
Obstructive sleep apnea (OSA) is a disorder characterized by repetitive collapse of the upper airway during sleep, with consequences of nocturnal hypoxemia and recurrent arousals from sleep.
The prevalence of OSA is significant and increasing with greater obesity and aging of populations. In addition to decreased neurocognitive performance from recurrent nocturnal arousals, there exists an increased risk of fatal and nonfatal cardiovascular events as well as all-cause mortality in patients with severe OSA. Recent evidence has demonstrated that the risk of cancer mortality and ischemic stroke carry a dose-response association with the severity of sleep-disordered breathing (SDB). The United States population of adults 65 years of age and older is to increase from 13.5 million in 1991 to 21.8 million by 2020 yielding a relative increase of 61%. Depending on the definition used for AHI 62% to 81% of this population will suffer from OSA. Endeshaw et al reported that the risk of OSA might increase as a result of edentulism.
 Full mouth extraction manifests a worsening of the cardiorespiratory symptoms, approximately doubling the number of episodes of apnea hypopnea per hour in a patient with OSA. Edentulism leads to a decrease in the size and tone of the pharyngeal musculature, which is a crucial risk factor for OSA.10 A loss in vertical dimension of occlusion leads to a reduction of the lower face height, counter- clockwise rotation of the mandible and may lead to OSA. Almeida et. al. commented, “There is no consensus in the literature about the impact of complete denture wear on OSA.”
Full mouth extraction manifests a worsening of the cardiorespiratory symptoms, approximately doubling the number of episodes of apnea hypopnea per hour in a patient with OSA. Edentulism leads to a decrease in the size and tone of the pharyngeal musculature, which is a crucial risk factor for OSA.10 A loss in vertical dimension of occlusion leads to a reduction of the lower face height, counter- clockwise rotation of the mandible and may lead to OSA. Almeida et. al. commented, “There is no consensus in the literature about the impact of complete denture wear on OSA.”
“Contrary to previous studies, we found that OSA patients may experience more apneic events if they sleep with their dentures in place. Specifically, in mild OSAS patients, the use of dentures substantially increases the AHI especially when in the supine position.”
Bone resorption in edentulous alveolar processes has been studied extensively. It is a chronic, progressive and irreversible process that occurs in all patients. In complete denture wearers there is a greater degree of mandibular resorption than maxillary resorption. Atwood and Tallgren documented that mandibular bone loss is four times greater than maxillary bone loss. Irreversible loss of supporting bone structure results in the most common patient complaint, difficulties with retention and stability of mandibular dentures.
 After twenty years the complete denture patient experiences loss of the vertical dimension of occlusion as viewed from the right profile. The mandible rotates in a counterclockwise fashion leading to a increase in relative prognathism. Maxillary alveolus remained stable while the mandibular alveolus resorbed. Dentures rotated counterclockwise and shifted slightly forward. These observed changes were not significantly affected by the sex of the patient or by the denture technique employed.
After twenty years the complete denture patient experiences loss of the vertical dimension of occlusion as viewed from the right profile. The mandible rotates in a counterclockwise fashion leading to a increase in relative prognathism. Maxillary alveolus remained stable while the mandibular alveolus resorbed. Dentures rotated counterclockwise and shifted slightly forward. These observed changes were not significantly affected by the sex of the patient or by the denture technique employed.
Dental implants date back in history to 3000 B.C. Dental implants are now regarded as the “Standard of Care” for the edentulous mandible. “The panelists reached consensus that they would recommend an IRMOD (Implant Retained Mandibular Over Denture) instead of a CD (Complete Denture) as the first-choice standard of care for patients who are healthy or have mild systemic disease, but not for patients with severe systemic disease.”
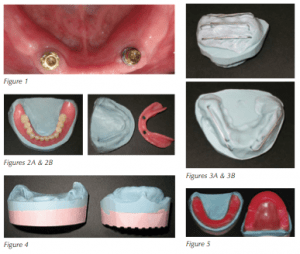
 (See Fig. 1)
(See Fig. 1)
Procedure
Treatment of the edentulous population suffering from OSA with PAP therapy can be challenging. The following is a technique developed by the author for treatment of the PAP intolerant edentulous patient with oral appliance therapy engaging two mandibular implants.
