by Samuel E. Cress, DDS

Patients who have obstructive sleep apnea (OSA) not only suffer from comorbidities such as hypertension and cardiovascular disease but also from occlusal disease. Occlusal disease is sometimes called the “silent” oral disease that many people, including dentists, overlook. Often dismissed as natural aging or wearing of the detention, it is the overworking of a pathological bite to protect the airway. If left uncontrolled, it can cause tooth damage, gum and bone loss, failing restorative work, fatigued muscles of mastication, and damage to the temporomandibular joints.
The extra muscle activity in patients with OSA is a result of the brain telling the jaws to protect the airway at any cost, sacrificing the detention. I like to use the analogy that if I were to place a plastic bag over your head, tie it around your neck and push you into a swimming pool, your sympathetic nervous system would kick on and you would use your feet to push off the bottom of the pool, get above the water, and rip off the bag to breathe. OSA patients do the same thing when the airway is compromised and SpO2 drops. Brains kick into high gear to protect the airway, overworking the pathological bite. You may have heard this process called “protective function.”
In one way or another we are all nighttime clinchers. Some are greater than others. We all have our teeth together at times during the night, for whatever reason, and we move our jaws back and forth in a “grinding motion,” searching for a position to optimize our airway and unleashing the “silent” oral disease. The most severely affected patients might do that with nearly every breath, overworking the pathological bite and creating a worn detention.
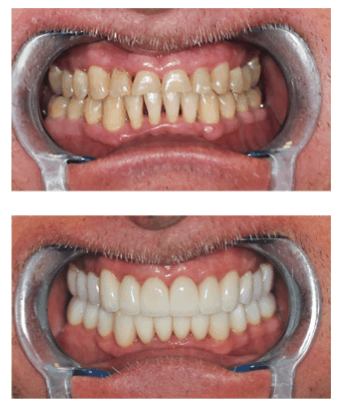
Why is educating yourself about OSA so important in restorative dentistry? This comprehensive approach is called “airway conscious dentistry.” Before restorative work begins, especially on patients that need several crowns, implants or bridges, elevate your standard of care and screen for OSA. If you have patients that are constantly breaking dental restorations, look to their airway. If the patient is diagnosed with OSA and is being treated with CPAP or an oral appliance like the Meridian PM, the predictability and success rate of dental restorations has increased tenfold. If you are planning a full mouth rehabilitation, consider whether airway is one of the reasons they need this extensive treatment. Planning treatment to affect the airway by opening the vertical and stabilizing a pathological bite will increase success. Pre- and post-sleep studies will illustrate the airway improvement that takes place when all etiologies are considered before restorative dentistry is begun. This is the ultimate in comprehensive dentistry.
Correcting jaw position is a vital part of changing a pathological bite. Read “Why start there?” by Dr. Mayoor Patel to discover the path to better treatment effects.