 by Daniel Klauer, DDS, DABCP, DABCDSM
by Daniel Klauer, DDS, DABCP, DABCDSM
When evaluating patients with sleep disorders, it’s ok to be nosy. We have to be detectives, delving into the details of patients’ waking and sleeping hours. One of the most beneficial parts of my diagnostic exam involves evaluating the airway and the “Four Points of Obstruction” comprising the nasal valve, nasopharynx, velopharynx, and oropharynx.1 Literature illustrates the importance of proper nasal breathing as it relates to the success of oral appliance therapy.2 It makes sense to start our evaluation at the tip of the nose and evaluate those four points of obstruction. Research on oral appliance therapy for OSA cites that the two most important factors to success are body mass index (BMI) and nasal airway resistance.2 3D CBCT imaging is integral to viewing possible obstructions of the airway.
A CBCT scan can show the vital details of the hard and soft tissues of the nose including turbinate hypertrophy (inflammation of the soft tissue of the nose), any possible bony obstruction such as a deviated septum or septal spur. Chronic sinusitis and chronic nasal inflammation are also visible on a CBCT. The only other way to evaluate this completely is via nasal endoscopy; however, as dentists we are not trained for this procedure. After seeing a potential area of concern, I always recommend a consultation with a board-certified otolaryngologist (ear, nose and throat physician) who is adept at sleep breathing pathophysiology. I share my CBCT scans with these clinicians so that they, too, have full 3D information. Treating these patients depends heavily on collaboration with talented medical specialists.
The nose is the first line of defense for our immune system — it warms, moistens, and filters the air we breathe. Mouth breathers, who often have inadequate nasal airflow and lack adequate patency in that area, are breathing in cold, dry, dirty air. Studies show that mouth breathers get upwards of 20 percent less oxygen in their bodies and are essentially breathing dirty, unhumidified air.
Additional literature shows that patients with nasal congestion are 1.8 times more likely to have moderate to severe OSA compared to those without symptomatic congestion.3, 4, 5, 6
Case study
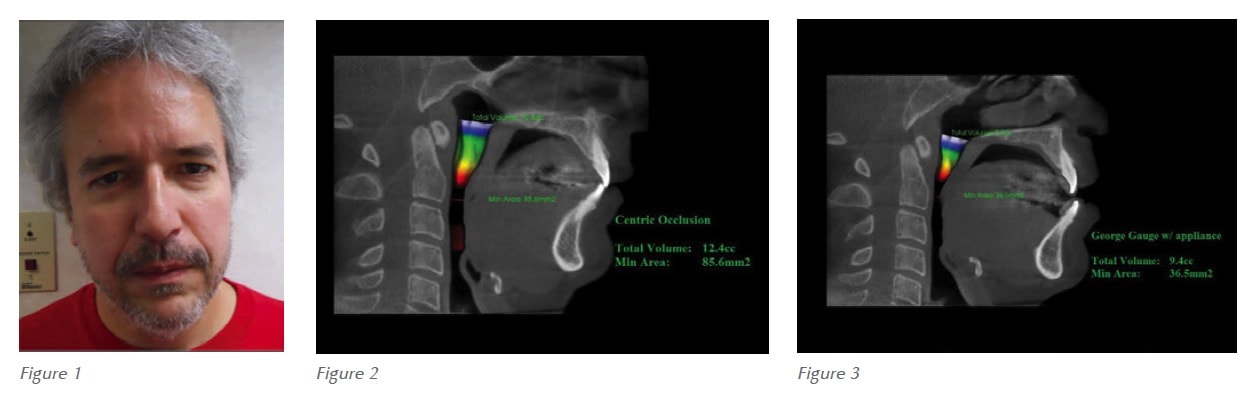
 The case study of a patient named Bill clearly demonstrates how nasal surgery and appliance therapy can help patients breathe and sleep more easily. Bill arrived at my office with several complaints: Frequent, heavy snoring; feeling unrefreshed in the morning; difficulty falling asleep; general fatigue; and excessive daytime drowsiness (Figure 1). His wife had moved out of their bedroom because Bill was frequently tossing and turning and grinding his teeth during the night. He had a pre-treatment AHI of 36.9 and had declined CPAP therapy.
The case study of a patient named Bill clearly demonstrates how nasal surgery and appliance therapy can help patients breathe and sleep more easily. Bill arrived at my office with several complaints: Frequent, heavy snoring; feeling unrefreshed in the morning; difficulty falling asleep; general fatigue; and excessive daytime drowsiness (Figure 1). His wife had moved out of their bedroom because Bill was frequently tossing and turning and grinding his teeth during the night. He had a pre-treatment AHI of 36.9 and had declined CPAP therapy.
