Editor’s intro: Dr. Steven Olmos shows a case study where rhinomanometry measurements and airflow-related treatment led to improvement of TMJ function.
by Steven Olmos, DDS, DABCP, DABCDSM, DABDSM, DAIPM, FAAOP, FAACP, FICCMO, FADI, FIAO
Diane a 62-year-old female, BMI 22, unremarkable medical history with the exception of osteopenia was referred to my office for concerns about jaw joint noises and jaw deflection to the right upon opening in September 2018. She states that it is easy to fall asleep, wakes rested, however she wakes twice nightly to urinate. She injured her neck in a motor vehicle accident in 2000. She occasionally has a dull mild ache on the right side of her cervical spine. Her Epworth Sleepiness Scale and David White Nighttime Sleepiness Evaluation were both zero.
Medications: Lipitor-statin drug, Retasis-ophthalmic emulsion for dry eyes, Travatan-2 reduces pressure from glaucoma, Vagifen-estrogen replacement. She drinks less than 4 cups of coffee per day. She does not smoke tobacco. She does not use alcohol and/or sedatives for pain relief and/or sleeping aids. She denies any trouble breathing through her nose. She has had prior orthodontic treatment. Currently using maxillary and mandibular retainers.
Clinical exam revealed normal BP 102/75, pulse 81, temperature 97.5. Palpation revealed mild pain on right anterior temporalis and right medial pterygoid muscles, right posterior TMJ joint space, left rotated cervical vertebra 5, 6, 7. Moderate pain on right lateral TMJ capsule, and right stylomandibular ligament insertion on medial surface of gonial angle of mandible.
Mandibular ranges of motion were normal: maximum opening 52 mm, left and right lateral at 10 mm, with Class I dental and skeletal relationships.
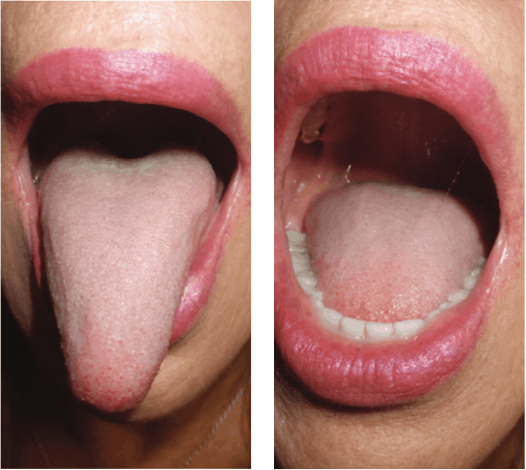
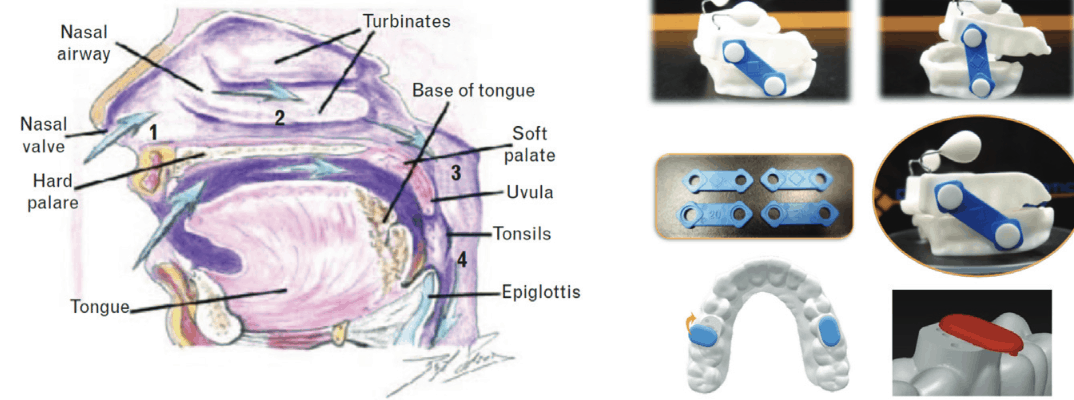
Mallampati Class IV, tongue coated at base and retracts upon opening. These are findings consistent with airway obstruction, as are nasal obstruction and high Mallampati.1,2,3
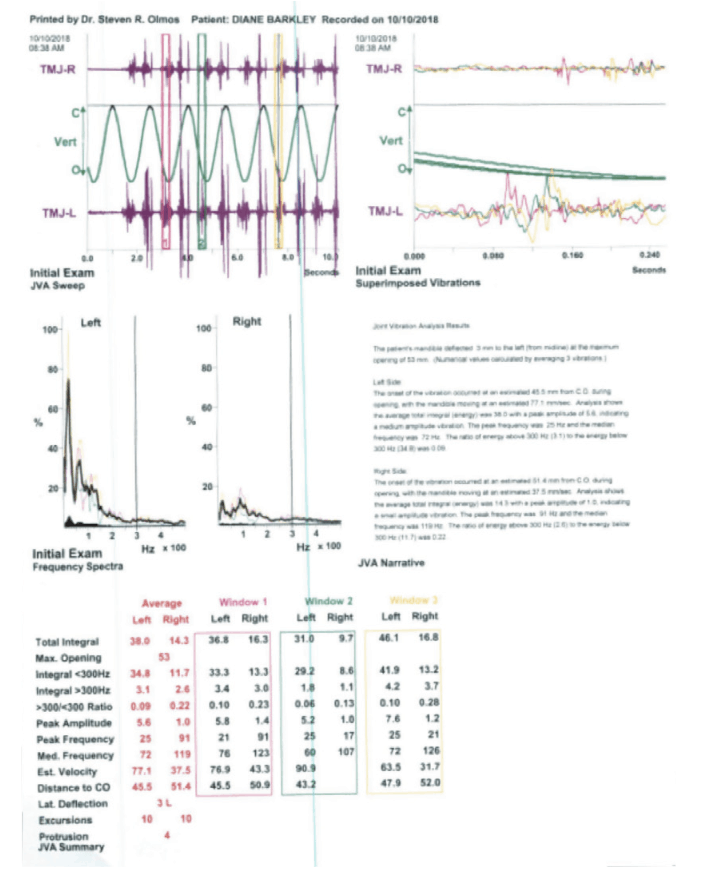
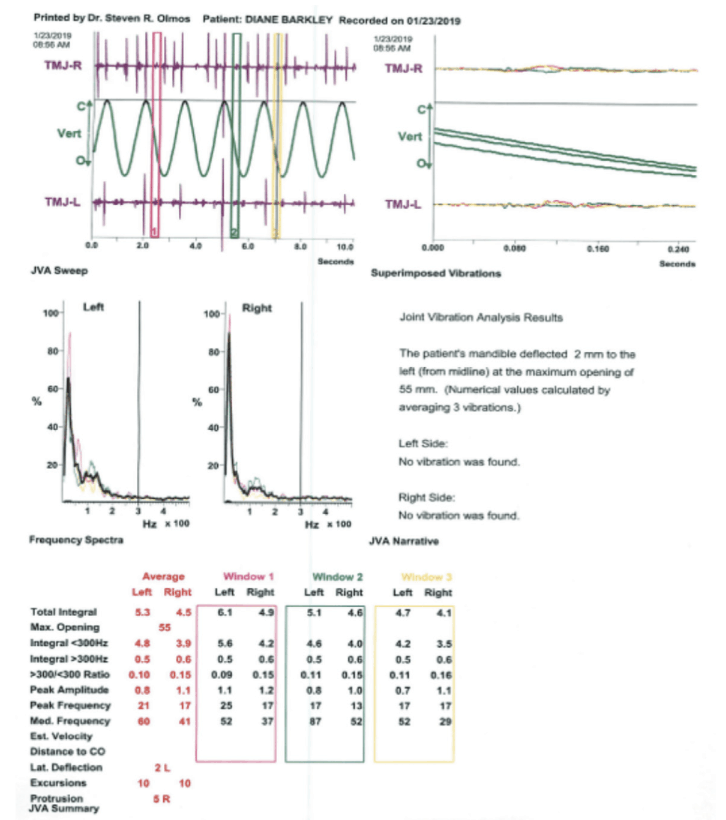
Joint vibration analysis (JVA) (BioResearch, Inc., Brown Deer, WI) demonstrates ligament laxity of the left TM joint, (vibrations greater than 20 Hz indicate pathology), Figure 4. JVA is an instrument that measures the hard and soft tissue dynamically as the jaw is moving to discern either health or pathology.4,5,6,7
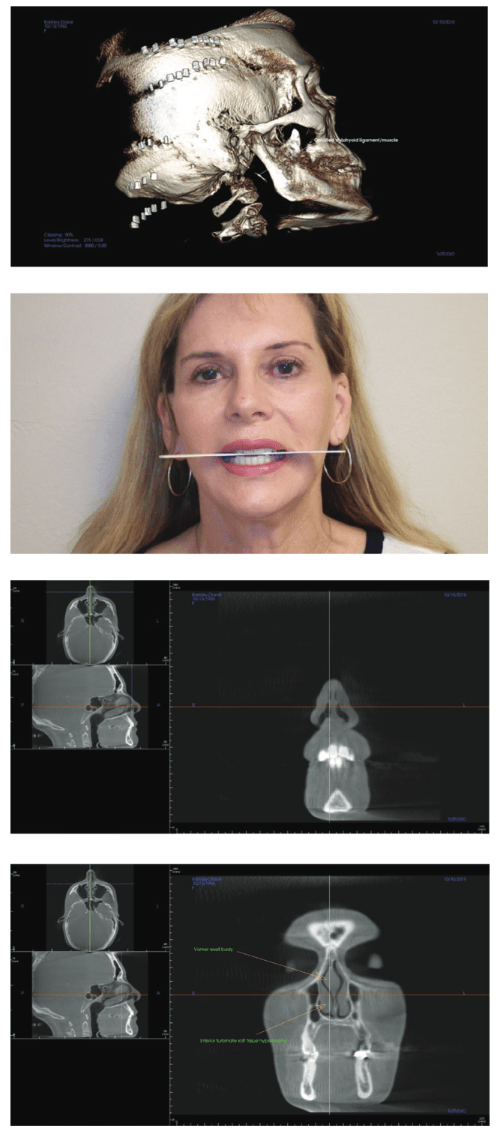
