structures and may have further implications. With the patient being considered for MAD treatment, of particular importance would be any finding of limited opening, limited excursions, or deviation and/or deflection on opening. Pain from the TM joints, particularly with palpation through the ear canal to the distal of the joint(s), and/or pain with jaw movements, especially if localized to the TM joints, should be carefully considered as to whether the patient is appropriate for MAD treatment. However, coarse grating and grinding (hard tissue crepitation) will usually be a contraindication for MAD treatment, particularly in the presence of pain from the same joint, as this is an indication of advanced degenerative joint disease (osteo-arthritis). While signs and symptoms of TMD do not necessarily increase during long-term therapy using a mandibular advancement device, patients with clinically detected TMJ crepitation have been shown to discontinue their mandibular advancement device therapy more often due primarily to TMD symptoms.10
The examples described above are not necessarily the only potential problems that might be identified with a TMD screening history and exam. They do, however, suggest the necessity for the sleep dentist to exercise care and good clinical judgement before undertaking MAD treatment for a SDB condition.
As described in the first article of this series (DSP Winter 2016) “Sleep Appliances and TMDs: Are You Ready?”, the importance of having a complete understanding of the potential for your patient to develop a TMD in response to MAD treatment, should that occur, is that you will need to be able to explain to the patient what may have happened. But out of an abundance of caution, not only do you need a well-worded informed consent, you need to be able to explain to your patient, prior to beginning MAD treatment, what you have found that may have the potential to lead to TMD issues. When you are well-informed, and can present your findings in a knowledgeable manner, your ongoing relationship with your patient will be much less likely to result in an uncomfortable condition for either you or your patient.
In the next article, in the Winter 2017 issue, I will discuss more specifically both normal and dysfunctional anatomy of the temporomandibular joints and how an understanding of this anatomy is of importance to not only the sleep dentist, but to every dentist.