The complete dentures must be well fitting and in good repair. If the prosthesis is ill fitting or shows signs of excessive wear fabrication of a new prosthesis is indicated.
The first step is to duplicate the tissue- bearing surface of the existing prosthesis (maxillary and mandibular) with a silicone based putty such as Ivoclar Vivadent’s Sil-Tech® Condensation Silicone (Figs. 2A and 2B). This is preferred over taking new impressions that may lead to over extension of the oral appliance as well as saving time.
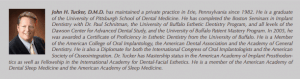
 The addition of paper clips to the underside of the silicone duplicate will provide a retentive mechanism for the addition of stone bases (Figs. 3A and 3B).
The addition of paper clips to the underside of the silicone duplicate will provide a retentive mechanism for the addition of stone bases (Figs. 3A and 3B).
Stone bases can now be added to the duplicate silicone models to provide stability for mounting to an articulation device (Fig. 4).
The duplicate silicone models are sent to the dental laboratory for fabrication of bite rims (Fig. 5).
Record the existing vertical dimension with the patients existing prosthesis in place. An eyebrow pencil can be used to mark a position on the nose and chin then recorded on a tongue depressor for future reference (Fig. 6).
 Seat maxillary bite rim and determine Fox Plane that mimics the patients existing complete maxillary denture (Fig. 7).
Seat maxillary bite rim and determine Fox Plane that mimics the patients existing complete maxillary denture (Fig. 7).
Seat mandibular bite rim and adjust accordingly to develop vertical dimension that replicates the patient’s vertical dimension with their complete dentures in place. The marked tongue depressor is used to verify the correct vertical relationship (Fig. 8).
The bite rims should mimic the existing prosthesis in all dimensions (Fig. 9).
A George Gauge 5.0mm bite fork was modified to accommodate the maxillary bite rim and secured with a VPS bite registration material (Figs. 10A and 10B).
The mandibular bite rim is modified to accept the incisal edge clamp of the George Gauge (Figs. 11A and 11B).
Determine maximum protrusive available and set George Gauge to correspond amount of protrusive desired. In this case 70% of maximum protrusive was used as the initial treatment position for the oral appliance (Figs. 12A and 12B).
Verify the protrusive bite position on the models prior to sending to the dental laboratory for fabrication of the oral appliance (Fig. 13).
The oral appliance is returned from the dental laboratory. The patient was treated using a SomnoDent appliance. The patient had two dental implants with Locator® attachments that provide retention of his complete mandibular denture. The Locator® attachments will also provide retention of his oral appliance (Fig. 14).
 The appliance is seated to verify that it fits passively over the Locator® attachments. The appliance is adjusted as indicated. (Figs. 15A and 15B)
The appliance is seated to verify that it fits passively over the Locator® attachments. The appliance is adjusted as indicated. (Figs. 15A and 15B)
The Locator® attachment housing can be transferred to the oral appliance directly in the mouth using cold cure acrylic or a BIS-GMA resin such as EZ PickUp™ available from Sterngold™ (Figs. 16A and 16B).
The Locator® attachment housings having been transferred to the oral appliance (Figs. 17A and 17B).
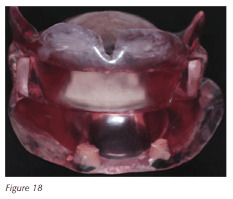
The completed oral appliance (Fig. 18).
Treatment Results and Comments:
Being an AADSM Accredited facility, I aspire to the AADSM Treatment Protocol. This involves a complete clinical examination, determination of current health of oral tissues and radiographic survey.
This patient was refereed for treatment of his OSA with Oral Appliance Therapy as a result of being intolerant to PAP therapy. His sleep physician provided a prescription for treatment. The diagnostic PSG revealed an AHI of 22.9/hour and Nadir SpO2 of 85%.
The patient was questioned during the initial consultation and examination as to why he was intolerant to PAP therapy. I believe it is important for the treating practitioner to investigate the reason(s) why the presenting patient is intolerant of PAP therapy to have an understanding of the patient’s attitude regarding treatment of their disease. I am of the mindset that we should reinforce the possibility of revisiting PAP therapy with the patient in the event the patient had a misunderstanding of their disease and treatment. A discussion as to Oral Appliance design, rational for Oral Appliance Therapy and treatment efficacy was completed with the patient. The informed consent was offered to the patient as well as the ability to ask any questions he may have regarding his treatment. Related treatment fees were also reviewed with the patient prior to treatment.