CBCT imaging reveals calcified stylohyoid ligament/muscle on the right side. This is evidence of a long-standing movement disorder. The reason why it is unilateral is that the patient has a cant of the mandible up to the right (Figures 5 and 6).
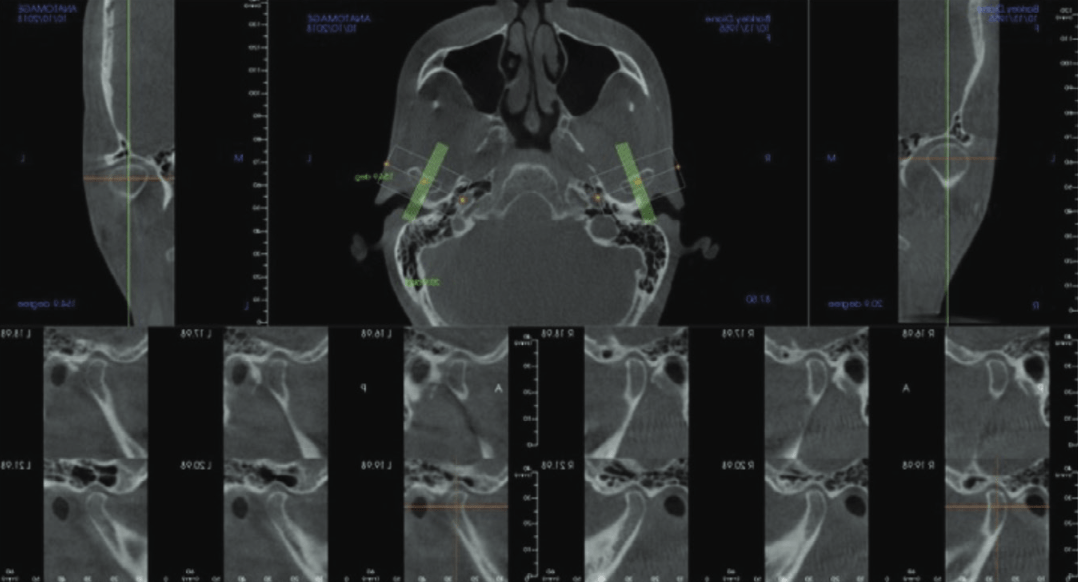
CBCT imaging of the nose demonstrates nasal valve compromise, soft tissue hypertrophy of the Vomer (swell body) and inferior turbinates (Figures 7 and 8). Nasal obstruction results in mouth breathing with facial and masticatory muscle dysfunction.
My Diagnosis
Capsulitis of the TM joint (bilateral). Suspected Sleep Breathing Disorder (SBD), with nasal obstruction. I believe the inflammation and mechanical changes to the joint are secondary to a movement disorder the result of an obstructed airway. Nasal obstruction results in mouth breathing. This fatigues the elevator muscles (temporalis, masseters, medial pterygoids) and the relief to the lactic acid is to contract (clenching). Mouth breathing results in changes to mandibular position and can result in anterior open-bite as referenced in the orthodontic literature (Harvold’s monkeys).8,9 This is due to a weakening of the orbicularis oris muscles and anterior tongue posture. The stretching of the mandible and in turn the TMJ ligaments results in tissue displacement.
