Drs. Preetam Schramm, Jason Hui, Pollyana Moura, Zohre German, Ju Ying Lin, William Stenberg, and Emet Schneiderman discuss sleep-disordered breathing and its impact, especially with medications and sleep issues.

by Drs. Preetam Schramm, Jason Hui, Pollyana Moura, Zohre German, Ju Ying Lin, William Stenberg, Emet Schneiderman
Background
The prevalence of Sleep Disordered Breathing (SDB) is well described and documented. Awareness of the disorder, its negative impact on health, and the financial burden it creates is growing globally. When SDB is viewed as a multisystem physiological disorder characterized by abnormal breathing during sleep that is often associated with repetitive upper-airway collapse, it is important to recognize that certain medications and the number of medications may have a direct impact on oral appliance therapy effectiveness. In mild forms, the SDB subtype, obstructive sleep apnea (OSA) manifests as snoring. Snoring is the most common form of SDB with about 37 million habitual snorers in the US population, almost 10%. More severe forms present as apneas, defined as an absence of breathing occurring for ≥10 seconds or hypopneas – shallow breathing associated with a 30% decrease in airflow for ≥10 seconds.1 Apneas and hypopneas are considered brain and cardiovascular stressors that are time-linked with blood oxygen desaturation (hypoxia), electroencephalogram arousals, hypercapnia, and increases in blood pressure, heart (tachycardia) and respiratory rate (tachypnea).
OSA involves several biological systems.3 Patients with OSA often present clinically with some or all of the following symptoms: daytime sleepiness, complaints of loud snoring, dry mouth on awakening, sexual dysfunction, forgetfulness and a concerned bedpartner. Frequently neglected during anamnesis for OSA are side effects from various medications addressing OSA-related symptoms and how they impact upper airway collapse during sleep. The research team led by Dr. Emet Schneiderman at Texas A&M University College of Dentistry (TAMUCOD) in Dallas, TX investigated this observation in a controlled trial in subjects randomly assigned to oral appliance only or oral appliance plus mouth shield. The results from their investigations suggest various medications and their number are highly relevant to dental sleep clinicians who provide upper airway management with oral appliance therapy.

Investigations into the Influence of Polypharmacy on Respiratory Dynamics during Sleep
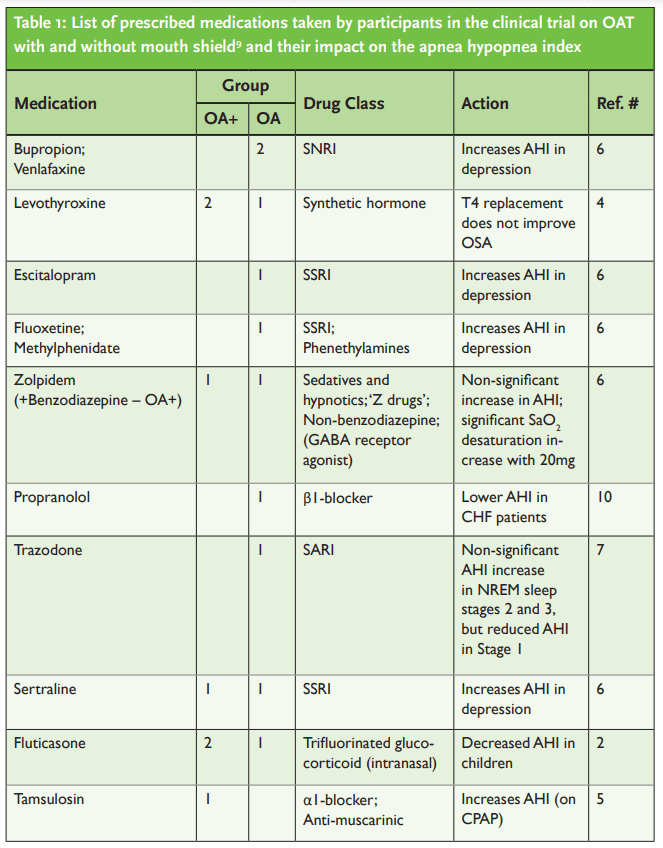
A recent publication from the team presented novel information on the influence of polypharmacy on respiratory dynamics during sleep among mild to severe OSA-mouth breathing patients receiving either oral appliance only or oral appliance plus mouth shield.9 The myTAP oral appliance (AMI, Dallas TX) that comes with a mouth shield was used in this study (Figure 1). The study results showed persistent apneas, hypopneas, snoring and mouth breathing occurred among medication users of commonly prescribed medications after 8-weeks of using either oral appliance intervention. The list of medications used among study participants are listed in Table 1. At 4-weeks, among non-medicated subjects, those using oral appliance plus mouth shield had significantly less oxygen desaturations compared with oral appliance only users. At 8-weeks of using either oral appliance intervention, the respiratory event index (REI; #apnea + hypopnea events/hour) was significantly higher in medication users (17.8 [9.7 – 25.7] events/h) compared with non-users (6.4[3.1 – 7.9] events/h, p = .027). While both medication and non-medication users showed reduction in the REI, the percent REI, mouth breathing and snoring reduction was significantly greater among non-medication users. Anti-depressants and opioids/opiates users of either intervention, had lower mean and minimum oxygen saturation percentages compared with non-medication users.

