
The “halcyon days” of CPAP
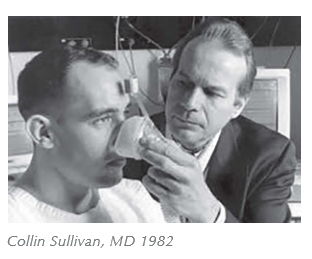
Thirty years ago, nasal continuous positive airway pressure (CPAP) became established as standard therapy for obstructive sleep apnea (OSA). At that time clinicians were faced with horribly sick, massively obese folks having extremely severe OSA. They died regularly and often required a tracheostomy. That all changed in 1982, when Sullivan discovered that air pressure applied to the nasal airway miraculously and immediately eliminated the problem. Suddenly, we could rescue these severely ill patients with simple air pressure. Our unbelievable amazement and relief cemented CPAP in our therapeutic armamentarium forever. And why not? We all thought it always works and never hurts, and it uses one of our favorite tools, air pressure.
 In the 1990’s we learned that OSA was prevalent in the general population. We began to encounter commonly apneics who, while overweight did not have “morbid” obesity. Lacking an alternative, CPAP became standard therapy for the burgeoning OSA population, even though some found it unacceptable, even barbaric. At the time, we believed that we were simply treating compromised quality of life, so whether or not the patient used CPAP represented his/her choice between improved quality of life and refusal to use awkward therapy. Our mantra was firmly established: “when in doubt, pressurize the snout”.
In the 1990’s we learned that OSA was prevalent in the general population. We began to encounter commonly apneics who, while overweight did not have “morbid” obesity. Lacking an alternative, CPAP became standard therapy for the burgeoning OSA population, even though some found it unacceptable, even barbaric. At the time, we believed that we were simply treating compromised quality of life, so whether or not the patient used CPAP represented his/her choice between improved quality of life and refusal to use awkward therapy. Our mantra was firmly established: “when in doubt, pressurize the snout”.
New knowledge disturbs our comfortable treatment paradigm
The arrival of new knowledge ten years ago changed everything. We learned that OSA presents a significant mortality risk. For instance, population studies indicated that severe OSA was associated with a 40% mortality risk in 15-20 years. This meant that OSA could no longer be viewed only as a problem that impaired quality of life. We were faced with the jarring reality that OSA was a chronic disease linked to cardiovascular consequences and having a mortality risk comparable to hypertension and diabetes.
The new reality implied that the clinician managing OSA would have to take a long-term view, focusing on compliance with therapy and health outcomes. Accordingly, poor adherence with CPAP therapy is now seen in a different light as the untreated patient may be at risk of serious co-morbid illness. At the same time, an alternative therapy with higher adherence emerged, oral appliance therapy (OAT). This viable therapeutic alternative raises the question: which is better for any particular patient, pressurizing the airway or protruding the mandible?
CPAP or OAT, which is better?
 Each of the two therapies has pros and cons. While benign and highly efficacious, CPAP is not an attractive therapy to many patients, and long-term compliance is low. OAT, while preferred and associated with higher compliance, is inconsistently efficacious, producing a satisfactory response in 50-75% of cases.
Each of the two therapies has pros and cons. While benign and highly efficacious, CPAP is not an attractive therapy to many patients, and long-term compliance is low. OAT, while preferred and associated with higher compliance, is inconsistently efficacious, producing a satisfactory response in 50-75% of cases.
Recent studies have shown that, when applied to unselected patients with OSA, the two therapies produce comparable outcomes. This suggests that the poor compliance of CPAP offsets the inconsistent efficacy of OAT. In other words, each treatment has a drawback, and these drawbacks offset each other in long-term treatment. So, apparently, it does not matter which treatment you pick; each is suboptimal, and the outcomes are equivalent.
