 Introduction
Introduction
The Centers for Disease Control and Prevention (CDC) has stated that getting sufficient sleep is not a luxury – it is a necessity – and should be thought of as a “vital sign” of good health.1 This emphasizes the importance of sleep as an integral part of health and wellbeing, as sleep insufficiency is linked to motor vehicle accidents, industrial disasters, occupational errors and medical comorbidities, such as cardiovascular diseases, type 2 diabetes, depression and obesity as well as having reduced quality of life and increased mortality.2,3,4,5,6
Insomnia and Obstructive Sleep Apnea are the two most common sleep disorders
Now it is estimated that 12% of adults suffer from Obstructive Sleep Apnea (OSA) and that 80% of the patient population is undiagnosed.2,3 A recent European study found the prevalence in a middle-aged general population of 43.1% or 19% when looking at only moderate and severe OSA.7 Because of the potentially serious adverse consequences associated with untreated OSA, a prompt diagnosis and treatment is critical.2,3,5,8
 Even though insomnia and sleep disordered breathing have a different etiology, individuals complaining of insomnia, even if they report no classic sleep breathing symptoms, are commonly diagnosed to be co-morbid with sleep disordered breathing, sharply contrasting their subjective perceptions about their awakenings. Frequent arousals may be classified as insomnia when they could be due to OSA, and consequently many patients who are actually suffering from undiagnosed and untreated OSA could be misclassified as having sleep-maintenance insomnia.9,10,11
Even though insomnia and sleep disordered breathing have a different etiology, individuals complaining of insomnia, even if they report no classic sleep breathing symptoms, are commonly diagnosed to be co-morbid with sleep disordered breathing, sharply contrasting their subjective perceptions about their awakenings. Frequent arousals may be classified as insomnia when they could be due to OSA, and consequently many patients who are actually suffering from undiagnosed and untreated OSA could be misclassified as having sleep-maintenance insomnia.9,10,11
The role of dentistry in sleep medicine
The primary methods that have been used for clinical screening for sleep disorders have mostly been limited to subjective questionnaires. This may have been for the lack of a practical physiological measure, although convenience, the little effort involved, and low cost may have contributed to the wide acceptance of patient-reported risk factors. Questionnaires are based on respondents’ own subjective evaluation of their sleep rather than physiological data. Though undoubtedly subjective estimates are of importance in OSA patients, sleepiness and daytime functioning vary widely between patients, as some report excessive daytime sleepiness while others do not.7,12
Even though questionnaires have been validated, when compared to physiological measures, their results have shown to be inconsistent and unreliable. For sleep apnea, there are high false-negative rates for questionnaire responses, and it is likely that, when relied upon as the sole determinant, most of the questionnaires will miss a significant proportion of patients suffering from sleep apnea.13,14,15
As the etiology and treatment for insomnia and SDB are different, it is important for clinical practice to adopt objective tests that are based on direct analysis of physiology to aid in the process of accurately identifying sleep complaints before treatment is initiated. In order to make that practical, it is important that sleep medicine evolves to a multidisciplinary team approach.
Dentists have an opportunity to play a vital role to serve this underserved population by expanding their practice to include sleep disorder screening. Dentists probably have a better opportunity to look at their patients’ airway than most other clinicians, providing an opportunity to improve the patient health and quality of life and strengthen the relationship. Using an accurate, efficient screening method that collects objective physiological data offers an opportunity for an accurate sleep disorder-screening test and, after diagnosis, test again to help optimize the treatment through device titration.
Tools and technology
The SleepImage system (www.sleepimage.com) is an FDA cleared and CE marked tool to screen for sleep disorders, presented through a HIPAA compliant cloud computing system. The data is analyzed automatically, using patented algorithms called Cardiopulmonary Coupling (CPC) and Cyclic Variation of Heart Rate (CVHR). The results can easily be shared through the cloud with a sleep physician who the dentist has partnered with for further evaluation, recommendations, and therapy decisions. Although constant positive airway pressure (CPAP) has been termed as the primary therapy for OSA, many patients have shown a preference for the use of a mandibular advancement device (MAD).