After identifying nasal obstruction, Bill went to a board-certified ENT and Sleep Medicine Physician for Conservative Functional Nasal Surgery for a deviated septum repair with balloon sinuplasty. We fabricated an oral appliance utilizing a George Gauge, which is the industry standard for taking a protrusive construction bite for sleep apnea appliances. Currently, I am not aware of any literature to support the efficacy of utilizing a George Gauge.
After some time, this therapy proved to not be very effective for Bill, so I fabricated a new oral appliance utilizing a peer-reviewed published bite registration technique. This new appliance, that was clearly more effective for Bill, was fabricated using the Sibilant Phoneme registration protocol to prevent upper airway collapse.7 (See Figures 2-4.) The airway is not a garden hose; it’s 3 dimensional and collapsible, so in many cases, we don’t have to pull the jaw forward to prevent airway collapse. Since adapting the phonetic bite technique, I rarely titrate my oral appliance past an end-to-end anterior relationship. Subsequently, I do not encounter patients with jaw joint issues post-delivery of oral appliance. With a CBCT, we can see the position we have placed the patient in and subsequent changes utilizing the phonetic bite. Now we very well know the CBCT shows the patient’s airway in an upright and awake position. At the very least, we know the airway won’t be getting any better than this while sleeping. Utilizing a thoughtful bite registration technique for our patients allows us to achieve a great starting point with these patients. In order to fabricate efficacious and predictable oral appliances, the protocols I adhere to include the following:
Comprehensive Exam – utilizing i-CAT™ CBCT within Tx STUDIO™ software, Joint Vibration Analysis (BioResearch), Motor Nerve Reflex Evaluation (orthopedic reflex evaluation), and detailed intraoral and extraoral documentation (Figures 2-4).

 Acculator – all of my appliances are fabricated to a phonetic bite and mounted to HIP (Hamular Incisive Papilla Axis/Plane) on an Acculator (Figures 5-7).
Acculator – all of my appliances are fabricated to a phonetic bite and mounted to HIP (Hamular Incisive Papilla Axis/Plane) on an Acculator (Figures 5-7).
This helps ensure that the patients’ occlusal plane cant is taken into consideration so it is built to the patient’s anatomy, not on a bench top or to a facebow that assumes symmetry. Note the photo above to see how the right side requires far more material than the left side (Figures 7-8).

 Without an Acculator, this could not be predictively fabricated. There is no other way to line up asymmetries because most of our patients aren’t symmetrical. After surgery and receiving his oral appliance, Bill improved from severe apnea to within normal limits with a post treatment AHI of 4.5 (Figure 9).Bill is now walking 3 miles most days and is able to enjoy life. When he goes on vacations with his family, he no longer has to have his own hotel room. He is eager to speak with others about his successful treatment, and has even attended local community lectures to give live testimonials. He is more than a patient now; he is a friend to me and my team. It is with the knowledge that I have gained from patients such as Bill, together with collaboration with my skilled medical colleagues that has allowed me to build a full-time TM/Sleep practice in less than 12 months. I never thought I’d retire from general dentistry at the age of 29! Every patient is different and requires a comprehensive evaluation and walking through the four points of breathing obstructions. The best outcomes are achieved by being “nosy” about how our patients are breathing and making thoughtful referrals to collaborate with our talented colleagues. We cannot do this alone, and our patients deserve a collaborative approach to achieve optimal health.
Without an Acculator, this could not be predictively fabricated. There is no other way to line up asymmetries because most of our patients aren’t symmetrical. After surgery and receiving his oral appliance, Bill improved from severe apnea to within normal limits with a post treatment AHI of 4.5 (Figure 9).Bill is now walking 3 miles most days and is able to enjoy life. When he goes on vacations with his family, he no longer has to have his own hotel room. He is eager to speak with others about his successful treatment, and has even attended local community lectures to give live testimonials. He is more than a patient now; he is a friend to me and my team. It is with the knowledge that I have gained from patients such as Bill, together with collaboration with my skilled medical colleagues that has allowed me to build a full-time TM/Sleep practice in less than 12 months. I never thought I’d retire from general dentistry at the age of 29! Every patient is different and requires a comprehensive evaluation and walking through the four points of breathing obstructions. The best outcomes are achieved by being “nosy” about how our patients are breathing and making thoughtful referrals to collaborate with our talented colleagues. We cannot do this alone, and our patients deserve a collaborative approach to achieve optimal health.
Stay Relevant With Dental Sleep Practice
Join our email list for CE courses and webinars, articles and more..