The patient reported that he had tried several nasal pillows and full-face masks. His primary complaint was instability of the nasal pillows and discomfort of the pre-maxilla. He also reported that full-face masks led to a feeling of claustrophobia. The patient was questioned as to his complete denture wearing status while attempting the various PAP therapies. He commented that he had tried all PAP therapies with and without complete dentures in place. “I feel more comfortable with my dentures in place but no matter what I tired I had pain under my nose or felt claustrophobic”, was his comment.
I reviewed with the patient the possibility of fabricating an Oral Appliance that would mimic his complete dentures with the mandibular component engaging the implants. The patient was also informed that I had patent pending status regarding Oral Appliance Therapy on implants to avoid any conflict of interest (COI). He stated that he understood the treatment process and COI. His comments were. “This is exciting to me.” “When can we get started?” The patient completed the informed consent. Treatment was initiated as per the protocol described in this article. The proposed treatment plan was documented appropriately and communicated to the patients sleep physician and primary care physician.
 After approximately three weeks the appliance was inserted using Pressure Indicating Paste ensuring a comfortable fit of the appliance. The patient was instructed to wear the appliance during sleep as well as hygiene of the appliance. All patient questions and concerns were answered to his satisfaction. “I like this appliance idea and think it is going to work for me” was his comment upon departing the office.
After approximately three weeks the appliance was inserted using Pressure Indicating Paste ensuring a comfortable fit of the appliance. The patient was instructed to wear the appliance during sleep as well as hygiene of the appliance. All patient questions and concerns were answered to his satisfaction. “I like this appliance idea and think it is going to work for me” was his comment upon departing the office.
The patient was contacted via phone 48 hours following delivery of his Oral Appliance to verify that he did not have a problem or questions regarding use of the appliance. The patient indicted that he did not have a problem wearing the appliance and did not have any questions. His comment was, “I love this thing and I think its working!”
The patient was seen two weeks post appliance insertion. The patient was asked subjective questions regarding his therapy. The questions with his responses are noted:
Do your wear your appliance when you sleep? Yes All the time? Yes
Does your appliance fall out? No
Has your snoring been reduced? Yes. “She says I don’t snore anymore.”
Are you less tired during wake time? Yes
Are you dreaming more? Yes
Do you have any jaw pain? No
Do you have any tooth pain? “I don’t have teeth.”
Based on the patients positive subjective answers I elected not to calibrate the appliance at this time. It is interesting to note that there was no report of tissue irritation or lack of retention by the patient. He was re-appointed for a six-week follow-up appointment and informed to contact the office should he have any discomfort or questions. Appropriate documentation was noted in the patients EMR (electronic medical record) and communicated to his appropriate health care providers.
Six-weeks following, the patient was once again asked the subjective questions regarding his therapy as previously noted. The only change noted was his comment that he seems to be “snoring a little” as per his wife. The appliance was calibrated by 1.0 mm forward advancement. Once again it is noted that there is no patient complaint of appliance discomfort. He was re-appointed for a six-week follow-up appointment and informed to contact the office should he have any discomfort or questions. Appropriate documentation was noted in the patients EMR and communicated to his appropriate health care providers.
After approximately four months of Oral Appliance Therapy and appropriate calibration based on his subjective comments he was re-evaluated with a PSG to document efficacy of treatment. The PSG with oral appliance therapy revealed an AHI of 4.6/hour and Nadir SpO2 of 90%.
It is my opinion that follow-up testing should be delayed for approximately four to six months post Oral Appliance delivery to allow the body to heal. It is interesting to note in a recent study by Hoyos et al “CPAP treatment increased IGF-1 levels after 12 weeks but not 6 weeks, with a further increase at 24 weeks. These findings indicate that CPAP improves specific components of the GH/IGF-1 axis by improvement in hypoxemia in middle-aged men with OSA in a time-dependent manner. Future research should incorporate these findings when investigating any time-dependent improvements into longer-term measures of cardiometabolic health, in the ever-increasing population of those with OSA.”18
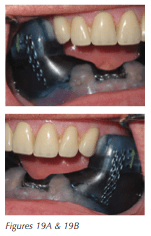
The technique and protocol described can be utilized with any type of Oral Appliance and any number of dental implants. The author has had experience in utilization of various appliance designs (Figs. 19A and 19B). My personal experience had led me to select appliance designs that do not rigidly connect the mandible to the maxilla. Appliances that rigidly connect the mandible to the maxilla have a tendency to un-seat the mandibular component from the attachments or dislodge the maxillary component. Careful selection of appliance design is indicated based on the above recommendation.