To ascertain if the above study’s observations were consistent, a retrospective analysis of a previous TAMUCOD study whose subjects alternatively used two different types of oral appliances,8 found that the REI was significantly lower in non-medicated compared with medicated subjects who were using 2 or 3 different medications. Negative correlations were found between the numbers of medications (1 – 3) and the mean and minimum oxygen saturation with oral appliance therapy (unpublished data).
Interdisciplinary Approaches to Bridge the Polypharmacy Influence on Airway Management Information Gap
Challenges remain to present this polypharmacy information, identified by dental sleep clinicians conducting airway management to medical physicians prescribing these medications. Interdisciplinary approaches need to focus on communication with the patient’s respiratory-sleep health as the primary focus. The use of Home Sleep Testing to generate an apnea hypopnea index (AHI), a now very familiar parameter, could be utilized by dental sleep clinicians to determine oral appliance treatment efficacy. The AHI metric can be used as a biomarker of sleep respiration ‘responsiveness’ relative to oral appliance effectiveness. Oral appliance advancement measures collected at 4-week intervals in association with AHI can provide clinically useful information in support of optimal advancement (i.e., AHI <5 events/h) or persistent residual AHI (>5 events/h) with polypharmacy.
Summary
Awareness of the number of medications and polypharmacy’s detrimental impact on the AHI and assessment of oral appliance efficacy under pharmacological conditions is the next logical phase to enhance our understanding of upper airway management, biomarkers, SDB phenotypes and comorbidities as well as assessment of oral appliance treatment efficacy. Tracking the pathophysiology along a continuum to determine biomarkers, oral appliance incremental advancement and symptom changes from baseline to clinical improvement is a reasonable approach. The use of temporary oral appliances fitted chairside such as the myTAP might provide the cost effective and testing solution to determine the effect on sleep quality. Furthermore, titration measures of oral appliances may provide thresholds to create categories that facilitate communication and clinical decision-making in patients with a history of snoring, mouth breathing and OSA.
- Berry, R.B., Budhiraja,R., Gottlieb,D.J., Gozal,D., Iber,C., Kapur,V.K.,et al. (2012). Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American academy of sleep medicine. J Clin Sleep Medicine. 8:597-619.
- Brouillette RT, Manoukian JJ, Ducharme FM, Oudjhane K, Earle LG, Ladan S, Morielli A. (2001) Efficacy of fluticasone nasal spray for pediatric obstructive sleep apnea. J Pediatr. 138(6):838-44.
- Lyons MM, Bhatt NY, Pack AI, Magalang UJ. (2020). Global burden of sleep-disordered breathing and its implications. Respirology. 25(7):690-702.
- Mickelson SA, Lian T, Rosenthal L. (1999) Thyroid testing and thyroid hormone replacement in patients with sleep disordered breathing. 78(10):768-71, 774-5.
- Moran M. (2016) Reversible exacerbation of obstructive sleep apnea by α1-adrenergic blockade with tamsulosin: A case report. Respir Med Case Rep. 14;19:181-186.
- Robillard R, Saad M, Ray RB, Bujaki B, Douglass, Lee EK, et al. (2016) Selective serotonin reuptake inhibitor use is associated with worse sleep-related breathing disturbances in individuals with depressive disorders and sleep complaints: a retrospective study. J Clin Sleep Med. 17(3):505–513.
- Smales ET, Edwards BA, Deyoung PN, McSharry DG, Wellman A, Velasquez A, et al. (2015) Trazodone Effects on Obstructive Sleep Apnea and Non-REM Arousal Threshold. Ann Am Thorac Soc. 12(5):758-64.
- Schneiderman E, Schramm P, Hui J, Wilson PD, Moura P, German Z, et al. (2021) Randomized Trial of 2 Self-Titrated Oral Appliances for Airway Management. J Dent Res. Feb;100(2):155-162.
- Schramm, P., Schneiderman, E., Hui, J., German, Z., Stenberg, W. and Lin, J.Y. (2024) Obstructive Sleep Apnea Mouth Breathing Phenotype Response to Combination Oral Appliance Therapy. Frontiers in Sleep, 3, p.1272726.
- Tamura A, Kawano Y, Naono S, Kotoku M, Kadota J. (2007) Relationship between beta-blocker treatment and the severity of central sleep apnea in chronic heart failure. Chest. 131(1):130-5.