Dr. Zareth Jana Hernández talks about the debilitating pain of TMJ disorders, and how oral myofunctional therapy may help.
 by Zareth Jana Hernández, DMD
by Zareth Jana Hernández, DMD
Temporomandibular disorders (TMDs) are debilitating conditions that may cause pain, dysfunction, and impaired quality of life.1 TMD patients may present with dysfunctional breathing, chewing, and speech patterns. They may compensate by recruiting orofacial muscles that should not be activated to perform these essential stomatognathic functions, which turns this into a vicious cycle that potentiates pain and dysfunction.2-4 Non-invasive therapies reported in the literature to alleviate pain are self-care guidelines, orthotics, and laser therapy.5-7 In addition to reducing pain, healthcare providers should aim to improve dysfunction.
Myofunctional therapy (OMT) involves neurologic reeducation through daily exercises that assist in breathing, chewing, speech,8 and even facial expressions in a social context.9 Modifying dysfunctional muscle patterns associated with TMDs may be achieved due to the principle of neuroplasticity.
Myofunctional therapy has three main goals:
- The tongue should rest on the palate
- Lips together, teeth apart
- Primarily nasal breathe10
Collaboration with dentists, ENTs, and osteopaths, among other specialties, is often required for comprehensive diagnosis and treatment planning.
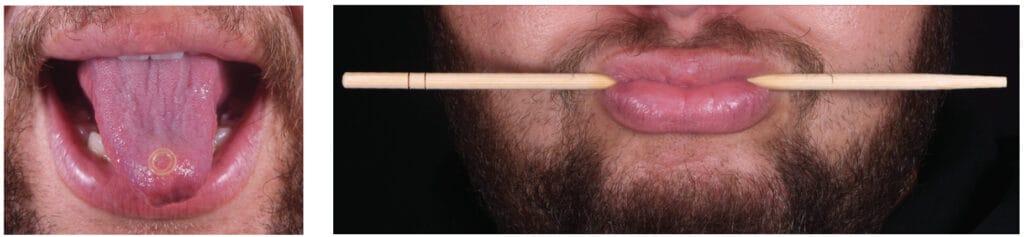
Figures 1-3 show examples of myofunctional exercises. During the first phase, myofunctional therapists may provide these and other exercises in weekly treatment sheets after thoroughly assessing orofacial functions.10

The role of OMT in improving health and quality of life cannot be emphasized enough. A recent international consensus statement reported that OMT should be considered an integral part of the interdisciplinary management of obstructive sleep apnea.11 Studies have found that OMT reduces the AHI by 50% in adults and 62% in children.12 Interestingly, the clinical and radiographic findings of TMD patients are often indistinguishable from those of airway patients.13

A systematic review that evaluated the evidence of OMT to manage TMD found a reduction in pain and dysfunction from baseline in symptomatic subjects that performed OMT. Results should be interpreted cautiously since the overall risk of bias was “High” and the certainty of the evidence for both outcomes was “Very low.”14 In this review, the primary outcome was pain which was measured subjectively via validated instruments,15 and the secondary outcome was dysfunction, measured with the validated Orofacial Myofunctional Evaluation with Scores (OMES) protocol.16
Most subjects were female (F= 92, M= 7) in all studies17-20 included in the review.14 The TMD diagnoses were made using the Research Diagnostic Criteria.21-22 Three-dimensional imaging was not reported in any of the studies for TMD diagnosis, which can be considered a limitation.23
Claudia María de Felício, a speech pathologist and myofunctional therapist from Brazil, developed an OMT protocol for TMD patients. The clinical trials included in the Jana et al. systematic review14 applied de Felício’s original or adapted protocol. Although this protocol is available, having the appropriate training is critical to individualizing the treatment exercises depending on the needs of each patient.8,17-20
The role of OMT in improving health and quality of life cannot be emphasized enough.
de Felício’s protocol is completed in 120 days. Patients receive a treatment sheet with exercises that change weekly during the first month and every two weeks afterward. Patients should be sitting with their backs straight while completing the exercises. They should also use a mirror for immediate feedback. The myofunctional therapist assesses compliance and reviews the exercises at each appointment.
