What is a functional oral appliance? How can we team support such therapies?
by Glennine Varga, AAS, RDA, CTA
Define and Educate
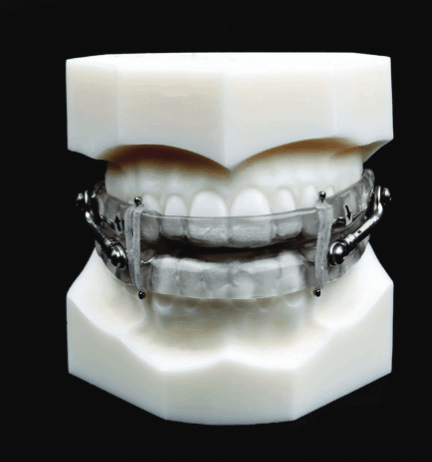
First, it’s important to define what a functional appliance is, and how the therapy fits within your practice. What is the difference between an occlusal guard and a functional oral appliance? The easiest way to understand this concept is an occlusal guard or night guard are fabricated to the patient’s habitual “everyday existing” bite – think of clenching, a ‘parafunctional’, or non-physiologic, movement or posture. The goal is to protect the structures from the excessive force and not allow changes, such as muscle pain or tooth wear. A functional oral appliance can be active, using normal movements like chewing, to use the muscle force with the intent to reposition the patient’s jaw, bite, teeth and muscles. Passive functional oral appliances include mandibular advancement devices for SRBD. This repositioning could be intended to be temporary or to make a more permanent change. Here are a couple of examples:
Functional Oral Appliance
- Oral device used to reduce
- upper airway collapsibility
- Orthopedic Expander
Non-Functional Oral Appliance
- Occlusal Guard
- Orthodontic Retainer
Oral appliances for sleep breathing disorders will reposition the mandible in a more forward position to support an open airway during sleep. This is a temporary change, which is why we supply our patients with morning exercises and aligners to recapture their habitual bite. However, an occlusal guard is fabricated to protect the teeth from dental forces during the night but not intended to anteriorly advance the mandible for airway patency and it is not considered a functional oral appliance. An orthopedic functional appliance will engage customized forces to change the shape and position of the bone which will change the position of the teeth, bite and muscles. However, an orthodontic retainer will hold the teeth in place to prevent a change in position therefore it also is not considered a functional oral appliance.
Functional oral appliances for adults can be used for sleep breathing difficulties, night time clenching and bruxing habits, temporomandibular disorders, orthodontic and orthopedic issues. Some athletes will also use a functional oral appliance during sports to reposition the mandible to gain the competitive edge similar to wearing nose strips or nose cones during sports. Functional oral appliances for children are geared toward making permanent orthopedic or orthodontic changes. Let’s take a look at team engagement with functional oral appliances and ways we can support it.
Evaluate and Plan
The responsibility of any dental team member is to understand the types of therapies provided and be able to answer simple questions regarding the necessity, procedure and outcomes. Team should keep all specifics up to their dentist to answer. However, once your patient commits to such therapies team responsibility becomes more involved in such actions as informed consent explanation, financial communications, medical insurance considerations, management of adjustments or use of appliance, documentation, home care instructions and promoting patient success. It is also important to know what the goal is for the treatment and document changes correctly. These processes can be completely different than what we are responsible for with dental procedures, but they can be very easily managed if you know what you should be saying.
Once you identify what types of functional appliance therapy your office offers, now it’s time to help identify which patients would benefit from such therapies. Updating your existing medical history has proven to be the most effective way to screen every patient for airway deficiencies, headaches, facial pain etc. This will allow for every patient to answer questions regarding symptoms and habits. Helping our doctors by working with your practice management systems to understand how to update these medical histories is the first step you can take. If you are offering a patient questionnaire focusing specifically on orthopedics, orthodontics, TMD or sleep breathing, work as a team to identify which patients should be introduced to this form. If possible, make it available on your website and include your office logo and contact information on any downloadable or printable form. You want your potential patients to have the opportunity to provide you with as much information as needed. When dealing with functional therapies there may be a medical component involved and obtaining a detailed medical history may be necessary for documentation. Taking measurements and documenting a changing position will require a new focus and level of awareness when it comes to the clinical aspects.
Evaluate what you’re offering your patients moving forward with therapy. Functional oral appliances may have insurance benefit, if there is documentation of a medical necessity. Always remember there may be a deductible to consider. Therefore, preparing for the financial discussion should be a priority. To be ready to discuss a benefit from medical insurance for your patients, be prepared by understating the insurance policy and requirements. Decide which financial arrangement will be discussed. Assemble a packet of contents including a financial contract, informed consent, copy of sleep reports, physician letters and educational materials. Include your office contact information.
Typically, functional appliance therapies require multiple adjustments, sometimes done by the patient. Make this process easy for them by providing a guide or a chart to follow. If the patient has an orthopedic device and is making adjustments at home, monitor and communicate with them often and celebrate his or her compliance. Ask them to take photos with their phone and email them to you for the chart – if they are receiving adjustments in the office take intra oral photos of the progress. Don’t forget to follow your HIPAA rules! Print home care instructions and sleep hygiene tips. These are all items that do not cost much but can go a long way with your patient and are easy to produce.
Promote, Promote, Promote!

Most dental offices offering airway therapies know it’s rough at first to shift from primary dental conversations to sleep breathing or head and facial pain. Patients expect to talk about decay, periodontal disease and restorative dentistry – instead, we bring up oxygen desaturation, apnea hypopnea scores and medical related conditions. It can be a lot to take in. So where do we start? Getting to know your patient is always best and personalize everything. Be specific with note taking and relaying information to each other. Find your best patient successes and ask for permission to share. Don’t forget to document their consent! You can get your first stories from your internal circle: teammates, bed partners, children, parents, brothers, sisters, uncles, aunts. It pays to treat a loved one at risk and experience benefits first hand. In my 13 years of assisting in a TMD, sleep breathing, functional orthopedic practice I can tell you it was the patient success stories and internal referrals that made the biggest impact. Specifically orthopedic cases showing before and after changes and improvements convinced parents and patients to commit to functional therapies.
A sleep appliance for diagnosed sleep breathing disorders in my opinion is the easiest to influence patients to manage. When our patients are diagnosed with a sleep breathing disorder such as UARS, OSA or snoring, it is imperative we team communicate the importance of managing this and testify to other patient’s benefits. This promotion doesn’t have to be about the device, and, in fact, it should be much more about how we care significantly about our patients and their health aliments including damaging forces manifesting within their dentition. Helping patients breathe better during sleep with fabricated oral appliances will also protect dentition as a bonus. Helping patients orthopedically change bony structures to optimize function and airway support can also improve aesthetics – another bonus they can see and feel.
Glennine Varga enjoys showing clinicians other technologies besides functional oral appliances to boost their practices. Check out “The Use of Technology in a dental sleep practice,” here.