But wait, that’s not the end of the story; unlike CPAP, the drawback with OAT is fixable. Imagine if we had the capability to select for OAT only those patients whom we know in advance will experience a successful therapeutic outcome. This would make OAT a highly efficacious therapy. Thus, OAT could be as efficacious as CPAP but would have better compliance. Thus, for patients who respond favorably to the therapy, OAT will result in better outcomes than CPAP.
Selecting patients for OAT
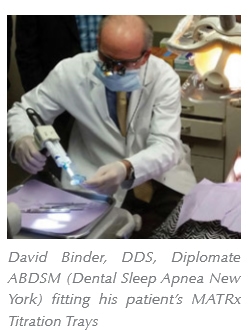 Attempts to prospectively identify OSA patients who will respond favorably to OAT using clinical features or pharyngeal imaging have proved disappointing. But, an encouraging development has recently occurred with the appearance of a test, called MATRx. This polysomnographically-based mandibular titration study prospectively identifies OAT responders and predicts an efficacious protrusive position of the mandible. Because of the high predictive accuracy, the physician and dentist can be completely confident that patients identified as favorable candidates will, in fact, experience elimination of OSA with OAT. As well, the dentist knows that the prescribed protrusive position will be adequate and probably less protrusive than that reached using the traditional trial-and-error adjustment of the appliance.
Attempts to prospectively identify OSA patients who will respond favorably to OAT using clinical features or pharyngeal imaging have proved disappointing. But, an encouraging development has recently occurred with the appearance of a test, called MATRx. This polysomnographically-based mandibular titration study prospectively identifies OAT responders and predicts an efficacious protrusive position of the mandible. Because of the high predictive accuracy, the physician and dentist can be completely confident that patients identified as favorable candidates will, in fact, experience elimination of OSA with OAT. As well, the dentist knows that the prescribed protrusive position will be adequate and probably less protrusive than that reached using the traditional trial-and-error adjustment of the appliance.
A more efficient and confident dentist
MATRx is the only prospectively validated method for selecting patients for OAT and determining an efficacious mandibular position. Together, these clinical predictions convey efficiency gains for the treating dentist. First, the dentist undertakes OAT with confidence knowing that the therapy will successfully eliminate OSA. Since the dentist never treats a patient who is a therapeutic failure, the number of visits per case is substantially reduced. Moreover, patient acceptance and adherence is greater. As well, because the dentist can expeditiously set the mandible at a minimal protrusive position that eliminates OSA, efficacious OAT is quickly established, a benefit both to the patient and the dentist. As one sleep medicine dentist put it: “Every MATRx case I do is a slam dunk”.
The next breakthrough – an in-home test
 And, there’s another breakthrough to come; Zephyr, the company that makes MATRx, has another breakthrough in the pipeline, one of particular importance for sleep medicine. The company is developing a home sleep test that employs a computer-controlled mandibular positioner. This test, like MATRx, identifies prospectively favorable candidates for OAT and determines a minimal protrusive position. The test apparatus can be dispensed from a dental office, a homecare provider, a sleep clinic or a general physician’s office and applied by the patient in the home. The data is automatically analyzed and provided to the physician and dentist. Early clinical trials show predictive accuracy comparable to that reported for MATRx.
And, there’s another breakthrough to come; Zephyr, the company that makes MATRx, has another breakthrough in the pipeline, one of particular importance for sleep medicine. The company is developing a home sleep test that employs a computer-controlled mandibular positioner. This test, like MATRx, identifies prospectively favorable candidates for OAT and determines a minimal protrusive position. The test apparatus can be dispensed from a dental office, a homecare provider, a sleep clinic or a general physician’s office and applied by the patient in the home. The data is automatically analyzed and provided to the physician and dentist. Early clinical trials show predictive accuracy comparable to that reported for MATRx.
So stay tuned. I believe that fantastic advances in sleep medicine are on the horizon. Patients with OSA will be provided therapeutic options, and for many, a simple oral appliance will be more effective therapy than pushing air.
Stay Relevant With Dental Sleep Practice
Join our email list for CE courses and webinars, articles and more..