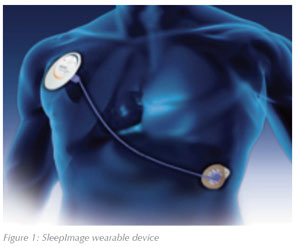
The SleepImage system is based on collecting single lead ECG data using a small wearable device that also includes a high precision 3-axis accelerometer to obtain actigraphy, snoring and body position (Figure 1). The data is automatically analyzed to measure sleep quality based on coupling Heart Rate Variability16 and electrocardiogram derived respiration (EDR), to provide an operator-independent measure of sleep to guide clinical decisions and therapy management. This low cost solution is an opportunity to foster patient relationships and expand the practice area at the same time.
The validation of the CardioPulmonary Coupling (CPC) and the cyclic variation of heart rate (CVHR) utilized clinical Polysomnography (PSG) recordings as the standard upon which it was compared.
Simultaneous SleepImage and PSG recordings were performed, validated and published. The data confirms that both systems were correlated as a valid clinical measure to identify the presence of sleep disorders (www.sleepimage.com/research).
While the CPC technology does not have a direct measure of SpO2 or generate an Apnea Hypopnea Index (AHI), it inherently presents information useful for clinical decision making to identify sleep disorders, whether for screening purposes or to track treatment efficacy.
Blood oxygen saturation levels are used as one of many measures of health. One association is with paused breathing is a reference point in apnea detection, but cannot be used to determine the presence or severity of apneas by itself, as it can drop for various health reasons not associated with apnea.
The AHI consists of counting events over a time period. To make the count as apnea, breathing must pause for at least 10 seconds and be associated with a decrease in blood oxygenation, so if breathing is paused for 9 seconds, it is not counted as apnea. Hypopnea is not considered clinically significant unless there is 30% (or greater) reduction in flow lasting for 10 seconds or more and when there is 4% (or greater) desaturation in O2 levels, or if it results in arousal or fragmentation of sleep. The reality is that it can consequently be quite random if an event is scored as apnea, hypopnea or is not considered “severe” or “long” enough to make either category. It is driven by a manual and, to some extent, subjective evaluation of each event.
The Sleep Apnea Indicator (SAI) on the other hand is based on a direct physiological measure of cardiovascular activity, looking for events of bradycardia followed by a sudden tachycardia at the end of an apnea event, a known condition based on cyclic variation of heart rate. There is no manually driven decision matrix to decide if the event is “severe” or “long” enough in seconds to make the count as it is not based on counting events.
The Autonomic Nervous System does not care if a person stops breathing for 9 or 10 seconds; the severity and strain caused by it negatively affects the person’s cardiovascular system. The SAI reports all activity as a percentage of the overall sleep period and is fully automated.
In summary the SAI presents events that are a reflection of the body’s physiological reaction to a drop in blood oxygenation. The parameters of the SleepImage system make it possible to identify sleep disordered breathing and differentiate between obstructive and non-obstructive sleep apnea.
Reimbursement
While use of the SleepImage system in a dental practice is not reimbursable, the cost of using it is very low and the value of the output is very meaningful. It provides an easy to understand report for the patient with metrics that are easy to track during therapy measured against the baseline screening test. For communicating with sleep physicians, the dentist can be very confident of recommendations given to the sleep physician based on the screening test, as it is an objective measure of physiology that has a very high correlation with PSG tests, yet it is not a test of parameters that are subject to the rules of sleep diagnostic tests that require a sleep physician to interpret the results. The system is fully automated and designed to provide operator-independent output that is intuitive for a multidisciplinary team approach. It is ideal to serve the vast populations of patients with undiagnosed and untreated sleep disorders by taking the “guessing” out of identifying patients who would benefit from a diagnostic assessment with a sleep physician.
Multidisciplinary team approach
The SleepImage system is an easy to use clinical solution. A multidisciplinary team approach starts with a screening test performed through the dental office, followed by a clinical diagnosis by a sleep physician on the team. Those patients who have untreated OSA are offered therapy choices and for many MAD therapy offered through the dental office is the therapy of choice. But it does not stop there, as a key to successful therapy is that it benefits the patient in subjective and objective improvements. Follow-up tests with therapy can be administered by the dental practice. These results can be shared over the cloud with the sleep physician on the team and the patient is much more likely to stay compliant on therapy if he/she feels the benefit of the therapy.