As was previously noted, treatment of the edentulous population with Oral Appliance Therapy can be challenging due to instability of the prosthesis as a result of bone loss. The addition of two mandibular implants is now considered to be the Standard of Care providing excellent retention of the complete mandibular denture during wakefulness. These implants can also provide retention of an Oral Appliance for the PAP intolerant edentulous population during sleep.
References:
- Malhotra A, White DP. Obstructive sleep apnea. Lancet 2002; 360:237–245.
- Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 1997;20:705–706.
- Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: An observational study. Lancet 2005;365:1046 1053
- Punjabi NM, Caffo BS, Goodwin JL, et al. Sleep-disordered breathing and Mortality: A prospective cohort study. PLoS Med 2009; 6:e1000132.
- Nieto FJ, Peppard PE, Young T, Finn L, Hla KM, Farre R. Sleep-disordered breathing And cancer mortality: Results from the Wisconsin sleep cohort study. Am J Respir Crit Care Med 2012;186:190–194.
- Douglass CW, Shih A, Ostry L (2002) Will there be a need for complete dentures in the united states in 2020? J Prosthet Dent 87:5–8
- Ancoli-Israel S, Kripke DF, Klauber MR, Mason WJ, Fell R, Kaplan O (1991) Sleep-disordered breathing in community dwelling elderly. Sleep 14:486–495
- Endeshaw YW, Katz S, Ouslander JG, Bliwise DL (2004) Association of denture use with sleep-disordered breathing among older adults. J Public Health Dent 64:181–183
- C. Bucca, A. Cicolin, L. Brussino et al., “Tooth loss and obstructive sleep apnoea,” Respiratory Research, vol. 7, article 8,2006.
- C. Bucca, S. Carossa, S. Pivetti, V. Gai, G. Rolla, and G. Preti, “Edentulism and worsening of obstructive sleep apnoea,” The Lancet, vol. 353, no. 9147, pp. 121–122, 1999.
- Almeida FR, Furuyama RJ, Chaccur DC, Lowe AA, Chen H, Bittencourt LR, Frigeiro ML, Tsuda H.Complete denture wear during sleep in elderly sleep apnea patients-a preliminary study.Sleep and Breathing September 2012, Volume 16, Issue 3, pp 855-863.
- Carlsson GE. Clinical morbidity and sequelae of treatment with complete dentures. J Prosthet Dent. 1998;79:17-23
- Atwood DA, Coy WA. Clinical, cephalometric, and densitometric study of reduction of residual ridges. J Prosthet Dent 1971;26:280-95
- Tallgren A. The continuing reduction of the residual alveolar ridges in complete denture wearers: a mixed-longitudinal study covering 25 years. J Prosthet Dent. 1972;27:120-32
- Douglass JB, Meader L, Kaplan A, Ellinger CW Cephalometric evaluation of the changes in patients wearing complete dentures: a 20-year study. J Prosthet Dent. 1993 Mar;;69(3):270-5.
- Ring M E. Pause for a moment in dental history: A thousand years of dental implants: A definitive history -Part 1. Compendium 1995;16:1060-1069.
- Kavitha P. Das, BDS, MPH, MS; Leila Jahangiri, BDS, DMD, MMSc; Ralph V. Katz, DMD, MPH, PhD. The first-choice standard of care for an edentulous mandible. JADA 2012;143(8):881-889.
- Hoyos CM; Killick R; Keenan DM; Baxter RC; Veldhuis JD; Liu PY. Continuous positive airway pressure increases pulsatile growth hormone secretion and circulating insulin-like growth factor-1 in a time-dependent manner in men with obstructive sleep apnea: a randomized sham-controlled study. SLEEP 2014;37(4):733-741.