In the first stage of de Felício’s protocol, mobility exercises are done in which oral structures are trained individually. Patients should slowly move the tongue and oral structures to maintain the target position for at least three seconds. The therapist decides on the number of repetitions based on the tonicity and fatigue limit of the orofacial muscles. After the mobility stage, strength and resistance exercises are implemented. Finally, coordination exercises are prescribed; in this phase, multiple orofacial muscles synchronize to assist stomatognathic functions.8
Take-home Message:
- OMT is a tool for healthcare providers to improve TMD patients’ pain and dysfunction.
- An OMT practitioner familiar with de Felício’s protocol would be a valuable member of the treatment team.
Karese Laguerre, RDH, delves into the benefits and challenges of incorporating myofunctional therapy into the dental practice in this CE. Subscribers can take the quiz and receive 2 CE credits! https://dentalsleeppractice.com/ce-articles/mastering-the-myo-merge-the-importance-and-essentials-in-implementation-in-the-dental-office/
- Hoffmann RG, Kotchen JM, Kotchen TA, Cowley T, Dasgupta M, Cowley Jr AW. Temporomandibular disorders and associated clinical comorbidities. The Clinical journal of pain. 2011 Mar 1;27(3):268-74.
- Rosa RR, Bueno MD, Migliorucci RR, Brasolotto AG, Genaro KF, Berretin-Felix G. Tongue function and swallowing in individuals with temporomandibular disorders. Journal of Applied Oral Science. 2020 Apr 3;28.
- Ferreira CL, Machado BC, Borges CG, Da Silva MA, Sforza C, De Felício CM. Impaired orofacial motor functions on chronic temporomandibular disorders. Journal of Electromyography and Kinesiology. 2014 Aug 1;24(4):565-71.
- Marim GC, Machado BC, Trawitzki LV, de Felício CM. Tongue strength, masticatory and swallowing dysfunction in patients with chronic temporomandibular disorder. Physiology & behavior. 2019 Oct 15;210:112616.
- de Freitas RF, Ferreira MA, Barbosa GA, Calderon PS. Counselling and self-management therapies for temporomandibular disorders: a systematic review. Journal of oral rehabilitation. 2013 Nov;40(11):864-74.
- Ebrahim S, Montoya L, Busse JW, Carrasco-Labra A, Guyatt GH, Medically Unexplained Syndromes Research Group. The effectiveness of splint therapy in patients with temporomandibular disorders: a systematic review and meta-analysis. The Journal of the American Dental Association. 2012 Aug 1;143(8):847-57.
- Maia ML, Bonjardim LR, Quintans JD, Ribeiro MA, Maia LG, Conti PC. Effect of low-level laser therapy on pain levels in patients with temporomandibular disorders: a systematic review. Journal of Applied Oral Science. 2012;20:594-602.
- Connelly S, Tartaglia G, Silva R., Oral Motor Treatment of TMD. In: de Felício CM, editor. Contemporary management of temporomandibular disorders. Springer International Publishing; 2019. p. 149-162.
- Kuć J, Szarejko KD, Gołȩbiewska M. Smiling, Yawning, Jaw Functional Limitations and Oral Behaviors With Respect to General Health Status in Patients With Temporomandibular Disorder—Myofascial Pain With Referral. Frontiers in Neurology. 2021:754.
- Academy of Orofacial Myofunctional Therapy. https://aomtinfo.org
- Mediano O, Mangado NG, Montserrat JM, Alonso-Álvarez ML, Almendros I, Alonso-Fernández A, Barbé F, Borsini E, Caballero-Eraso C, Cano-Pumarega I, de Carlos Villafranca F. Documento internacional de consenso sobre apnea obstructiva del sueño. Archivos de Bronconeumología. 2022 Jan 1;58(1):52-68.
- Camacho M, Certal V, Abdullatif J, Zaghi S, Ruoff CM, Capasso R, Kushida CA. Myofunctional therapy to treat obstructive sleep apnea: a systematic review and meta-analysis. Sleep. 2015 May 1;38(5):669-75.