Plan
Decompression appliance therapy is needed for the nocturnal forces of sleep bruxism that have produced her craniofacial symptoms. Weekly treatments using the MLS laser (BioResearch, Inc., Brown Deer, WI) to reduce inflammation and shorten stretched TMJ ligaments. While she is undergoing therapy for her orthopedic complaints, she will be referred to a Board-Certified Sleep Physician, and ENT. As I suspect a SBD and know is has nasal obstruction, the decompression appliance will need to maintain a patent airway in all four points of obstruction (Figure 9). Maxillary nighttime therapy is necessary: DDSO (Diamond Digital Sleep Orthotic) is a printed Type 12 nylon appliance with Nasal Dilators and Tongue Pillows. The DDSO is the only appliance that can titrate vertically, protrusively, manage the tongue and the nasal valve simultaneously. The bite registration technique used was the Sibilant phoneme registration, which has been demonstrated to reduce pharyngeal collapse and increase volume of the airway.10 She will be evaluated for MMI in 10-12 weeks. She will benefit from the following adjunct therapies/supplementation, MLS cold laser (BioResearch, Inc.), deflame diet, medication regimen, nasal spray, and prolo therapy injections. Her prognosis is good.
Nasal pillows or dilators are necessary when the patient has nasal valve compromise or collapse, as Diane’s CBCT revealed.
She was directed to use Xlear nasal spray (Xlear, American Fork, UT) before bed for her nasal blockage. Nasal spray is necessary to shrink soft tissue swelling in the nose and increase flowrate. A recent study found a 20% increase in volume (which can have up to a four-fold increase in flowrate) using hyperosmotic saline and Xylitol.11
The appliance was delivered, and the patient was evaluated weekly. MLS laser therapy was performed to decrease inflammation and accelerate healing (can also reduce orthodontic treatment time by increasing tooth movement).12,13,14,15 At four weeks a sleep study was performed. It consisted of three nights utilizing HST (home sleep testing), as ordered by the sleep physician. The results were: Night 1 – AHI 2.5, nadir oxygen desaturation 91%, diagnosis = Hypersomnia. Night 2 – AHI 4.2, nadir oxygen desaturation 90%, diagnosis = Hypersomnia. Night 3 – AHI 1.8, nadir oxygen desaturation 89%. Patients are often told that they do not have apnea with these results; however, that is inaccurate. The patient has upper airway resistance syndrome (UARS). This does not take into account unhealthy meals (high in sugar or saturated fat, low in fiber), that both worsen RDI.16
The patient was treated for 12 weeks of laser treatment and decompression appliance therapy. Re-evaluation diagnostics revealed a reduction of joint pathology (noises) from 38 Hz left and 14.5 Hz right to 5.3 and 4.5 Hz respectively utilizing JVA (Figure 11).
The patient was asked to quantify reduction of her chief complaints and stated that they had plateaued at 30% reduction of mandibular deflection on speaking and jaw joint noises at 40%. This demonstrates the value of the subjective evaluation of the patient and an objective measurement of the TMJ function, which showed a return to normal function in relation to noises.