Workflow and metrics
The SleepImage system is operator-independent with metrics and workflow suggestions based on automatic analysis of ECG data collected during sleep. The primary metrics can be explained as follows:
- Sleep Quality Index (SQI) is a summary index of sleep duration, sleep stability and sleep pathology.17,18,19,20,21
- Sleep Apnea Indicator (SAI) is a measure of Cyclic Variation of Heart Rate (CVHR) detecting oscillations in cardiac intervals that are often associated with prolonged cycles of sleep
apnea. 22,23 - Stable sleep (HFC) is driven by the parasympathetic nervous system (Rest & Digest), dominated by integrated activity around individual respiratory cycles. Heart rate slows down and speeds up in synchrony with respiration. Characterized by stable breathing, high vagal tone and non-cyclic alternating pattern on the electroencephalogram, high delta power and blood pressure dipping, stable sleep may be considered to be “effective” NREM sleep. Effective sleep enables the normal functions of sleep, such as recovery and restoration processes.
- Unstable sleep (LFC) is driven by sympathetic nervous system (Fight & Flight), it is dominated by low frequency cycling of respiration and heart rate, with tidal volume fluctuations, cyclic variation in heart rate, a cyclic alternating pattern, electroencephalogram low delta power and stable (non-dipping) blood pressure. Unstable sleep may be considered “ineffective” NREM sleep, sleep that fails to accomplish the normal functions of healthy sleep.
- Using SQI together with SAI and biomarkers for sleep pathology called elevated Low Frequency Coupling broad-band (eLFCbb) and elevated Low Frequency Coupling narrow-band (eLFCnb), it is possible to identify the presence of SDB and categorize it as either obstructive or non-obstructive sleep apnea.17,18,19,20,21

The workflow to identify the presence of sleep disorders, using the SleepImage system can be demonstrated in Figure 2.
Clinical Example
The subject is a 57 year old male, BMI>35, with a history of daytime somnolence, snoring and waking up gasping or choking for air.
In addition to the above-mentioned metrics, the SleepImage system provides a spectrographic picture of the sleep parameters. A frontal view of the spectrogram presents the frequency ranges on the y axis and the sleep timeline on the x axis, while the 90° view presents a cross-sectional view of the frequency bands on the x axis and paints the peaks that are indicative of periodic breathing or non-obstructive sleep apnea as red peaks that tend to line up in a narrow band (eLFCnb), while obstructive sleep apnea footprint can be seen as white peaks that stretch across a broad frequency band (eLFCbb).

Metrics before treatment:
- SQI=31
- SAI=35
- eLFCbb=27%
- eLFCnb15%
- Snore count 1360
The frontal view of the spectrogram before treatment indicates a lack of Stable sleep (HFC) with long periods of Unstable sleep and both eLFCbb and eLFCnb (Figure 3).
The 90° view of the spectrogram before therapy further confirms that the patient is suffering from complex sleep apnea, narrow red colored peaks indicative of central events and the white peaks ranging across the frequency band indicative of obstructive sleep apnea events (Figure 5).
Metrics with treatment:
- SQI=49
- SAI=0
- eLFCbb=25%
- eLFCnb=0%
- Snore count 101.
The frontal view of the spectrogram with therapy displays slight improvements in Stable sleep (HFC), limited improvement in Unstable sleep, with eLFCbb still above and the SQI still below expected value indicative that there is room to optimize therapy with better titration of the device (Figure 4).



The 90° view spectrogram with therapy confirms that the central and obstructive component of the sleep apnea has been successfully treated, while there is still room to optimize the therapy by increasing stable sleep (Figure 5).
Conclusion
For this patient, although his sleep apnea has been treated to a degree of success (SAI and eLFCnb are both within expected values) his sleep quality and eLFCbb are still not within the expected values. This is a classic case of what research has shown to occur in more than 50% of sleep apnea therapy cases, namely that the patients stop using the therapy as they are is not feeling the benefit.
This is an opportunity for dental practices that see their patients on a regular basis for check-up and cleaning services to add sleep quality tests that can build a lasting relationship of happier and healthier patients. These tests will:
- Identify the presence of sleep disorders for patients who have not been previously diagnosed using a simple test that is objective and scientifically tested to motivate them to seek additional diagnoses and treatment.
- Help patients who are on MAD therapy for OSA optimize their treatment with regular device titration based on repeated sleep quality tests.