- Rouse, J, McKee, J. Are we treating the same patient? The Blend of Airway and TMJ. SpearEducation. 04/17/2020. https://online.speareducation.com/course/are-we-treating-the-same-patient/lesson/are-we-treating-the-same-patient#_ga=2.130040207.1843449027.1677775272-1718351918.1677775272 Accessed: 01/02/2023.
- Jana Z, Blanco A, Elías A, López L. Efficacy of orofacial myofunctional therapy to manage pain and dysfunction in patients with temporomandibular disorders: a systematic review. (unpublished). 2023
- de Felício CM, de Oliveira Melchior M, Rodrigues Da Silva MA. Clinical validity of the protocol for multi-professional centers for the determination of signs and symptoms of temporomandibular disorders. Part II. CRANIO®. 2009 Jan 1;27(1):62-7.
- de Felício CM, Medeiros AP, de Oliveira Melchior M. Validity of the ‘protocol of orofacial myofunctional evaluation with scores’ for young and adult subjects. Journal of oral rehabilitation. 2012 Oct;39(10):744-53.
- Felício CM, Ferreira CLP. Protocol of orofacial myofunctional evaluation with scores. International Journal Pediatric Otorhinolaryngology 2008;7(3)367-375.
- de Felício CM, Melchior MD, da Silva MA. Effects of orofacial myofunctional therapy on temporomandibular disorders. CRANIO®. 2010 Oct 1;28(4):249-59.
- Machado BC, Mazzetto MO, Da Silva MA, de Felício CM. Effects of oral motor exercises and laser therapy on chronic temporomandibular disorders: a randomized study with follow-up. Lasers in medical science. 2016 Jul;31:945-54.
- de Felício CM, de Oliveira Melchior M, Lúcia Pimenta Ferreira C, Rodrigues Da Silva MA. Otologic symptoms of temporomandibular disorder and effect of orofacial myofunctional therapy. CRANIO®. 2008 Apr 1;26(2):118-25.
- Brandão RD, Mendes CM, Brandão Filho RA, De Sena EP. Isotonic exercises and relaxing techniques in individuals with temporomandibular dysfunction. CRANIO®. 2022 May 4;40(3):199-206.
- LeResche L, Von Korff M. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J craniomandib Disord. 1992;6(4):301-55.
- Schiffman E, Ohrbach R, Truelove E, Truelove E, Look J, Anderson G, Ceusters W, Smith B. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications.
- Schnabl D, Rottler AK, Schupp W, Boisserée W, Grunert I. CBCT and MRT imaging in patients clinically diagnosed with temporomandibular joint arthralgia. Heliyon. 2018 Jun 1;4(6):e00641.
 Zareth Jana Hernández, DMD, is a graduate of the University of Puerto Rico School of Dental Medicine and completed a 12-month Advanced Education in General Dentistry Postdoctoral Program with NYU Langone Hospitals’ affiliated institution in Puerto Rico. Dr. Jana trained in Orofacial Myofunctional Therapy with the Academy of Orofacial Myofunctional Therapy in 2020. She is in her senior year of Prosthodontics Residency at Puerto Rico’s Medical Sciences Campus. After residency, Dr. Jana will pursue further education in craniofacial development, airway, sleep, and TMD. She enjoys research, running, and spending time with her partner, Armando.
Zareth Jana Hernández, DMD, is a graduate of the University of Puerto Rico School of Dental Medicine and completed a 12-month Advanced Education in General Dentistry Postdoctoral Program with NYU Langone Hospitals’ affiliated institution in Puerto Rico. Dr. Jana trained in Orofacial Myofunctional Therapy with the Academy of Orofacial Myofunctional Therapy in 2020. She is in her senior year of Prosthodontics Residency at Puerto Rico’s Medical Sciences Campus. After residency, Dr. Jana will pursue further education in craniofacial development, airway, sleep, and TMD. She enjoys research, running, and spending time with her partner, Armando.