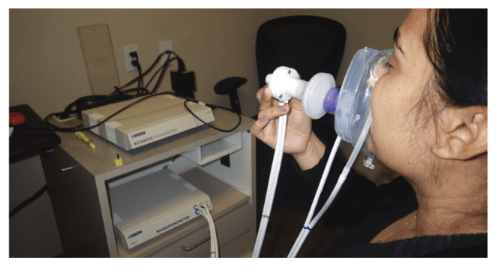
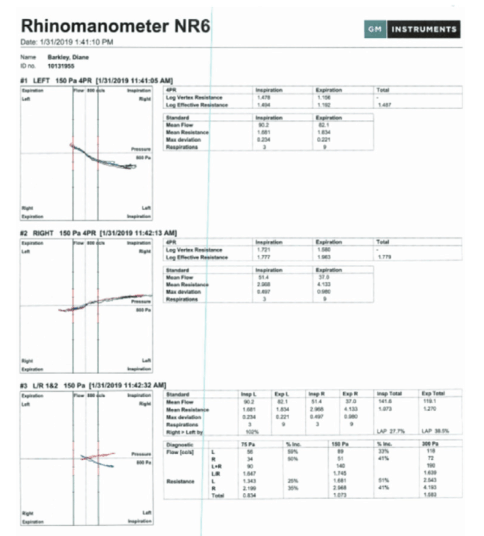
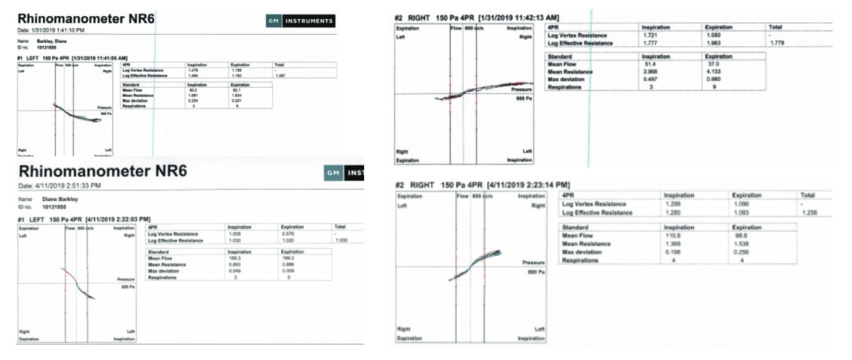
I explained to Diane that her remaining symptom of jaw deflection was secondary to nasal obstruction (mouth breathing). This is a muscle problem and not a TM joint problem. I demonstrated by spraying her nose and inserting nasal dilators that it corrected the deviation. She needed surgery to improve nasal function and airflow. It is always difficult to know how much of the obstruction we see on CBCT imaging makes a clinical difference in patient symptoms. Rhinomanometry (GM Instruments, BioResearch) measures flowrate as opposed to rhinometry, which measures volume.17 Rhinometry is helpful in discerning where the most narrow portion of the nasal airway is for triaging treatment options (sprays or surgery).18 Anterior rhinomanometry and acoustic rhinomanometry are probably the most common methods of clinical measurement of airflow.19
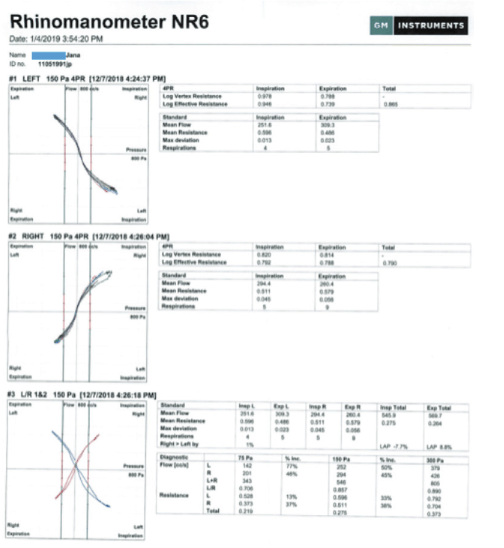
An example of proper airflow is shown in Figure 13 showing the contoured line in the green for both left and right valves.
Diane’s presurgical readings (1/31/2019) are shown with almost horizontal flow demonstrating severe obstruction (Figure 14). Post nasal surgery (4/11/2019) demonstrates improvement, showing a comparison of left and right flowrates however still below normal levels (Figures 15 and 16).

The clinical result was that she was left with a noticeable movement of the mandible to the right upon speaking. Most ENT surgeons perform surgery for the 2, 3, and 4 airway zones identified in the saggital head drawing (nasopharynx, velopharynx, oropharynx). They rarely perform surgery for the first point of entry: the nasal valve. A new surgical technique that is very easy to perform is Vivaer (Aerin Medical). It is an internal recontouring of the nasal valve by radiofrequency and pressure. It can be completed in the ENT office with local anesthetic. Demonstrating that the deviance of her mandible was the result of the nasal valve was demonstrated by nasal dilators (Figures 17 and 18). Video of speech (without and with nasal valve dilation), and the freeze frame of recorded speech with deviation and without using nasal dilation. Note the rotation (yaw) and medial lateral cant (roll). In these two-dimensional pictures it is not possible to demonstrate the third-dimension distortion anterior posterior cant (pitch).
Rhinometry and Rhinomanometry were necessary to show the ENT a reason to schedule for revision surgery for the nasal valve and resolve her speaking deviance. Use of the nasal dilators helped connect the measurements with clinical outcome for Diane. She is scheduled for Vivaer procedure.

